File - Jessica Lafaele

NURS 360
PMH Care Plan
Student Nurse Reporting Form
SN: JESSICA LAFAELE Date: 02/22/2014
Pt.: Sex: FEMALE Age: 15 Date of Admission: 10/13/2013
Transferred? NO
Income source:
CLIENT RECIEVES HAWAII STATE MEDICAL BENEFITS
Legal Status : MH4
DSM Diagnosis
: Mood Disorder NOS h/o MDD w/psychotic symptoms PTSD & ADHD. R/o Bipolar versus Substance induced mood disorder, Borderline Personality Disorder
.
I – PTSD / ADHD/ BIPOLAR
_________________________________________________________________
II
– Mood Disorder NOS **
Depressive Disorder Not Otherwise Specified **
Client’s chart states client denies auditory and visual hallucinations but reports “I know they are still there.”
Client is hypomanic and silly although she is reporting depression and helplessness. Client has several suicide attempts and reports no enjoyment in anything.
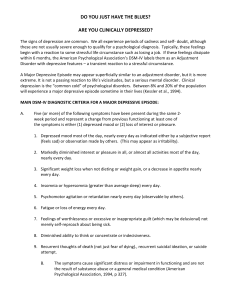
The Depressive Disorder Not Otherwise Specified category includes disorders with depressive features that do not meet the criteria for Major Depressive Disorder, Dysthymic Disorder, Adjustment Disorder with Depressed Mood, or Adjustment Disorder with Mixed Anxiety and Depressed Mood. Sometimes depressive symptoms can present as part of an Anxiety Disorder Not Otherwise Specified. Examples of Depressive Disorder Not Otherwise Specified include:
1.
Premenstrual dysphoric disorder : in most menstrual cycles during the past year, symptoms (e.g., markedly depressed mood, marked anxiety, marked affective lability, decreased interest in activities) regularly occurred during the last week of the luteal phase (and remitted within a few days of the onset of menses). These symptoms must be severe enough to markedly interfere with work, school, or usual activities and be entirely absent for at least 1 week postmenses.
2.
Minor depressive disorder : episodes of at least 2 weeks of depressive symptoms but with fewer than the five items required for Major Depressive Disorder.
3.
Recurrent brief depressive disorder : depressive episodes lasting from 2 days up to 2 weeks, occurring at least once a month for 12 months (not associated with the menstrual cycle).
4.
Postpsychotic depressive disorder of Schizophrenia : a Major Depressive Episode that occurs during the residual phase of Schizophrenia.
5.
A Major Depressive Episode superimposed on Delusional Disorder, Psychotic Disorder Not
Otherwise Specified, or the active phase of Schizophrenia .
6.
Situations in which the clinician has concluded that a depressive disorder is present but is unable to determine whether it is primary, due to a general medical condition, or substance induced.
http://www.medicalhomeportal.org/issue/depressive-disorders-dsm-iv-criteria#sthash.8ja5VP26.dpuf
1
III - None
IV -
Multiple psychiatric hospitalizations over last several years; multiple foster home placements.
V - GAF 30-21
Behavior is considerably influenced by delusions or hallucinations
OR serious impairment in communication or judgment (e.g., sometimes incoherent, acts grossly inappropriately, suicidal preoccupation)
OR inability to function in almost all areas (e.g., stays in bed all day; no job, home, or friends).
** (UTL in patient chart, but after assessing client I think she falls into this category while approaching the
31-40 category)
Some impairment in reality testing or communication (e.g., speech is at times illogical, obscure, or irrelevant)
OR major impairment in several areas, such as work or school, family relations, judgment, thinking, or mood (e.g., depressed man avoids friends, neglects family, and is unable to work; child frequently beats up younger children, is defiant at home, and is failing at school).
Global Assessment of Functioning (GAF) Scale ( From DSM-IV-TR, p. 34.)
What brought patient to the hospital?
Client tried to commit suicide via cutting while in her bedroom but was found by her foster father whom brought her to the emergency room.
P atient’s description of illness/issues:
Client suffered physical and emotional abuse from her parents. “I want to cut myself and slice my throat. I just want to die.”
Spirituality:
Client states, “I used to go church with my grandma.” Client chart states that she is
Christian.
Considerations r/t ethnicity or religion:
Religion: Client states that she is Christian. Client regularly participates in FTC Sunday spiritual classes.
Ethnicity – Client is Portuguese. Client states “I’m local Portuguese.”
Patient’s Strengths:
Client – “I know what I want. I’m not scared of anything.”
Per my observation – Client is helpful to staff and peers, appears to be social able but becomes withdrawn and highly emotional at times for no apparent reason.
2
Per Staff – Client is labile. Client can be cooperative and pleasant within FTC community then become impulsive and withdrawn at times.
Patient’s Limitations:
Client – “I just want to die sometimes.”
Per my observation – Patient’s affect is appropriate and exhibits no difficulty in speech or self expression but sometimes appears to become withdrawn.
Per Staff – Patient has no problem performing ADL’s and will let you know when she is not having a good day.
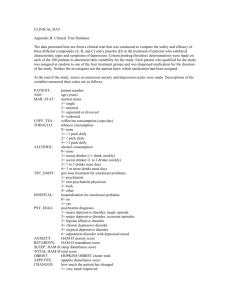
MEDICATION ORDER &
Route
CLASS 24HR
DOSE
S/E TARGET SX RANGE
Ibuprofen
Seroquel
Seroquel
Venlafaxine
XR
Q8H PRN
*PO
DAILY
*PO
BEDTIME
*PO w/Breakfast
*PO
NSAID
ANTIPSYCHOTIC 300mg
ANTIPSYCHOTIC 400mg
SSRI
800mg MI
STROKE
225mg
Depression
Dry Mouth
EPS sx
Drowsiness
Depression
Dry Mouth
EPS sx
Drowsiness
Anorexia
Constipation
Weight Gain
Serotonin
Syndrome
Pain
Inflammation
Psychotic
Disorders
Manic episodes in
Bipolar 1 DO
MDD
Anxiety
Panic DO
300 mg q.i.d., or 400, 600, or
800 mg t.i.d. or q.i.d. Range:
1.2 to 3.2 g daily.
300 mg once daily in evening.
Dosage increased daily in increments up to 300 mg, as needed.
Maximum: 800 mg daily.
300 mg once daily in evening on day
1, followed by
600 mg once daily in evening on day
2 and 200 to
400 mg b.i.d. on day 3 and thereafter.
Maintenance:
200 to 400 mg b.i.d
Maximum dose:
(moderately depressed outpatients):
225 mg/day
3
AXIS III: List all conditions even if they are not listed in multi-axial diagnoses or on chart. (Particularly note any unstable conditions & all non-medication interventions.)
1.
PMH of appendectomy – client chart shows no surgery date
BMI:
26.3
Category:
Over weight
(Height:
5’01”
Weight:
63.15kg/139#s
)
Sleep pattern:
Client states that she has a hard time falling asleep and is always getting up in the middle of the night.
Total sleep/24 hrs: Per client 6-7 hrs/night
(circle) Hypersomnia/Difficulty falling asleep/Middle insomnia/Early morning awakening
Number of hrs of disruption:
2+
Naps:
0 (per client / observation)
Lab & studies
** NO RESULTS FOUND PER CLIENT’S CHART DATED 01/25/204
DRUG/ETOH USE:
Cannabis use (10/14/2013)
MENTAL STATUS ASSESSMENT:
Behavior:
Calm, helpful, and appropriate w/peers and staff
Affect: euthymic full range (neutral mood)
Sensorium: no hallucinations, delusions, or suicidal ideations. Client states, “I’m ok.” Client is oriented to person, place and time.
Imagery:
Self harm scars, well nourished, uncombed hair, good hygiene
Cognition:
Attention/concentration= ok
Language = ok
Memory = ok
Interpersonal relationships: grandmother, siblings, therapists, medical staff, peers, case manager
Developmental level: (Assets & barriers)
Erikson’s Identity VS Confusion
Because of client’s extensive history of physical, emotional and psychological abuse she is having difficulty developing a sense of self and personal identity as defined by her diagnosis. Lack of role models has
4
contributed to client’s inability to trust and defy others while remaining insecure and confused about themselves and their future.
Client has a history of cannabis use but chart does not state last date of usage or frequency.
Problems Identified In Hospital’s Master Treatment Plan:
1.
Suicide precautions
2.
Safety
3.
Boundaries
4.
Structure
Current Discharge Plan:
Will continue Seroquel 100mg TID but hold off on Effexor for now. Client will be on suicide precautions.
Foster home placement
Nursing interventions you performed this shift (Include safety and teaching!):
Performed one on one therapeutic communication to establish trust and rapport.
Assessed client’s mental status and completed Assault & Violence risk assessment. Notified RN of results.
Encouraged client to express herself and importance of proper nutrition d/t lack of appetite side effects of medications. Discussed coping skills to deal with feelings of helplessness and unworthiness. Provided patient education in regards to alternate forms of expression such as coloring, music therapy, and guided imagery.
D: “I will control my impulse by filtering what I see so I am able to stay out of trouble and stay mellow.”
Client very attentive, helpful, and joined in discussions during goal setting.
A: One to One to establish trust and rapport while assessing client’s mental status. Client was praised when she expressed self in relations with others. Monitored client’s mood, affect, and safety.
R: Client joined peers during breakfast and completed all given tasks on time. Client helped staff and peers with “store” and stated “sometimes they need someone to remind them what things to buy, otherwise they just waste their credits on candy.”
5
Patient-centered Care Analysis
PRIORITIZED PATIENT NEEDS
What are the patient’s 4 highest needs/problems?
(Use your best nursing judgment! It will be different than the master treatment plan.)
1. P:
Safety
E:
Client says “I wanna just kill myself.”
S:
Assess for suicide risk, plan, availability of resources to commit act. Establish trust and rapport.
Encourage client to express herself. Report findings to primary nurse.
2. P:
Insomnia
E: Client says she has a hard time falling asleep. Client does not take daytime naps. Client appears lethargic and tired.
S:
Explored coping skills such as decreasing activity, not drinking caffeinated beverages, and relaxation techniques before sleep. Encourage client to eat healthy foods and stay away from sugary items before sleep.
3. P:
Reducing mistrust and anxiety r/t early life stressors. (see article attached)
E:
Client becomes easily agitated when talking about childhood experiences. Client said, “We were homeless one time. My mom moved us to Texas, to get away from my dad who abused us all, and had all these boyfriends” while she shook her head in dismay and avoided eye contact.
S:
Explored coping skills such as meditation, guided imagery, self expression and reminding client that none of these events was her fault.
4. P:
Hygiene
E:
Client’s hair was messy.
S:
Encouraged client to maintain grooming at all times to help build self confidence.
6
Priority # 1 CARE PLAN
Nursing Diagnosis: Risk for suicide and risk for self violence.
P: Safety
E: Client admitted to the ER for cutting herself on 10/13/2013.
S: Assess for plan, intent, and risk. Assess for physical factors that may foster violence such as physical discomfort, inability to cope with frustrating situations, helplessness.
LT goal: Client will not harm self or others while residing at Queens FTC.
ST goal: Client avoids self directed harm during my shift.
Establish trust and rapport at beginning of every shift to assess client for suicidal tendencies and risk factors such as expressions of low self esteem, noncompliance with treatment plan.
Intervention & Frequency
Scientific Rationale
(In complete sentences!)
(Reference in APA format, including page number)
Thorough assessment of precipitating factors is needed so preventive measures can be instituted.
Evaluation
Client did not experience any suicidal thoughts or tendencies throughout the shift. Client is cooperative and willingly participated in community goals.
Client’s chart shows that prescribes meds were taken. Administer prescription meds as prescribed. Medication may be indicated to decrease potential risk for injury.
Permit verbalization of feelings associated with agitation. Verbalization of feelings may diffuse aggressive behavior.
Client said, “I feel ok.”
Acknowledge normalcy of feelings related to being physically and emotionally abused.
Guilty about feelings and blaming of self can lead to self mutilation.
Client stated that she knows that she is not to blame for the abuse she experienced and will try not to focus on the good things in her life.
Reference
Gulanick,M. & Myers, J. (2011). Nursing care plans: diagnoses, interventions and outcomes.(7 th ed.) PA: Mosby.
7
8