Reimbursement Ambulatory & Other M'care & M'caid Reimbusement
advertisement

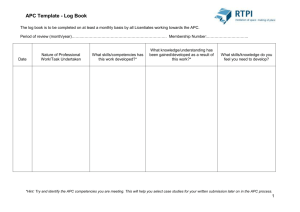
Reimbursement Ambulatory & Other M'care & M'caid Reimbusement Systems OUTPATIENT SIDE -- AMBULATORY (Part 1) Physicians (OutPt) paid on Resource-based relative value scale (RBRVS) BACKGROUND Physician (other allied health professionals) services include office visits, diagnostic/surgical procedures, therapies, wide range of settings. RBRVS / Fee-for-service / CMS's estimation of the value of service (not full price) M'care beneficiaries have cost-sharing: deductible and coinsurance Relative Value Scale: permits comparisons of labor, costs (supplies, equip, overhead), skill level (worth of the services) CPT CPT S.IL. S.IL. KNOW + (MP RVU)(MPGPCI)] = (SUM) x CF = MPFS Cost-sharing: For covered services, M'care beneficiary responsible for annual deductible and 20% coinsurance (out of pocket or supplemental insur). After deductible, provider receives 80% of PFS amount. POTENTIAL ADJUSTMENTS Budget Neutrality Adjustor (BN adjustor) Requires refinements that federal payment systems do not result in signficant differences in expenditures. Applied to (CF) component of generic formula to maintain Budg. Neutrality Upcoming expenditures must equal past expenditures (accounting for inflation). Payments to Drs. cannot differ > $20 million, otherwise apply another adjustment to CF. Application of the adjustor varies from year to year. Structure of Payment Relative Value Unit (RVU): Weight of CPT code S.IL. [(work RVU)(work GPCI) + (PE RVU)(PE GPCI) Outpt Facility Reimbursement (CMS) reimbursed by APC Payments RBRVS based on cost of furnishing physician services in different settings, skill/training required, and time and risk involved. Facility/ Nonfacility Calculation CPT Ch-7: Page | 1 Geographic adjustment This is why one must recognize importance of monitoring the Federal Register Conversion Factor Clinician Type: 3 types RVU & Geographic Practice Cost Index Participating - Agree to accept Assignment of Benefits (contract to bill M'care directly for covered expenses, beneficiary only for coinsur. & deductible, & accept M'care payment in full.) Nonparticipating - (Opt Out) No assignment of benefits contract and they do not get direct payments from Medicare. Allows coinsurance portion can be higher (paid to Dr). Disadv: Slower payment turnaround/cashflow problem, Less 5% of Participating payment, Patient pays/liable for higher portion. Anesthesiologists - Their own CF adj. for geographic location (no GPCI tbl). Generic Formula: RBRVS based on HCPCS Level I and Level II codes Each code is assigned an RVU (wt) for time, skill level, equipment needed. (high complexity = higher wt) RVU: 3 elements Physician Work (wt) for time spent providing service and intensity, effort & judgment, skill, stress Physician practice expense (PE): costs for overhead, (payroll, ofc expenses (rent, utilities, phone), medical materials/supplies, equipment expenses, all other expenses o Facilities (Physician Office) More Overhead o Nonfacilities (hospital/clinic) Less Overhead Malpractice (MP) /Professional Liability Insurance (PLI) Geographic practice cost indexes (GPCIs) Each element of RVU adjusted based on geog. location. [Base Unit + Time (in units)] x CF = MPFS Nonphysician Providers - Midwives (NPs), therapists, clinicians, social workers, etc. paid only 85% of full MPFS amt and only when their services are NOT "incident to" direct supervision of physician. If under direct (employed by) supervision, they are paid by salary. Conversion Factor: an across-the-board multiplier set by CMS. CF converts RVU into M'care Provider Fee Schedule (PFS). This is the gov't's direct control on M'care payments to physicians and other professionals. CF posted in Federal Register annually. Sustainable Growth Rate (SGR): CF calculated using formula called SGR to protect M'care trust fund. Matches updates in Dr. reimb to growth in national economy. CMS estimates growth of nat'l economy to create a target for M'care spending on Dr. services. A negative update sets CF less than the previous year. Special Circumstances - Modifiers Bilateral - 1st (total charge paid), 2nd (50% charge) = 150% Multiple procedures - (-51) 1st (100%) + 2nd-5th (50%) + 6th or more (require review) Physician Assisting in Surgery - Assistant (16%) of PFS amt for the primary surgeon. Reimbursement Ambulatory & Other M'care & M'caid Reimbusement Systems Underserved Area (Part 2) HPSA = Health Professional Shortage Area Bonus pmnt (incentive) for providing services designated in an HPSA. Based on the location of the service. AQ modifier to specify HPAS eligibility for zip codes not entirely in HPAS area. Receive 10% bonus quarterly. Quality PQRS = Physician Quality Reporting System endorsed by a consensus org such as at'l Quality Forum or devel'd by physic. assoc. Participation is Voluntary. Physicians doing specialty studies of group measures. (Optional participation in Category II codes for Quality Studies). EP - Eligible Professional. EPs and reimb. specialists should carefully review indiv. measures, grp measures, & specs bcs CMS may add/delete/alter measures each year. EPs may choose to report on indiv. or grp measures (except back pain has to be grp). EPs choose to rpt quality data thru claims-based or registry-based submissions (except CABG has to be thru registry). Claims-based submission uses CPT Category II or G codes. Registry-based - EPs submit info to PARS-qualified clinical data registry & registry submits quality data (to CMS). Incentives req'd by TRHCA (act) may be positive or negative. Positive 2012-14: EPs successfully reporting qual. meas. (w/in 2 mo. of the end of a reporting period) receive (bonus = 0.5% of allowable charges) Negative 2015: EPs who do not satisfactorily rpt qual. data under PQRS are subject to 1.5% reduction of their MPFS. 2016: Reduction is 2%. Technology (by ARRA HITECH) E-prescribing Incentives EHR Incentives Physician submits Rx to pharmacy electronically. EPs rpt data on e-prescribing w/G codes (Jan 1-Dec 31) Incentives (Mandatory after 2012) Positive incentives for rpting. 2011-16: EPs who are "meaningful EHR users" may receive incentive pmnts thru CMS reimbursement (w/limits) Negative unsuccessful EPs pmnts are negatively adj. 2012: by 1%. (99% of MPFS). 2013: by 1.5% (98.5%) 2014: by 2% (98%) 2015: M'care will apply penalty to EPs who cannot demonstrate meaningful use. No penalty under M'caid. Restrictions: M'care EPs cannot earn bonuses under both eRx and EHR Hospital-based EPs are ineligible for M'care or M'caid EHR incentive program. Ch-7: Page | 2 Temporary Bonuses from Affordable Care Act (ARA) Primary Care Incentive Pmnt (PCIP) Btwn 2011-16, primary care phys. (PCP) receive 10% increase in pmnts for specific services. E/M services for office, nursing home, or home health visit. PCPs eligible for HPSA bonus may also receive the PCIP bonus. HPSA Surgical Incentive Pmnt (HSIP) Gen'l surgeons providing services in HIPSA are eligible for incentive pmnt. 10% of Profees (M'care B) Eligible surgeons may only receive HSIP bonus, not also HPSA bonus. OPERATIONAL ISSUES Close mgmt of operations critical for small offices w/little margin: Processes to ensure full, accurate reimbursement The impact of unnecessary admin. costs Coding & Documentation Poor coding & inadequate doc. negatively affect (adj) RBRVS reimb. (see Tbl 7.10, 11, 12) Unnecessary Administrative Costs Staffing has a large impact on small practices. People are hired to deal with processing claims & trying to get reimbursement (contacting multiple health plans for prior authorizations, billing requirements, claim submission & adjudication procedures, formularies). Efficiency has the potential to reduce these unnecessary costs. Summary RBRVS pmnt system is a fee-for-service pmnt method. CMS's estimation of the value of a phys. services Physician's work Practice expenses, Malpractice determine RVU of phys. services. The RVU is adjusted for geographic location (converted to $ amt with CF) Other adjustments budget neutrality type of clinician providing service special circumstances, add'l geographic considerations other factors Accurate coding and complete documentation underpin full and accurate physician reimbursement. Reimbursement Ambulatory & Other M'care & M'caid Reimbusement Systems Ch-7: Page | 3 Hospital Outpt Prospective Payment System (H-OPPS, p. 175) (Oh, please play something!) 1983 IPPS went live & went so well that the they moved many other sectors to the same type of system. Hospital side moved in Aug. 2000. 3M HIS 1988-90 developed & came up with ambulatory patient groups (APGs). 1995 APGs updated. CMS didn't pick this up yet. 1997 BBA set dates for M'care to move to PPS in 1999. 1998 CMS released proposed rule for OPPS (using ambulatory pmnt classifications (APCs), revised APGs. Maintenance of H-OPPS (p. 178) CMS maintains OPPS by annual review of APC groups and relative wts. APC Advisor Panel assists (15 experts) with analysis and recommendations, but CMS makes final ruling for updates and changes to OPPS. MedPAC provides Congress & CMS w/recommendations to improve OPPS. CMS considers, but can do what it wants. CMS makes final updates and changes to OPPS. Revisions to OPPS released in Federal Register within 45 day (Mid-November) of the start of the CY. Hold-harmless Status: Gov't lesgislation(BIPA, 2000) provided exclusions for (supplementary modifications to APC system) specialized facilities: Child's, cancer, hosp's. No penalties for not participating in OPPS. Pass-through APC category developed for high-cost drugs, biol. agents, devices. Provided method for dealing with exclusions. Ambulatory Payment Classification System (APC) Each APC grp comprises procedures or services that are clinically comparable w/respect to resource use. Group like things together. Packaging: occurs when reimb for minor ancillary services assoc. w/significant procedure are combined into a single pmnt for the procedure. Bundling: occurs when pmnt for mult. significant procedures or mult. units of the same procedure related to an outpt encounter or episode of care is combined into a single unit of pmnt. Groupers in APC: The logic includes ancillary pkging and bundling. These are all CMS incentives for HC facilities to improve their efficiency by avoiding unnecessary ancillary services, supplies,, & pharmaceuticals, and by substituting less expensive, but equally effective, options. OPPS Methodology (p. 176) OPPS devel'd for outpt services to help encourage a more efficient delivery of care for outpt beneficiaries. Reimbursement for H- Outpt Services - 3 methods Fee schedules: A fee schedule system establishes a separate pmnt amt for each item/service and no packaging. Ex: Amb. Transp, PT, OT, Lab services Prospective Payment (APC): costs for certain items & 2ndary services assoc. w/primary proced. are pkg'd into the pmnt for that procedure. Ex: ESRD services Cost-based: Certain items/services (acquis. of tissues/vaccines, etc) continue to be paid on reasonable cost basis. RBRVS is a fee-for-service pmnt. Reporting of Services & supplies under H-OPPS Payment Status Indicator: Every HCPCS code assigned this to establish how that service, procedure, or item is paid (fee schedule, APC, reasonable cost, unpaid). OPPS covers only outpt services, even tho HCPCS was designed for all physician services. To move off the inpt-only list, a procedure must be performed in outpt settings at least 60% of the time. To be reimbursed, procedures indicated as inpt only must be provided to M'care beneficiaries in an inpt setting, and pmnt made under IPPS. Excluded Facilities CAHs; hospitals outside the 50 states, DC, Puerto Rico, Indian Health Service Ancillary Packaging: If present, ancillary service APC groups will automatically combine into a significant procedure or surgical service group: Guidance services Image processing services Intraoperative services Imaging supervision & interpretation svc Diagnostic readiopharmaceuticals Contrast media Observation services When ancillary service w/pmnt status indicator Q1 is performed on the same date of service as a service with an S, T, V, or X pmnt status indicator, then the ancillary service is packaged and has a pmnt rate of $0.00. If the ancillary service is performed without any S,T,V, or X services, then pmnt is provided for the ancillary service. APCFinder (Procedure drives the APC) Biopsy, liver, percutaneous (needle)... Guidance is status N with no payment bcs it is packaged in w/status T procedure. Bundling combines supply and pharmaceutical costs or medical visits w/assoc. procedures or services. Combining things together to make 1 pmnt. Bundled services w/HCPCS code have pmnt status indicator N. Reimbursement Ambulatory & Other M'care & M'caid Reimbusement Systems Structure of APC System (p. 182) Only 10 of 23 Payment Status Indicators (PSI) drive APC pmnts. Clinic or ED visit (PSI V) Significant procedure, mult reduction applies (PSI T) APC PSI Payment Rate (Fig. 7.5) 1 T 100% 2 T 50% 3 T 50% 4 S 100% T - Discounted 5 S 100% S-$ Significant procedure, not discounted when mult (PSI S) Ancillary service (PSI X) Non-pass-thru drugs/nonimplantable biol. agents, incl. therapeutic radiopharm (PSI K) Pass-thru drugs or biol agents (PSI G) Pass-thru device categories (PSI H) Partial hospitalization (PSI P) Blood or blood product (PSI R) Brachytherapy sources (PSI U) Each HCPCS code is assigned to one and only one APC. Tbl 7.19: G,H: Pass-thru, Calculate APCs, but cost-based pmnt K, P, R,S,T,U,V,X: APC Payments Q1, Q2, Q3: Conditionally pkg'd APC pmnts. Discounting (p. 184) Mult surg. procedures w/pmnt status indicator T performed during the same operative session are discounted. The highest-weighted procedure is fully reimbursed. All other procedures w/PSI T are reimbursed at 50%. Copayment (p. 182) CMS moved to OPPS to ensure beneficiary copmnt amt from hosp to hosp is consistent (20% of total charges). Charges are the same in same region bcs of wage index adj. Both M'care facility component and beneficiary copmnt components are adj'd for differences in wage indexes. This is the only adj made to APC pmnt rates to account for differences among hosp's. 60% of the facility amt is wage index adj'd. Copmnt may be collected at time of service or on a retrospective basis. Fig. 7.7: Wage Index Adjustment Formula for OPPS (p. 187) [(Nat'l unadjusted pmnt amt x 60%) x wage index] + (Nat'l unadjusted pmnt amt x 40%) = Locality payment or (Base rate x 60%) + (base rate x 40%) = Local Pmnt Ch-7: Page | 4 New Technology APCs (p. 183) These APCs house modern procedures and services until enough data are collected to properly place them in an existing APC or a new APC for the service/procedure. Category III codes. Classified by history which is being collected over time. 41 have PSI S with no discount 41 have PSI T and subject to mult-procedure discounting Composite APCs Allows for mult services that are typically performed together by one APC rather than mult APC. Mental health service composite APC 0034 Cardiac electrophysiological eval & ablation composite APC 8000 Low-dose rate prostate brachytherapy composite APC 8001 Multiple Imaging composite APCs o Ultrasound composite APC 8004 o CT & CTA w/out contrast composite APC 8005 o CT & CTA w/contrast composite APC 8006 o MRI & MRA w/out contast composite APC 8007 o MRI & MRA w/contast composite APC 8008 Observation Services An outpt in observation: Bundling costs for observ services into the APC pmnt for the procedure or visit. Exception APC 339 for which 3 clinical conditions qualify as an observ service: Chest pain, CHF, Asthma Partial Hospitalization An intensive outpt program of psychiatric services. May be provided by hospital outpt depts & M'care-certified community mental health centers. (Day care) Unit of Service for partial hosp. is one day. Therefore, APC paymentis based on a per diem amt. Interrupted Services 73 Interrupted surgery before anesthesia (50%) 74 interrupted surgery after anesthesia (100%) 52 Reduced Services (50%) Potential for an adjustment made to pmnt amt. High-Cost Outlier This is more for inpt, but a device or medication may apply on outpt side. Financial assistance to the facility for unusually high-cost services. Cost must exceed 1.75 times the APC pmnt AND the cost must also exceed the APC pmnt plus a fixed dollar threshold of $1900. THEN they take 50% of the difference (the hosp. is still losing money, but not as much as before this adjustment). Reimbursement Ambulatory & Other M'care & M'caid Reimbusement Systems Rural Adjustment Rural sole-community hosps (SCHs) cost was 7.1% > urban hosp. therefore SCHs are paid an additional 7.1% of the total amt. Ch-7: Page | 5 Pricer software completes steps 2-7. After step 7, pmnt made to the facility & data from the encounter added to nat'l claims history file. Outpt standard analytical file and OPPS file are extracts from nat'l claims history file and are used for statistical analysis and research. Cancer Hosp Adjustment IPPS-Exempt for some Hosps. Pass-Through Payments Exceptions to the M'care PPS system. For high-cost drugs, devices, etc. Will be assigned a Status Indicator of a Pass-through. These are paid on a cost-basis. Can stay pass-thru status for at least 2 yrs, but not more than 3 yrs. when it will be bundled into APC pmnt for the procedure in which the item is used or into an indiv. APC group. Transitional Corridor and Hold-Harmless Pmnts Hold-Harmless payments are permanent for IPPS-exempt cancer centers & children's hospitals. Eligible facilities receive a quarterly interim hold-harmless pmnt that provides additional reimbursement when the pmnt received under OPPS is < the pmnt the facility would have received for the same services under the prior reasonable cost-based system. (Makes up difference.) Ambulatory Payment Classification Assignment 1. Code the encounter accurately and completed. You have to know the CPT code to get to the APC. 2. Pull in Chargemaster driven codes 3. Run it through a code editor to check edits & see if it is appropriately coded and modify it appropriately, if necessary. 4. Find APC status indicator (Probably more than 1 APC on a claim). 5. Put claim thru a scrubber (OCE) Payment Determination 1. APC Assigned. Claims are sent to the MAC. Edits found on the OCE 2. APC pmnt rate established. Relative wt of APC x CF for that CY 3. Wage index adj'd to nat'l unadjusted facility component. 60 / 40 split (see Fig. 7.7) Wage index from Federal Register 4. Fee schedule amts applied Labs paid 5. Reasonable cost amnts applied. Vaccines paid at reasonable cost 6. M'care pmnts (all of the above) are added together. 7. Outlier add-on applied. Outlier calculation completed in pricer software for all eligible procedures & serv., then added to M'care pmnt. 3M & Quantim are encoders (find codes) and groupers (find APCs or DRGs). Pricer Calculates (determines actual pmnt amt).