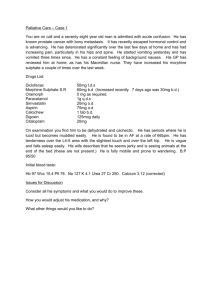
Practical symptom management for cancer and beyond
advertisement

Practical symptom management for cancer and beyond St Ann’s Hospice • Dr Catriona Barrett-Ayres • Speciality doctor Palliative Medicine • Dr Alison Phippen • Associate Specialist Palliative Medicine Palliative Care • • • • • • What is it? How is it relevant to you now? How is it relevant to you in the future? Practical applications for foundation jobs Quiz Questions Palliative care (from Latin palliare, to cloak) WHO Definition of Palliative Care “..an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.” Palliative care encompasses • holistic care of patients with advanced progressive illness. • Management of pain and other distressing symptoms through early identification and thorough assessments to promote comfort • psychological and emotional, social, spiritual support, care coordination and advance care planning (multidisciplinary approach) • achievement of the best quality of life for patients and their families. • Affirms life and regard dying as a normal process • Neither hastens or postpones death • Offers a support system to help patients and families cope during the patient’s illness and with their own bereavement • Strives for excellent communication with patients and families • Many aspects of palliative care are also applicable earlier in the course of the illness. How is palliative care provided? • Hospital advisory service (Macmillan nurses and specialist palliative care consultants) • Community-GP/ Macmillan nurses/ District nurses/ continuing health care • Nursing homes • Hospice inpatient • Outpatient services • Day care • Carer support through outpatients (NCCC) • • • • • • • • • • Symptom control Pain Nausea and vomiting Dry mouth Breathlessness Bowel obstruction Lymphoedema/ ascites Psychological support Bleeding Difficult wounds secretions What is pain? • .“an unpleasant sensory and emotional experience associated with actual or potential tissue damage” • “pain is a category of complex experiences, not a single sensation produced by a single stimulus.” • “pain is what the experiencing person says it is, existing whenever (s)he says it does.” PAIN • Assess what it is! Reverse anything reversible. • What is the aetiology? Does it need urgent investigation? • Is it new and therefore needs further investigation? Is it escalating? • What is the severity? • Visceral? • Neuropathic? • Bone pain? • Incident pain? PAIN in cancer patients • Pain associated with cancer often increases with progression of the disease. • 1/3 with cancer report pain, rising to 3/4 in the advanced stages of cancer. • Attempts to control pain and hence improve functional ability and quality of life have been overshadowed in the past by attempts to cure the underlying disease. • Several myths surrounding opiates make patients and Drs wary • Cancer pain has many dimensions including psychological, physical, social and spiritual which must be addressed in order to improve quality of life and functional ability Where to look for help • • • • • BNF or Palliative care formulary Symptom control guidelines St. Ann’s Hospice SIGN guidelines 2008 NICE guideline (in progress) If in doubt seek help/ advice from senior staff, Macmillan team WHO pain ladder Step 1 • Regular paracetamol • NSAID (remember can worsen renal function, bleeding risk) Step 2 • Codeine • Tramadol cocodamol can reduce tablet burden Remember side effectsconstipation/neuropsychiatric disturbance Step 3 • Morphine • Morphine type drugs may be used but this is more specialist and you should seek advice about these. • Oxycodone • Fentanyl • bupenorphine • hydromorphone • Alfentanil • Lozenges/ buccal/ intranasal/ subcutaneous Adjuvants • • • • • • • Amitriptyline Gabapentin Ketamine Methadone clonazepam Benzodiazepines Antidepressants Amitriptyline • • • • • • • Unlicenced for neuropathic pain Dose range for pain is 10-75mg TCA NNT=3 Comes as liquid preparation Dry mouth, presyncope can limit Helpful in sleep disorders, depression Gabapentin • Anticonvulsant • NNT=3 • eg 300mg TDS(can be increased gradually to 900mg tds) • Capsules can be opened • Dry mouth, movement disorder, tremor ataxia, dry mouth, drowsiness can limit • Reduce in renal failure Pregabalin is (an expensive) pro-drug. It is licenced for anxiety. It is indicated if other agents have failed or not been tolerated Opiates • • • • In use since 4th century Brompton cocktail – 1920’s Queen Victoria used laudanum Patients often think they mean euthanasia Opiate Problems •Problems- addiction/ tolerence ( 1000 opiate related deaths in England and Wales in 2004, 327,500 problem users in 2005) •Respiratory depression/OD } think trainspotting! •Withdrawal } • Recent death in media- opiate naïve patient given diamorphine high dose • Side effects- confusion, nausea, constipation • No set dose- metabolism and requirements differ Communicate • Explain possible side effects • Arrange frequent review of the patient to monitor progress and adjustments • Titrate up according to need, increase if ineffective, review if pain is sensitive • Reduce if toxicity • Write down/ look at prn doses • Involve carer Concurrent prescribing • Regular laxatives eg senna • Antiemetics for 1-2 weeks- eg metoclopramide (avoid if bowel obstruction/colic) • 30% started on opiates get nausea How to start morphine • • • • • Check opiates are appropriate-not in chronic pain. Is pain opiate sensitive? Are they at step 3 WHO ladder? Would a neuropathic agent be better? Opiate naïve? 2.5-5mg 4 hourly PRN oramorph . May need to be offered 4 hourly regularly plus PRN if pain is still problematic. • Convert total in 24h to Modified Release equivalent twice daily once dose established. • Breakthrough instant release dose is 1/6 total • Review every 48 hours and Increase according to extra PRN’s used but only by 30-50% total dose. Caution with rapid dose escalation Initiating Opiates • Already on step 2 weak opiates? – Codeine in 24h/10 to convert to morphine (eg 60mg qds=240mg/10= 24mg morphine= 10mg zomorph twice daily) – Tramadol in 24h/10 (eg 100mg qds= 400/10 = 40mg morphine ie 20mg zomorph twice daily) – Refer to symptom control guidelines/ conversion tables • Elderly/ renal failure? 1.25mg 4-6 hourly PRN oramorph. • Reduce the dose if toxicity occurs (30-50%) • Consider alternative opiate. Get advice. Opiate toxicity • • • • • • • • Drowsiness Pin point pupils Twitching (myoclonus) Hallucinations Nausea Slow cognition Confusion Respiratory depression- rr<8 omit, consider naloxone, seek advice Other things that may help • • • • • • • • • • Addressing total pain Antidepressants for low mood/ anxiety What does the pain mean? Which route of administration do they need? Interventional anaethsetic blocks Bisphosphonates Lignocaine plaster/ capsaisin cream Local heat or cooling Surgical intervention Complementary therapy Sore mouth • • • • • • • • Any triggers- recent chemoradiotherapy? Is it dry? Is the patient dehydrated? Do their dentures fit? Is it coated? Are they immunocompromised? diabetes etc Is there infection- viral, fungal or bacterial? Look for thrush and treat if present Dry mouth (xerostomia) • • • • • • • • • • • Tongue is dry and fissured Add gravy and sauces Saliva replacements – tablets, spray or gel Mints and sweets or gum(sugar free) Melon, avoid citrus Ice chips/ water/ frozen drinks (G&T!) Pilocarpine drops Do they have salivary reserve or not? Do they have their own teeth? Do they object to animal products? Is it iatrogenic? O2 or drugs Simple things can make a big difference to comfort Oral candida • • • • Treat with topical or systemic treatments Is there a short prognosis? Can they swallow? Are they on any medications that could interact with antifungals? • Do their dentures need to be treated? • In resistant cases consider a swab Treatments • Fluconazole 150mg stat dose • Fluconazole 50mg once daily for 1 week • Daktarin oral gel to mucous membranes and angles of mouth • Nystatin drops to tongue • Milton solution for dentures Rx stomatitis • • • • • • • Good dental hygiene Mouthwashes Coating agents Topical anaethetics Systemic anagesia IV fluids Nutritional drinks Coated Tongue Gentle Brushing Mouthwashes- chlorhexidine (dilute with water) Pineapple Chunks