Cancer Care Training: A Multidisciplinary Approach to Pain and
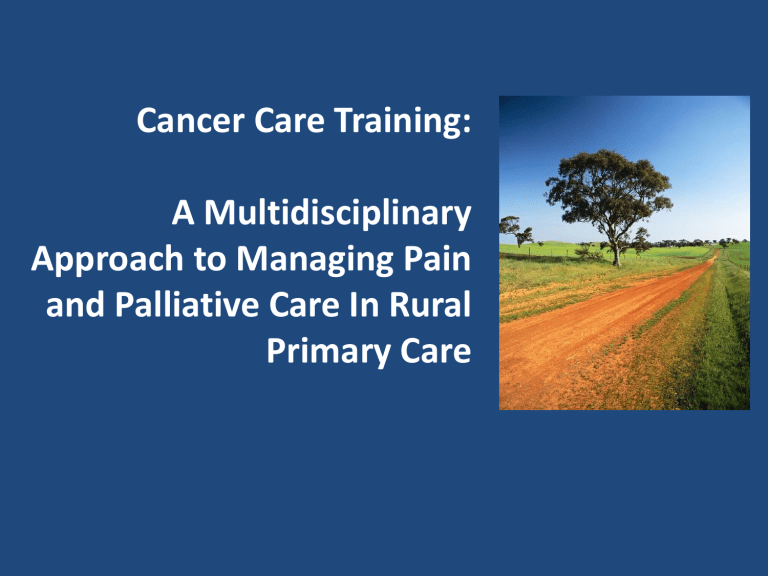
Cancer Care Training:
A Multidisciplinary
Approach to Managing Pain and Palliative Care In Rural
Primary Care
Program Partners
Kendra Siler-Marsiglio, PhD
Director
Mary Ann Burg, LCSW, PhD
Community Health & Family Medicine
Dawn Grinenko, MD
Community Health & Family Medicine
Merry Jennifer Markham, MD
Adult Medical Director, UF Cancer Survivor
Program
Gail Adorno, LCSW, MSW
Social Worker, UF Cancer Survivor Program
Susan Fleming
Cancer Program Administrator
Why this training, why now?
– Growing numbers of cancer survivors require cancer follow-up care and comprehensive health care
– Need to increase access for patients to these services in their home communities
– Need to increase capacity and skills of rural providers to care for persons with cancer histories
National Cancer Survival Rates
FIGURE 2-2 Five-year relative survival rates. SOURCE: NCI (2004c).
Cancer Incidence and Mortality in Rural North Florida
Rate of New Cancers 2002-2006 Rate of Cancer Deaths 2002-2006
Counties with mortality rates higher than state average:
Baker , Clay , Dixie, Hamilton, Levy, Madison, Marion, Putnam,
Suwannee, Taylor, Union. Putnam County has experienced a
RISING trend in cancer mortality:
Cancer Survivors By Site of Cancer
People With A Cancer History Are Everywhere
You Look…
Today’s Training Goals:
• Discuss the role of the multidisciplinary primary care team in cancer care;
• Define cancer-related palliative care
• Review best practices for screening and treating palliative care needs of rural patients with cancer histories in primary care settings
• Treatment, and then what?
• Fragmented care
• Body changes & unexpected symptoms
• Emotional rollercoaster
• Role changes
• Family stress
• Financial stress
What is the Cancer Experience?
Life “Before and After” Cancer
The Cancer Experience Can Also Be…
A new beginning:
• “post traumatic growth”
• improved wellness behavior
• improved health knowledge
• A cycle of new medical problems
• Cancer recurrences
• The beginning of the end
Patients Need Comprehensive Cancer Care:
• Anti-cancer therapy
• Supportive care
• Palliative care
• End-of-life care
• Bereavement care
Comprehensive cancer care is ALL care that occurs after a patient is diagnosed with cancer
Comprehensive Cancer Care Model
Palliative Care
Hospice Care
Palliative Care Is…
“ Patient and family-centered care that focuses upon effective management of pain and other distressing symptoms, while incorporating psychosocial and spiritual care according to patient/family needs, values, beliefs and culture(s).
The goal of palliative care is to prevent and relieve suffering and support the best quality of life for patients and their families, regardless of the stage of disease or need for other therapies.”
NCCN Practice Guidelines in Oncology – v.1.2010
Palliative Care Is Also…
• Relevant to any type of cancer
• Important at all stages of cancer care
• Care that can be combined with therapies aimed at remitting or curing cancer, or it may be the total focus of care
• Multidisciplinary: members of a palliative care team may include professionals from medicine, nursing, social work, chaplaincy, nutrition, rehabilitation, pharmacy and other professional disciplines
Caring for the Patient With A Cancer History in a
Primary Care Setting
• Assessment and treatment of acute and chronic health problems
• Health promotion
• Cancer screening
USUAL
CARE
PALLIATIVE
CARE
• Intervention for consequences of cancer and its treatment
• Coordination of care between specialists and negotiation of care
• Assisting patients through care transitions
(including hospice care)
Primary Care Is An Essential Site for Palliative Care
Primary
Care
Primary
Care
Cancer treatment
Cancer follow-up Care
Cancer recurrence
End-of-life care
Primary
Care
Primary
Care
The Primary Care Team: Taking
Multiple Roles In Caring for Persons With Cancer
Front
Office
Social
Worker/
Nurse Provider Pharmacist
Initiate a cancer care medical record
Cancer- sensitive communication
Screen for cancer related symptoms
Screen for palliative care needs
Help coordinate care
Encourage family participation in care
Assisting in care transitions
PLAY VIDEO: INTAKE SPECIALIST & OFFICE STAFF
PLAY VIDEO: INTAKE SPECIALIST & OFFICE STAFF
Best Practices 1:
Welcoming the New Patient With a Cancer History
• Acknowledgment of the cancer history & its relevance
• Welcoming patient to their “medical home”
• Assisting patient in information gathering
• Assisting patient in communication with providers
Consider Health Literacy
“ Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions".
• Low health literacy impacts cancer incidence, mortality, and quality of life:
– Cancer screening information may be ineffective; as a result, patients may be diagnosed at a later stage.
– Treatment options may not be fully understood; therefore, some patients may not receive treatments that best meet their needs.
– Informed consent documents may be too complex for many patients and consequently, patients may make suboptimal decisions about accepting or rejecting interventions.
( Merriman, Betty, CA: A Cancer Journal for
Physicians, May/June 2002)
Patients With Low Health Literacy May Have
Difficulty With…
• Locating providers and services
• Filling out complex health forms
• Sharing their medical history with providers
• Interpreting test results
• Knowing the connection between risky behaviors and health
• Managing chronic health conditions
• Understanding directions on prescription labels
PLAY VIDEO: NURSE
PLAY VIDEO: NURSE
The New Patient Medical History Interview:
Cancer-related Components
1. Type of cancer /stage of diagnosis/current status
2. Cancer treatments/dates/places/dosages
3. Treatment-related side-effects
4. Patient’s beliefs about their cancer and aftermath
Possible Cancer Trajectories
• Live cancer free for many years
• Live long cancer free, but die rapidly of late recurrence
• Live cancer free (first cancer), but develop second primary cancer
• Live with intermittent periods of active disease
• Live with persistent disease
• Live after expected death
Welch-McCaffrey et al., 1989
Definition of Cancer Stage
• Stage of cancer
– Extent that cancer has spread
– Correlated with prognosis
– Stages I, II, III, and IV
– Varies by cancer type
• “Early stage” (stage I and II): mostly curable
• “Locally advanced” (stage III): sometimes curable
• “Metastatic” (stage IV): rarely curable
Types of Cancer Treatments
• Surgery
• Radiation therapy
• Chemotherapy
• Immunotherapy
• Hormone therapy
Treatment type varies by type and stage of cancer
Late and Long-term Effects of Cancer
• Late effects refer specifically to unrecognized toxicities that are absent or subclinical at the end of therapy and become manifest later with the unmasking of hitherto unseen injury because of any of the following factors: developmental processes, the failure of compensatory mechanisms with the passage of time, or organ senescence.
• Long-term effects refer to any side effects or complications of treatment for which a cancer patient must compensate; also know as persistent effects, they begin during treatment and continue beyond the end of treatment . Late effects, in contrast, appear months to years after the completion of treatment.
SOURCE: Aziz and Rowland (2003).
Common Cancer Effects Can Be Helped With
Palliative Care Approaches in the Primary Care
Setting
Including:
• Pain
• Fatigue
• Anxiety/depression
• Sexual side effects
PLAY VIDEO: PROVIDER
PLAY VIDEO: PROVIDER
Pain & Palliative Care Assessment Tools
• FACT-G (B, C, M, P) Functional Assessment of Cancer
Therapy
– http://www.facit.org/about/overview_website.aspx
• Patient Comfort Assessment Guide
– www.partnersagainstpain.com
• Distress Management Screening Tool
– www.nccn.org
Possible Complaints by Type of Cancer History
GENERAL Pain, fatigue, sleep problems, swelling, weight loss, appetite problems, urinary or bowel problems, sexual dysfunction, shortness of breath
Breast Lymphedema, hot flashes
Colorectal Appetite, bowel problems, diarrhea, swelling, weight loss
Prostate Urinary problems, rectal bleeding, sexual dysfunction, hot flashes
Lung Pain, cough, shortness of breath
Patients With Cancer Histories May Have More
Functional Limitations
SOURCE: Hewitt et al. (2003).
Best Practices 2:
Responding to Cancer-related Symptoms In
Primary Care
• Prioritize symptoms and negotiate care plan with patient
• Set goals with patient to recover optimal level of functioning and quality of life
• Encourage patient, family and caregiver participation in care
Responding To Pain Complaints In Patients With
Cancer Histories
Main considerations:
• Type of pain
• Assessment of pain and functioning
• Steps of analgesic management
• Side-effects of pain management
• Non-pharmacological pain management
Common Types of Cancer Pain
• Somatic pain
• Visceral pain
• Neuropathic pain
Treatment induced chronic pain syndromes
Breast cancer
Head & Neck
Lung
Genitourinary
Intercostobrachial neuralgia
Phantom breast pain
Pain related to implants/reconstruction
Peripheral neuropathy
Osteoporotic vertebral compression fractures
Radiation induced plexopathy
Postcervical lymph node dissection pain syndrome
Accessory nerve damage
Jaw ostonecrosis
Shoulder pain
Post-thoracotomy pain syndrome
Chronic “chest tightness”
Pelvic pain syndrome
Osteoporosis
Vertebral compression fractures
Levy M, Chwistek M, Mehta RS. Management of chronic pain in cancer survivors. Cancer J 2008;14:401-
409
Guidelines for Responding to Pain in the Primary
Care Setting
• Promptly evaluate pain to rule out recurrence or new cancer or other medical problem (x-ray, bone scan, imagery?)
• Treat first with analgesics and non-pharmacologic therapies
• Refer intractable pain back to oncologist or pain specialist for narcotics and other approaches
Steps of Analgesic Pain Management
Common symptoms Type of pain Co-analgesic medications
Focal/incident pain Somatic
Dull, poorly localized Visceral
NSAIDs
Sharp, shooting, stabbing, burning
Localized to neural dermatome or distal extremities
Neuropathic Tricyclic antidepressants
Desipramine
Nortriptyline
Levy M, Chwistek M, Mehta RS. Management of chronic pain in cancer survivors. Cancer J 2008;14:401-
409
Common Side-Effects of Pain Management
• Constipation from narcotics
• Somnolence
• Gastrointestinal problems (e.g., dyspepsia or gastritis from NSAIDS)
Consider Non-pharmacologic Modalities
• Physical therapy
• Acupuncture
• Hypnosis
• Mindfulness-based stress reduction
• Cognitive behavior therapy
• Guided imagery
• Massage
Frequent Use of Complementary Therapies After
Cancer
• Relaxation techniques (44%)
• Spiritual forms of healing (42%)
• Nutritional supplements (40%)
• Meditation (15%)
• Massage (11%)
• Support groups (10%)
• Gansler T, Kaw C, Crammer C, Smith T. A population-based study of prevalence of complementary methods use by cancer survivors. Cancer 2008;113:1048-57.
Special Considerations In Pain Management In the
Primary Care Setting
• Even if you don’t prescribe narcotics in your practice, cancer patients may be taking them under the care of a pain specialist or oncologist
• There is a real stigma of addiction among patients and families which can be a barrier to pain control
• Patients may be reluctant to take adequate pain medications because they fear being over-medicated and less cognitively sharp
Best Practices 3:
Pain Management In Palliative Care
• Consider patient’s ability to function in usual activities and how to improve it
• Consider “double effect” approach to pain and multiple symptoms (e.g., treating anxiety first)
• Negotiate goals of care and treatment priorities with patient and family
• Coordinate team approach to care
Patient and Family Education About Pain
Palliation
• Relief of pain is important; there is no benefit to suffering with pain.
• There are many options to treating pain.
• When narcotic drugs are used appropriately to treat pain, addiction is rarely a problem.
• Communication with doctors and nurses about your pain is critical.
• Pain can be helped with non-pharmacologic therapies
Review:
Goals of Primary Care Provider With Patients with Cancer
Histories
• Comprehensive cancer-related history
• Surveillance for cancer spread, recurrence
• Assessment of medical and psychosocial effects of cancer
• Health promotion
• Palliative care intervention for consequences of cancer and its treatment
• Coordination of care between specialists and negotiation of care
• Assisting patients through care transitions
(including hospice care)
PLAY VIDEO: SOCIAL WORKER
PLAY VIDEO: SOCIAL WORKER
Psychological Impacts of Surviving Cancer
• Fear
• Feelings of isolation
• Ambivalence about completing treatment
• Coping with permanent disabilities
• Realization of lost opportunities
• Unanticipated depression when recovery is supposed to be a “good thing”
• Anxiety associated with checkups
• New meaning to life (“Post-traumatic growth”)
Psycho- Social lmpacts of Cancer
Risk Factors for Psychological Distress in
Survivors
– Unexpected symptoms
– No discussion of cancer within the family
– Family problems
– Low social support
– Pain and/or fatigue
– Co-morbidity
– Impaired professional work
– Previous psychiatric problems
*Massie MJ. Prevalence of Depression in Patients With Cancer. J Natl Cancer Inst Monogr 2004;32:57–71.
Components of Palliative Psychosocial Care for
Patients With Cancer Histories
• Know risk factors for psychosocial distress
• Assess psychosocial problems
• Provide supportive counseling
• Connect patients with appropriate services
• Coordinate psychosocial and biomedical care
• Engage family and caregivers in care
Interventions for Psychological Distress
– Relaxation therapy
• Progressive relaxation, Guided imagery, meditation, yoga
– Psycho-education
• Providing information through print, audiovision or chat rooms increases knowledge about cancer and reduces uncertainty
– Supportive-expressive therapies
• Group therapy, Art therapies
– Cognitive-behavioral therapy
• Changing maladaptive thoughts and behaviors
– Family therapy/Couples counseling
Jacobsen PB, Jim HS. Psychosocial interventions for anxiety and depression in adult cancer patients: achievements and
Challenges. CA Cancer J Clin 2008;58:214-230.
Comprehensive Cancer Care Includes End-of-Life Care
Palliative Care
Hospice Care
• Safe and comfortable dying
• Self-determined life closure
• Effective grieving
Hospice Care Goals:
Levels of Hospice Care
• Routine care
• General inpatient care
• Continuous care
• Respite care
Hospice Core services
• Interdisciplinary care
– Chaplaincy, nursing, medical social services, counseling, volunteers
– Hospice medical director
– Primary care physician
– Palliative care physician (consultation)
• Bereavement counseling
• Medical equipment, supplies
• Medications and therapies related to the terminal diagnosis
Review:
Role of the Primary Care Team
With Patients with Cancer Histories
• Communicate with and support the patient
• Assist patient and family retrieve and comprehend medical information
• Assess for AND respond to psychosocial problems
• Be aware of therapeutic options
• Have knowledge of community resources and covered services
• Address ongoing health maintenance needs
• Assist in care coordination
• Maintain regular contact
• Be available
Brotzman GL, Robertson RG. Role of the primary care physician after the diagnosis of cancer.
Prim Care. 1998;25:401–6
Cancer Supportive Care Resources
• Local resources
• State resources
• National resources
• Complementary and alternative care resources
COMPREHENSIVE
CANCER CARE FOR
THE RURAL PRIMARY
CARE PATIENT:
IT TAKES A TEAM!
PLAY VIDEO THROUGH END