MHFA+ - Administration, Monash University
advertisement

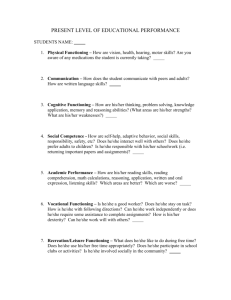
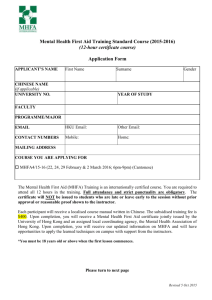
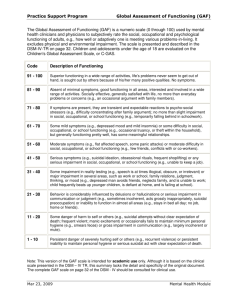
MHFA Sally Trembath Manager, Mental Health & Safer Community Programs Health Wellbeing & Development Aims of introducing Mental Health First Aid (MHFA) at Monash Reducing stigma associated with mental health Increasing mental health literacy and confidence in order to reduce anxiety when dealing with mental health issues Promoting pro-active and early intervention strategies Building capacity to respond in crisis situations Promoting culture of care and safer community Summary of Feedback Overall themes Change in attitude Change in behaviour Reducing stigma Early interventions Building capacity Improved communication Improved workplace outcomes Tracking these aims … Survey Monkey demographics Composition of staff Numbers n = 145 Academic Staff Numbers n = 146 Berwick 8 Caulfield 26 Clayton 83 Gippsland 16 Peninsula 12 Malaysia 1 South Africa 0 19 Professional Staff 79 Student 19 Monash Residential Services Campus 39 Changing attitude Since completing MHFA, do you believe you are: n = 141 Response percent Response count More able to recognise mental health problems 34.8% 49 More confident in offering help 39.7% 56 More inclined to actively engage with those effected by mental illness 25.5% 36 Changing attitude Since completing MHFA, what action(s) have you taken to assist someone? Listening non judgmentally n =122 Provided advice and reassurance n = 100 Called CAT team n=9 Educated someone about mental health n = 54 Feedback from respondents Reducing stigma & building capacity • Avoid engaging in mental debate with those having a mental health illness. • Increased awareness has helped boost my confidence and tips about how to communicate and respond have helped. • Very positive experience, will be useful in my role as a First Aid/Safety Officer and in my life outside of work. • I have changed my approach to people since the workshop. I am much more understanding of those with depression and anxiety. • Has given me practical advice for dealing with people who suffer from mental illness. Change in behaviour Q: Since completing MHFA, have you done anything differently to help others? 60 50 40 Family (n=45) Colleague (n=39) Student (n=61) Friend (n=59) 30 20 10 0 Assisting others post MHFA training (n = 119) Change in behaviour Q: Since completing MHFA, have you helped someone with: 90 80 Panic/Anxiety attack (n=40) Suicidal thoughts/ threats (n=25) Psychotic episode (n=7) Depression (n=94) 70 60 50 40 30 20 10 Threats to inflict self injury (n=10) 0 Specific interventions post MHFA training (n = 110) Change in behaviour Q: Since completing MHFA, what action(s) have you taken to assist someone? Listened non judgmentally (n=122) 140 120 Provided advice and reassurance (n=100) 100 Referred for professional help (n=63) Called CAT team (n=9) 80 60 40 20 0 Specific interventions post MHFA training (n=134) Consulted a university counsellor (n=36) Educated someone about mental health Feedback from respondents Early interventions, Improved communication & workplace outcomes • Helped to have strategies for dealing with panic attacks – I actually helped someone while they were having an attack. • I had to call a CAT team and I was more confident in dealing with them because of the training. • I dealt with a student suffering severe depression, including being suicidal and was able to convince them to see a professional. • A staff member was suffering an anxiety attack and after having attended the workshop I was able to suggest methods of getting them through the anxiety episode. • As a member of the Halls of Residence, I have found MHFA to be the single most beneficial professional development activity I have ever participated in. Q. Have you done anything differently to improve your own mental health? (n=145) 43% answered Yes Comments: • I exercised more, went to a doctor & psychologist • I’m far more mindful of negative mental behaviour on my behalf • I’ve seen a counsellor & improved my mental health • I make sure I get 30 mins exercise a day – usually walking my dogs • I sought assistance for depression whereas I wouldn’t want to admit it previously & the ultimate I’m keeping mood notes, more regular exercise, yoga & pilates, more time with friends & family, less workload, more time at home relaxing, gone on a short holiday interstate Reducing staff stress Testimonial I feel more able to deal with any unexpected mental health problems that I may be confronted with in my daily working with students. Coming to work in the morning is less stressful because I know that when there is a problem I will be able to help in a constructive and safe manner. I have recommended to my colleagues that they should attend the course as well. General concerns and recommendations… • MHFA is a fair introduction into mental health but it only scrapes the surface. I worry that it may make the trainees feel overly confident in dealing with people who have mental health issues that are not as mild as those portrayed in the training. • Very useful and I think all those dealing with students should attend this program. Further, it might be useful to run a refresher program (half day) each year for those who have done it. • Whilst MHFA is valuable, I have found getting management to understand and acknowledge things is the greatest challenge. … The failure to acknowledge changing situations and symptoms seems to be common and managers being older or more experienced overrides their willingness to listen to the advice of a mental health first aider. SOCIAL AND ACADEMIC FUNCTIONING (SAF) SCALE Adapted from Global Assessment of Functioning (GAF) Scale – DSM IV Score Level of Functioning Cognitive & academic functioning Social functioning Coping behaviours Psychological functioning Response & recommendation s 100 Superior functioning in a wide range of activities High achieving student Engaged in a range of activities Positive coping skills No symptoms, resilient, generally happy 90 Good functioning in all areas Good student Active socially, positive friendships, good network Good functioning overall Minimal symptoms, resilient, generally happy, may have some anxiety related to assessment tasks May benefit from opportunity to enhance stress management eg. counselling or group program. Provide information on available services and resources 80 Slight temporary impairment. Symptoms are short lived and understandabl e in the circumstances Capable student experiencing minor problems May have temporary setback due to challenge of unfamiliar academic task Occasional arguments or minor ups and downs in relationships Actively engaged in network May withdraw briefly Understandable stress reaction to difficult situations Returns to normal once situation resolved Brief period of understandable reactive low mood or irritability Short-term anxiety symptoms such as brief sleep disturbance Needs: Common sense support and problem solving. Peer support Advise: to talk to someone trusted and/or see a counsellor if no improvement after 2 weeks SOCIAL AND ACADEMIC FUNCTIONING (SAF) SCALE Adapted from Global Assessment of Functioning (GAF) Scale – DSM IV 70 Some mild symptoms or difficulty in social or academic functioning. Slightly diminished selfmanagement in some areas and may seem less organised Generally functioning adequately Academically related stress Some doubt about academic ability May become demanding of help or avoidant Some difficulties such as missing classes, late work Seeking extensions Concentration and focus may be affected in short term Some meaningful personal relationships May see others as critical and rejecting Some difficulties in usual social functioning, eg some avoidance of friends and activities. May be increased dependency on others Increased hours engaged on internet General functioning is reasonable Occasional irritability Maybe episodes of binge drinking May appear less organised May appear less cooperative than usual Stressed and negative in response to additional expectations Self critical, self doubt Pre-occupied or worrying Coping difficulties eg increased anxiety, irritability, avoidance May show disorganised patterns in eating, sleeping, attendance Moody Occasional loss of objectivity Guilt, anxiety about letting others down Needs: Supportive consultation with academic/facult y staff regarding difficulties and problem solving strategies Encourage: self care and accessing support Refer: counselling for positive coping strategies and how to get back on track Consult: counselling if problems continue SOCIAL AND ACADEMIC FUNCTIONING (SAF) SCALE Adapted from Global Assessment of Functioning (GAF) Scale – DSM IV 60 Moderate symptoms, moderate difficulty in social or academic functioning. May appear disorganised and unreliable. May be denying any problems and/or responsibility for difficult behaviour Unlikely that issues will resolve without intervention. Action required to prevent serious deterioration Impaired study ability due to reduced concentration and learning capacity Unable to prioritise tasks Difficulty meeting course requirements Stress of assessment period may result in concerning writing, drawing on exam papers Conflict in group assessment tasks Poor decision making Inconsistent behaviour All or nothing thinking Ruminating/circular worrying Few friends Conflict with peers May be withdrawn, Isolated Increased hours engaged on internet Behaviour may be having negative affect on others Others may express concern or make complaints Inappropriate sexual or provocative comments Generating targeted, harmful rumours Low level use of written, verbal or physical abuse eg pushing, shoving Concerning unwelcome relationship seeking Poor coping May be demanding of others to find solution Overall functioning compromised May be inappropriate emotional outpourings, eg tearful, aggressive outbursts, maybe hints of self injury Excessive coping through on-line chat and other internet activity Substance abuse Impulse control problems may lead to high risk behaviours eg unsafe sex, overspending, gambling Intentional theft Damage to property Threatening communications (nonviolent) Sleeping on campus Pornography use contravening Monash IT policy and/or affecting others Persistent complaining Unstable mood and emotion Mood swings, depression to manic May feel out of control Panic attacks May be eating disorder Sleep disturbance Self-medicating eg excess alcohol and/or other substances Addictive internet use Impaired judgement and decision making Impaired organisation and planning May appear chaotic Guilt and fear regarding poor performance, letting others down Thought sof escaping situation, possibly of suicide Non suicidal self injury Needs: Psychological assessment, intervention and additional support. Encourage: student to inform and enlist support of family and close others. Negotiate reduced academic expectations reducing academic stress to aid recovery. Refer: counselling, health service or GP. Medication may be indicated. Consult: counselling if not accepting help Where immediate threat call security ext 333 Where risk of harm to others consult community care on 9905 1599. A safety plan may be recommended SOCIAL AND ACADEMIC FUNCTIONING (SAF) SCALE Adapted from Global Assessment of Functioning (GAF) Scale – DSM IV 50 Serious impairment in a number of areas of functioning.May be avoiding reality of situation. May have high investment in staying a student and gaining degree.despite reduced capacity Issues will not resolve without intervention. Action required to prevent further serious deterioration Unable to focus on academic tasks eg in tutorials Missed classes and deadlines Confused, ineffective decision making and communication Concerning written, drawn material on exam papers No friendship group Unresolved conflicts interfere with daily functioning Others may express concern or make complaints Poor self- care in decisions regarding social group and activities Unresponsive to efforts to support Might be very demanding of others Isolated and withdrawn Overly dependent on friends Repeated episodes of physical aggression Physical attack Stalking behaviour Threats of violence and/or suicide Unwanted attention: physical, written, verbal Serious struggling If faced with seriousness of situation may become very demanding of solution or threaten self injury Likelihood of alcohol or other substance abuse, self-medicating non suicidal self injury Compromised selfcare Possibly eating disorder Compulsive behaviour eg hand washing, cleaning, use of pornography Obscene exposure Thoughts of suicide and may have plan and means Suicide attempt Feeling hopeless Ineffective problem solving Vulnerable and withdrawn Extreme emotional pain eg possibly severe eating problems Severe depression Impaired self control Excessive hours sleeping Unable to sleep Shame and guilt regarding perceived failure and letting others down Feelings may be masked by addictive behaviours such as excessive internet use, alcohol, drugs Needs : Assessment and treatment with psychiatrist, possible specialist forensic assessment. Reduced stressors so reduction or removal of academic expectations while recovering. Recommend: University Community Care-line and counselling services to be involved in developing a coordinated intervention to facilitate assessment and care of the person and safety of community. A behaviour contract may be recommended including informing parents should an emergency occur. If not accepting recommendations Statute 6.3 exclusion on health grounds may be indicated Inform: parents Action: consult community care-line or community care dropin on your campus for advice. Where immediate threat call security ext 333 SOCIAL AND ACADEMIC FUNCTIONING (SAF) SCALE Adapted from Global Assessment of Functioning (GAF) Scale – DSM IV 40 Major impairment in several areas of functioning May have high investment in staying a student and gaining degree.despite reduced capacity Significant impairment in reality testing and communication. Some bizarre behaviours Action required to prevent further serious deterioration 30 Delusional or impaired judgement. Inability to function in most areas May have high investment in staying a student and gaining degree.despite reduced capacity Action required to prevent further serious deterioration Failing Unable to attend classes Unable to meet deadlines Unable to put in consistent effort Communication problems Appears vague, not with it Not capable of making use of academic advice or help Unable to maintain relationships Poor self- care in decisions regarding social group and activities Hostile or irrational interactions Severe communication problems Unable to respond to support or guidance Others may express concern or make complaints Appears out of character Ongoing physical aggression and attacks Not attending class Unable to study Unable to manage timetable or academic requirements Unable to function as student No friends Withdrawn, isolated Unable to engage with others Unable to function as part of community Hostile or unpredictable engagement and communications Ongoing physical aggression and attacks Inconsistent adherence to treatment recommendations eg. medication Odd, bizarre behaviour Aggressive, defiant or withdrawn behaviours Presents as “dissociated”, cut off, disconnected Disorganised No routine May not be capable of using advice to prepare for appeals process Speech sometimes illogical, obscure or irrational May appear confused, disoriented Contact with reality unstable May show paranoid, bizarre thinking Depression and suicide plans and intent Needs: Psychiatric treatment. Reduced stressors including removal of academic expectations to facilitate recovery. Safety plan. Statute 6.3 is indicated to facilitate treatment if not responding to advice and recommendations. Assessment and treatment with psychiatrist essential to continue. Facilitate administrative tasks to enable re- enrolment if and when appropriate. Not adhering to treatment Behaviour is erratic and inappropriate May stay in bed all day Inability to function in almost all areas Homeless violent Suicidal preoccupation with plans and intent Delusional thinking in form of grandiose or paranoid themes Impaired judgement May appear despairing and cynical Needs: If not accepting treatment, implement assessment and treatment through Statute 6.3 Treatment and low stress for recovery. Support of family and close ones. Facilitate administrative tasks to enable re- enrolment if and when appropriate. Where immediate threat call security ext 333 SOCIAL AND ACADEMIC FUNCTIONING (SAF) SCALE Adapted from Global Assessment of Functioning (GAF) Scale – DSM IV 20 Danger of hurting self or others. Gross impairment in communication and interaction Not attending class Unable to function as student Friends and peers alienated, unable to understand the person, may feel afraid Unable to function as part of community Disorganised lack of boundaries Not adhering to treatment Largely incoherent Neglects basic self care, eg poor hygiene, poor diet Psychotic thinking: delusions and hallucinations Chaotic Suicide attempts Needs: Hospitalisation for assessment and treatment. Low stress for recovery. Support of family and close ones. Facilitate administrative tasks to enable reenrolment if and when appropriate. Where immediate threat call security ext 333 10 Persistent danger of severely hurting self or others Persistent inability to maintain hygiene. Serious suicidal act with clear expectation of death Unable to function as a student Unsafe Danger to self or others Unable to function independently Behaviour is unsafe Not adhering to treatment Suicidal or violent Unable to function independently Serious suicidal act with a clear expectation of death No attachment or concern for others Recurrent violence Needs: Hospitalisation, case management. Facilitate appropriate administrative tasks to enable reenrolment if and when appropriate Where immediate threat call security ext 333 INTRODUCING COMMUNITY CARE-LINE Community Care-line: 990 51599 Email: communitycare@adm.monash.edu.au Community Care-line is not an emergency response. For emergency response phone security on ext 333 Community Care-line is a new service providing a central point of enquiry by phone or email to Community Care staff who will provide advice and support for managing concerning or threatening behaviour and situations within the Monash University community. Students and staff are encouraged to ask for assistance if they: Feel threatened or unsafe Have concerns about someone else’s behaviour Are worried about someone harming themselves or someone else Wish to clarify issues of responsibility, confidentiality or duty of care INTRODUCING COMMUNITY CARE-LINE Community Care-line: 990 51599 Email: communitycare@adm.monash.edu.au The Co-ordinator Community Care programs will provide leadership and support at all stages of responding to complex and sensitive situations. At all times the welfare of both the individual and the Monash community will be considered and all recommended action will be in accordance with university statutes and policies. Community care drop-in times for your campus in HWD Berwick (Monday & Friday) 10.00-11.00am HWD Hub Bldg 930 Caufield (Wednesday) 9.00-9.30am HWD Hub Level 1 Bldg B Clayton (Daily) 9.00-9.30am HWD Hub Western end Campus Centre Gippsland (Monday) 10.30–11.30am HWD Hub Room 102 Bldg 3N Parkville (Monday) 10.00-10.30am HWD Hub Ground Floor, Sissons Bldg Peninsula (Tuesday & Thursday) 10.00-11.00am HWD Hub Level 1 Bldg A Future directions … • Tutor training • MHFA for students • Speakers on mental health issues during mental health week • Health Wellbeing & Development webpage MHFA@Monash