Advantages
advertisement

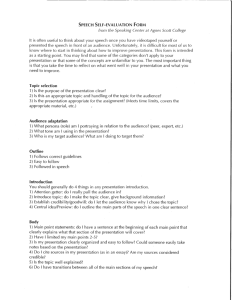
Hoarseness and Laryngitis Dept of Otolaryngology BERJIS N, MD Definition of Hoarseness • the perceived • • breathiness quality of the voice (Bailey) a rough or noisy quality of voice (Dorland) a rough, harsh voice quality (Stedman) Symptom –vs- Diagnosis • Hoarseness is a symptom of a disease process • Although hoarseness appears on the ICD9 as a diagnosis (784.49): – it is really a symptom resulting from the underlying disease process – the underlying disease process is your diagnosis (ex. vocal nodules) Anatomy: Laryngeal Cartilage Anatomy: Laryngeal Muscles Histology • Mucosal layer – Pseudostratified squamous epithelium superiorly and inferiorly – Nonkeratinizing squamous epithelium at contact surface of medial cord Histology • Subepithelial tissues: three layered lamina propria – Superficial Layer (Reinke’s space) – Intermediate layer – Deep layer • the intermediate and deep layers make up the vocal ligament • Vocalis and thyroarytenoid muscle Histology Physical Examination • Laryngeal mirror – Advantages: fast, inexpensive, minimal equiptment – Disadvantages: gag, nonphysiologic, no permanent image capability Physical Examination • Rigid Laryngoscopy (70 or 90-degree telescope) – Advantages: best optic image, magnifies, video documentation – Disadvantages: gag, nonphysiologic, expensive Physical Examination • Flexible fiberoptic nasolaryngoscope – Advantages: well tolerated, physiologic, video documentation – Disadvantages: time consuming, expensive, resolution limited by fiberoptics Physical Examination • Videostroboscopy – Advantages: allows apparent “slow motion” assessment of mucosal vibratory dynamics, video documentation – Disadvantages: time consuming, expensive Surgical Treatment Varices and Ectasias Cysts • Treatment – Cold instrument resection • Subepithelial infusion of saline and epinephrine is helpful • Must retreive entire cyst wall to prevent recurrence • Preserve normal SLP – Microspot CO2 laser not as effective due to necessity of delicate tangential dissection Cysts • Results – Mucosal wave usually improves – Does not return to normal if cysts has replaced substantial amount of SLP • SLP does not regenerate Cysts Granulomas • Results from hypertrophic inflammatory reaction due to traumatic mucosal disruption • Majority found in arytenoid region • Usually exophytic with narrow base • Typically arise in patients with LPR • Seen with endotracheal intubation Granulomas • Treatment – Vocal therapy including antireflux management – Surgical resection • conservative management has failed • concern of a neoplastic process • airway compromise Granulomas Granulomas Granulomas Granulomas Polypoid Corditis (Reinke’s Edema) • Extensive swelling of SLP • Usually on superior surface of musculo- membranous vocal fold • Typically bilateral but asymmetric volume • Multifactorial cause – Smoking – LPR – Vocal hyperfunction Polypoid Corditis (Reinke’s Edema) • Treatment – – – – Smoking cessation Antireflux medication Preoperative vocal therapy Surgery • Epithelial microflap elevation with SLP contouring and reduction using either cold instruments, Microspot CO2 laser, or both • Vocal ligament should never be visualized • Both vocal folds can be treated in one procedure if flap is elevated on superior surface of vocal fold Polypoid Corditis (Reinke’s Edema) Papillomatosis • Human papillomavirus 6 and 11 • Confined to epithelium – Excision should preserve SLP • Most commonly found in musculo- membranous region, but may extend into arytenoid, ventricle, subglottis Papillomatosis • Surgical treatment – Cold instruments – Microdebrider – Microspot CO2 laser • Resection of lesions inhibits recurrence in 30% of chronic patients Papillomatosis Physiology 1. Airway protection 2. Swallowing 3. Voice production 4. Air passage inspiration phonation Common laryngeal disorders 1. Acute laryngitis 2. Croup 3. Epiglottitis 4. Vocal nodule 5. Vocal polyp 6. Vocal granuloma 7. Laryngeal carcinoma 8. Laryngeal trauma 9. Laryngopharyngeal reflux (LPR) Laryngitis •Laryngitis is inflammation of the vocal cords •Laryngitis can be acute (short term) or chronic • Short term laryngitis usually follows upper respiratory infections. • Long term laryngitis is most commonly caused by misuse, overuse and exposure to smoke, dust and other irritants, as well as acid reflux. Acute laryngitis Pathogen - adenovirus, influenza Morexella catarrharis Hemophilus influenza Streptococcus pneumoniae Symptoms - hoarseness cough, +/- fever, malaise Sign - TVC swelling Acute laryngitis Treatment - voice rest - mucolytic, anticold +/- antibiotic Symptoms > 2 week, recurrent DDx - chronic laryngitis Croup (acute laryngotracheobronchitis) - Severe respiratory infection - 6 months-2 yrs. Pathogen - parainfluenza*influenza, adenovirus - follow by bacterial esp. H. influenza Symptoms - early URI symptoms - 2-3 days - barking cough, stridor - exhausted, lying down Croup (acute laryngotracheobronchitis) Diagnosis - symptoms & signs - flexible scope - x-ray norrowing of subglottis “Pencil’s sign” Pencil’s sign Normal Croup (acute laryngotracheobronchitis) Treatment - early detection - observe, admit - humidification, hydration, O2 - antibiotic (penicillin) severe - steroid - intubation Epiglottitis Signs - epiglottis > swelling, inflam - ** laryngospasm เมื่อกดลิ ้น - fiberoptic X-ray - “Thumb’s sign” Epiglottitis Treatment - admit, closed monitoring broad spectrum penicillin hydration, humidification +/- steriod prepare for intubation Aetiology • Congenital • Traumatic • Inflammatory • Neoplastic • Functional Congenital • Laryngomalacia (75%) - a “rough” cry associated with stridor which is worse when feeding and begins within a few weeks of birth Congenital • Neurological (10%) - unilateral or bilateral recurrent nerve palsies (idiopathic or birth trauma) Congenital • Other - laryngocoele (blind sac of the laryngeal ventricle) - haemangioma (site determines severity of dysphonia) Laryngitis Sicca Laryngistis sicca is caused by inadequate hydration. The protective mucus normally needed for the vocal cords becomes too thick and they cannot open or close properly. Acid Reflux •Acid reflux affects singers in that the stomach acid can flow past the esophagus into the throat. •Small amounts of reflux can cause considerable damage. The left picture is damage from acid reflux. Notice how the vocal cords are mostly red instead of white. The right picture is the same vocal cords after successful treatment. Grandulomas Another result of acid reflux. Symptoms • Hoarseness • Bad/bitter taste in mouth (especially in morning) • Chronic (on-going) cough • Asthma-like symptoms • Frequent throat clearing • Referred ear pain • Pain or sensation in throat • Post-nasal drip • Feeling of "lump" in throat • Singing: Difficulty hitting high notes • Problems while swallowing Hemorrhage A vocal hemorrhage is actually a ruptured blood vessel on the true vocal cord, and bleeding into the tissues of the fold. It is a rare occurrence caused by aggressive use of the vocal cords (e.g. cheerleading) Common Signs of Vocal Abuse by Prof. David Otis Castonguay, Radford Univ. • Throat is tender to the touch after use. • Voice is hoarse at the end of singing. • Throat is very dry, with a noticeable “tickle” that • • is persistent. Check dehydration. Inability to produce your highest notes at pianissimo volume. Persistent hoarseness or an inability to sing with a clear voice after 24-48 hours of vocal rest. www.radford.edu/~dcastong/ARTARCH/vocal.html