Clinical Pharmacy Department Drug Therapy Modul 1. Introduction
advertisement

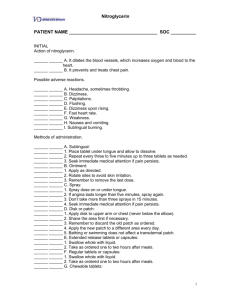
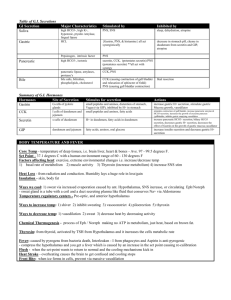
Clinical Pharmacy Department Drug Therapy Modul 1. Introduction to the drug therapy with the basics of pharmacokinetics. Principles of rational pharmacotherapy. Pharmacotherapy of diseases of internal organs Which of the following substances has its major activity as a saline cathartic? A. sodium bicarbonate B. methylcellulose C. sodium phosphate D. castor oil E. mineral oil ANSWER: C The correct statement regarding sucralfate: A. pharmacologic action is to reduce gastric acid secretion by antagonizing gastrin B. enhances N+-K+ ATPase C. antagonizes acetylcholine D. most common side effects is constipation E. increases gastric motility ANSWER: D Correct statement regarding metoclopramide: A. central nervous system dopamine receptor agonist B. peripheral blockage of acetylcholine at muscarinic synapse C. decreases lower esophageal sphincter pressure D. adverse effects include dystonic or extrapyramidal effects E. increases motility of colon ANSWER: D In general, mechanisms of laxation include: A. adding bulk to the stool B. increasing peristaltic activity C. emulsifying aqueous and fatty substances with stool D. lubricating the passage of stool E. All of the above ANSWER: E Appropriate indications for and/or uses of laxatives include: A. prevent straining at the stool in patients with cardiovascular disease B. bulk forming agents for diverticular disease C. treatment of drug overdose D. All of the above E. None of the above ANSWER: D Which of the following substances is most likely to cause systemic alkalosis? A. sodium bicarbonate B. methylcellulose C. sodium phosphate D. castor oil E. mineral oil ANSWER: A Adverse effect(s) of laxatives: A. electrolyte disturbances (hypernatremia, hypokalemia) B. dehydration C. spastic colitis with stimulant laxatives D. gastrointestinal obstruction with bulk forming agents E. All of the above ANSWER: E In esophagitis, elevation of the head of the bed, abstinence from ethanol and tobacco, and small frequent meals are all useful adjunctive therapeutic measures. Other useful therapy may include all of the following EXCEPT: A. omeprazole B. metoclopramide C. bethanechol D. cimetidine E. amitriptyline ANSWER: E Drug which exerts anti-peptic ulcer effects through histamine-2 receptor antagonism: A. sucralfate B. ranitidine C. metoclopramide D. omeprazole E. misoprostol ANSWER: D Agents of potential use in peptic ulcer disease include: A. muscarinic antagonists B. proton pump inhibitors C. antacids D. prostaglandins E. All of the above ANSWER: E Possible drug interactions: Aluminium hydroxide antacids tend to interfere with the gastrointestinal absorption of: A. cephalexin B. penicillin G C. erythromycin D. chloramphenicol E. tetracycline ANSWER: E Prostaglandins E2 inhibit the secretion of gastric acid and stimulate the secretion of mucus. One adverse effect limiting the wide use of prostaglandins for gastric disease is: A. headache B. thrombocytopenia C. gynecomastia D. diarrhea E. seizures ANSWER: D Antacids having a relatively non-systemic effect include: A. aluminum hydroxide B. sodium bicarbonate C. calcium carbonate D. all of the above E. aluminum hydroxide and calcium carbonate ANSWER: E One mechanism to reduce gastric acid secretion is by blocking the H+Na+ATPase pump in the parietal cell. One drug that has this pharmacologic action is: A. misoprostol B. pirenzepine C. omeprazole D. serotonin E. isoniazid ANSWER: C The amount of sodium, phosphate or magnesium contained in an antacid should be assessed when selecting an antacid for patients with: A. renal insufficiency B. congestive heart failure C. ascites D. All of the above E. None of the above ANSWER: D The concomitant administration of calcium and/or magnesium antacids to patients receiving one of the tetracycline drugs may have which of the following effects upon the action of the tetracycline: A. enhances the action B. causes no significant change C. decreases the action D. increases toxicity E. suppresses hypersensitivity reactions ANSWER: C In general, mechanisms of laxation include A. adding bulk to the stool B. increasing peristaltic activity C. emulsifuing aqenons and fatty substances with stool D. lubricating the passage of stool E. all of the above ANSWER: E Drug which exerts anti-peptic effects through histamine-2 receptor antagonism: A. Denol B. Ranitidine C. Omeprasole D. Aluminium hydroxide E. All of above ANSWER: B For treatment of heartburn patient regularly used some powder. After a week of drug using vomiting, nausea, abdomen pain, fibrillation, shallow and slow breathing. Biochemical examination show alkalosis. What drug used patient? A. Natrii hydrocarbonas B. Aluminium hydroxide C. Magnesium sulfate D. Omeprasole E. Calcium carbonate ANSWER: A All these Drugs are cause obstipation Except: A. Anticholinergic agents B. Ca channel antagonists C. Opioids D. Tricyclic antidepressants E. Muscarinic agonists ANSWER: E In the treatment of acute diarrhea A. antibiotics are worst avoided in non-pathogenic diarrhea B. antibiotics are worst avoided in viral gastroenteritis C. oral rehydration should not be used for initial therapy D. electrolytes and glucose should not be supplemented for initial therapy E. oral rehydration and electrolytes supplementation are required particularly in children and in the elderly ANSWER: E In patients with diarrhea the following can be used Except A. antibiotics to treat systemic illness B. antibiotics in evidence of bacterial infection C. antidiarrheal drugs decreasing intestinal transit time D. antidiarrheal drugs increasing bulk and viscosity of the gut contents E. opioids, antimuscarinics ANSWER: C Peptic ulcer disease A. is an acute disorder B. characterized by frequent recurrences C. comprises bones D. the incidence of duodenal ulcers is four to five times lower than that of gastric ulcer E. affects approximately 50% of the population ANSWER: B All these are major factors of known importance for the etiology of ulceration Except A. acid-pepsin secretion B. mucosal resistance to attack by acid and pepsin C. the age D. effects of non-steroidal anti-inflammatory drugs E. the presence of Helicobacter pylori ANSWER: C Antacids: A. react with gastric acid to form a neutral salt B. produce sweating C. are Ineffective at healing duodenal ulcer D. are very effective at healing gastric ulcers E. its effect on acid secretion lasts for long (5 hours) ANSWER: A Antacids include: A. balsalazide B. orlistat C. cimetidine D. sucralfate E. aluminium salts (hydroxide, phosphate, glycinate) ANSWER: E Sodium bicarbonate (an antacid) A. acts only locally B. excessive doses produce systemic acidosis C. produces carbon monoxide by reacting with hydrochloric acid D. causes belching and distension of the large intestine E. sodium intake need not to be considered in patients with hypertension or heart failure ANSWER: B Magnesium and aluminium salts A. do undergo absorption so are effective locally B. magnesium salts are constipating, aluminium salts may produce diarrhea C. can not reduce the rate and extent of absorption of other drugs D. aluminium salts should not be used with caution with any renal compromise E. magnesium and aluminium salts are taken 1-3 hours after meals and at bedtime ANSWER: E H2 lytics: A. at least 4 days treatment is required to achieve healing B. pain is relieved within 4 weeks treatment C. include morphine , tramadol D. include nizatidine, ranitidine, famotidine E. include pirenzepine ANSWER: D Omeprazol A. is an irreversible stimulator of the proton pump B. can be used only for healing gastric ulcer C. Is for women only D. is taken once weekly E. degrades in the presence of moisture. Capsules are supplied in special containers ANSWER: E Misoprostol A. is a synthetic analog of prostaglandin E1 B. produces gastric acid secretion C. causes Stricture in the submucosa D. decreases production of protective mucus E. is indicated especially in pregnancy ANSWER: A Pharmacokinetics is: A. The study of biological and therapeutic effects of drugs B. The study of absorption, distribution, metabolism and excretion of drugs C. The study of mechanisms of drug action D. The study of methods of new drug development E. All of the above ANSWER: B What does “pharmacokinetics” include? A. Complications of drug therapy B. Drug biotransformation in the organism C. Influence of drugs on metabolism processes D. Influence of drugs on genes E. All of the above ANSWER: B What does “pharmacokinetics” include? A. Pharmacological effects of drugs B. Unwanted effects of drugs C. Chemical structure of a medicinal agent D. Distribution of drugs in the organism E. All of the above ANSWER: D What does “pharmacokinetics” include? A. Localization of drug action B. Mechanisms of drug action C. Excretion of substances D. Interaction of substances E. All of the above ANSWER: C The main mechanism of most drugs absorption in GI tract is: A. Active transport (carrier-mediated diffusion) B. Filtration (aqueous diffusion) C. Endocytosis and exocytosis D. Passive diffusion (lipid diffusion) E. None of the above ANSWER: D What does the term “bioavailability” mean? A. Plasma protein binding degree of substance B. Permeability through the brain-blood barrier C. Fraction of an uncharged drug reaching the systemic circulation following any route administration D. Amount of a substance in urine relative to the initial doze E. Amount of a substance obtained orally and quantity of intakes ANSWER: C The reasons determing bioavailability are: A. Rheological parameters of blood B. Amount of a substance obtained orally and quantity of intakes C. Extent of absorption and hepatic first-pass effect D. Glomerular filtration rate E. Permeability through the brain-blood barrier ANSWER: C Pick out the appropriate alimentary route of administration when passage of drugs through liver is minimized: A. Oral B. Transdermal C. Rectal D. Intraduodenal E. All of the above ANSWER: C Which route of drug administration is most likely to lead to the first-pass effect? A. Sublingual B. Oral C. Intravenous D. Intramuscular E. Rectal ANSWER: B What is characteristic of the oral route? A. Fast onset of effect B. Absorption depends on GI tract secretion and motor function C. A drug reaches the blood passing the liver D. The sterilization of medicinal forms is obligatory E. All of the above ANSWER: B Tick the feature of the sublingual route: A. Pretty fast absorption B. A drug is exposed to gastric secretion C. A drug is exposed more prominent liver metabolism D. A drug can be administrated in a variety of doses E. All of the above ANSWER: A The term “biotransformation” includes the following: A. Accumulation of substances in a fat tissue B. Binding of substances with plasma proteins C. Accumulation of substances in a tissue D. Process of physicochemical and biochemical alteration of a drug in the body E. All of the above ANSWER: D In case of liver disorders accompanied by a decline in microsomal enzyme activity the duration of action of some drugs is: A. Decreased B. Enlarged C. Remained unchanged D. Changed insignificantly E. Remained unchanged or changed insignificantly ANSWER: B Half life is the time required to: A. Change the amount of a drug in plasma by half during elimination B. Metabolize a half of an introduced drug into the active metabolite C. Absorb a half of an introduced drug D. Bind a half of an introduced drug to plasma proteins E. All of the above ANSWER: A An agonist is a substance that: A. Interacts with the receptor without producing any effect B. Interacts with the receptor and initiates changes in cell function, producing various effects C. Increases concentration of another substance to produce effect D. Interacts with plasma proteins and doesn’t produce any effect E. Interacts with plasma proteins and produce various effects ANSWER: B If an agonist can produce maximal effects and has high efficacy it’s called: A. Partial agonist B. Antagonist C. Agonist-antagonist D. Full agonist E. None of the above ANSWER: D If an agonist can produce submaximal effects and has moderate efficacy it’s called: A. Partial agonist B. Antagonist C. Agonist-antagonist D. Full agonist E. Agonist-antagonist and partial agonist ANSWER: A The substance binding to one receptor subtype as an agonist and to another as an antagonist is called: A. Competitive antagonist B. Irreversible antagonist C. Agonist-antagonist D. Partial agonist E. Full agonist ANSWER: C Give the definition for a therapeutical dose: A. The amount of a substance to produce the minimal biological effect B. The amount of a substance to produce effects hazardous for an organism C. The amount of a substance to produce the required effect in most patients D. The amount of a substance to accelerate an increase of concentration of medicine in an organism E. All of the above ANSWER: C Which effect may lead to toxic reactions when a drug is taken continuously or repeatedly? A. Refractoriness B. Cumulative effect C. Tolerance D. Tachyphylaxis E. Toxic effect ANSWER: B What term is used to describe a more gradual decrease in responsiveness to a drug, taking days or weeks to develop? A. Refractoriness B. Cumulative effect C. Tolerance D. Tachyphylaxis E. withdrawal syndrome ANSWER: C Tachyphylaxis is: A. A drug interaction between two similar types of drugs B. Very rapidly developing tolerance C. A decrease in responsiveness to a drug, taking days or weeks to develop D. None of the above E. All of the above ANSWER: B The situation when failure to continue administering the drug results in serious psychological and somatic disturbances is called? A. Tachyphylaxis B. Sensibilization C. Abstinence syndrome D. Idiosyncrasy E. All of the above ANSWER: C What is the type of drug-to-drug interaction which is connected with processes of absorption, biotransformation, distribution and excretion? A. Pharmacodynamic interaction B. Physical and chemical interaction C. Pharmaceutical interaction D. Pharmacokinetic interaction E. Pharmacokinetic interaction+ Pharmaceutical interaction ANSWER: D What is the type of drug-to-drug interaction which is the result of interaction at receptor, cell, enzyme or organ level? A. Pharmacodynamic interaction B. Physical and chemical interaction C. Pharmaceutical interaction D. Pharmacokinetic interaction E. Chemical interaction ANSWER: A A teratogenic action is: A. Toxic action on the liver B. Negative action on the fetus causing fetal malformation C. Toxic action on blood system D. Toxic action on kidneys E. Toxic action on the mother and the fetus ANSWER: B Mother, whose child suffered from dry cough that did not let her to sleep at night, consulted a pediatrician. What preparation can’t be used in such case? A. Libexyn. B. Tusuprex. C. Codeine. D. Bromhexyn. E. Acetylcistein. ANSWER: C A patient admitted to the hospital with a diagnosis of pneumonia asks the nurse why she is receiving codeine when she does not have any pain. The nurse's response is based on knowledge that codeine also has what effect? A. Immunostimulant. B. Antitussive. C. Expectorant. D. Immunosuppressant. E. Antihistamine. ANSWER: B The patient with severe allergic bronchial asthma has been treated by oral drug during 7 months. Hypertension, “moon face”, obese trunk, oedema, insomnia occur. What drugs does he used? A. Patient used one of orally used glucocorticoids, e.g. prednisolonum. B. Patient used one of beta-agonists. C. Patient used cromolynum. D. Patient used euphyllinum E. Patient used all above. ANSWER: A Common adverse reactions of corticosteroidal therapy are: A. bradycardia, mental dullness B. anorexia, polyuria C. tachycardia D. “moon face”, obese trunk E. insomnia ANSWER: D The most specific agent for prevention of asthma is: A. Salbutamolum B. Libexinum C. Adrenalini hydrochloridum D. Pertussinum E. Mucaltinum ANSWER: A Regarding its actions, cromolyn is best described as: A. bronchodilator B. anticholinergic C. beta agonist D. inhibitor of mast cell degranulation E. glucocorticoid ANSWER: D Which of the following work through cholinergic receptor antagonism? A. isoetharine B. cromolyn C. ephedrine D. ipratropium E. salmeterol ANSWER: D A 20-yr-old woman presents with a week's history of fever, rigors arid productive rusty cough. CXR shows right lower lobe consolidation. Prescribe treatment A. Erythromycin B. Co-trimoxazole C. Prednisolone D. Amoxicillin E. Salbutamol inhaler ANSWER: D Which of the following asthma severity categories has a treatment including inhaled low-dose steroid, cromolyn, nedocromil, zafirlukast or zileuton? A. Mild intermittent asthma B. Mild persistent asthma C. Moderated persistent asthma D. Severe persistent asthma E. Exercise-induced asthma ANSWER: B Which of the following, along with Formoterol, is a long acting anti-asthmatic? A. Albuterol B. Salmeterol C. Metaproterenol D. Terbutaline E. Pirbuterol ANSWER: B Rifampin is used mainly in the treatment of: A. cholera B. typhoid fever C. tuberculosis D. rickettsial diseases E. pseudomonas infections ANSWER: C The drug applied at the case of hypersusceptibility to nitroglycerine for removing attack of angina pectoris A. Aspirin B. Atropine C. Piracetame D. Papaverine E. Molsidomine ANSWER: E The clot aggregation blocker oppressing the Adenosine absorption and reducing its enzyme destruction A. Papaverine B. Propranolol C. Reserpine D. Dipiridamole E. Trental ANSWER: D What group does Trimetazidine belong to? A. Adrenomimetics B. Cholinoblockers C. Cardioprotectors D. Sympatholitics E. Diuretics ANSWER: C The cardioselective beta-adrenoblocker A. Atenolol B. Adrenalin C. Riboxinum D. Enalapril E. Nifedipine ANSWER: A The drug applied for the medical treatment of ischemic heart disease A. Sympatholitics B. beta-Adrenoblockers C. alpha-Adrenoblockers D. Myorelaxants E. M-cholinomimetics ANSWER: B Which drug belongs to the beta-adrenoblockers’ group? A. Nitroglycerine B. Metoprolol C. Captopril D. Nifedipine E. Furosemidum ANSWER: B The action of nitroglycerine and others organic nitrates is caused by A. The blockade of potassium channels B. The blockade of sodium channels C. The blockade of calcium channels D. The release of nitrogen oxyde in the vessel walls E. The excitation of beta2 -adrenoreceptors vessels ANSWER: D The efficiency of Nifedipine at arterial hypertension is caused by A. The dilation of vessels B. The rise of myocardium contractility C. The decline of renine production D. The decline of diuresis E. The rise of diuresis ANSWER: A Which drug belongs to the Calcium-channel blocker group? A. Papaverinum B. Atenolol C. Verapamil D. Furosemidum E. Anaprilinum ANSWER: C The drug applied for the medical treatment of ischemic heart disease A. alpha-Adrenoblockers B. Sympatholitics C. Diuretics D. M-cholinomimetics E. Nitrates ANSWER: E Which drug decreases the demand in oxygen due to the blockade of the sympathetic innervation? A. Molsidomin B. Atenolol C. Pentoxiphylline D. Papaverinum E. Nitroglycerine ANSWER: B The drug, applied sublingually at the attack of angina pectoris A. Isosorbide dinitrate B. Riboxinum C. Pentoxiphylline D. Atenolol E. Nitroglycerinum ANSWER: E Which drug belongs to the group of beta-adrenoblockers A. Nitroglycerine, Molsidomine B. Nebivolol, Atenolol C. Pentoxiphylline, Papaverinum D. Nifedipine, Verapamil E. Captopril, Enalapril ANSWER: B Which drug belongs to the group of antagonists of calcium ions A. Molsidomine, Nitroglycerine B. Anaprilinum, Atenolol C. Pentoxiphylline, Papaverinum D. Nifedipine, Verapamil E. Captopril, Enalapril ANSWER: D Which drug belongs to the inhibitors of ACE A. Nitroglycerine, Molsidomine B. Anaprilinum, Atenolol C. Pentoxiphylline, Papaverinum D. Nifedipine, Verapamil E. Captopril, Enalapril ANSWER: E Which drug is used for ischemic heart disease, hypertension and cardiac arrhythmias? A. Bisoprolol B. Sustac C. Nitroglycerine D. Novocainamidum E. Validolum ANSWER: A What antiarrhythmic drug has local anaesthetic activity? A. Novocainamidum B. Chinidinum C. Verapamilum D. Xycainum E. Dipheninum ANSWER: D For treatment of what arrythmias Lidocaine is the most effective? A. Ventrical tachyarrhythmia B. Atrium tachyarrhythmia C. Atrio-ventrical block D. Sino-auricular block E. Chronic paroxismal arrhythmia ANSWER: A For treatmant of what kind of arrythmia cardiac glycosides are contraindicated? A. Ventrical tachyarrhythmia B. Atrium tachyarrhythmia C. Extrasystolia D. Flutering of atrium E. Chronic paroxismal arrhythmia ANSWER: A Indicate the side effect of nitroglycerine A. Itching of skin B. Bradicardia C. Rise of arterial pressure D. Headache E. Intestine atony ANSWER: D Which antianginal drug provokes bronchial spasm? A. Sustac B. Propranolol C. Nitroglycerine D. Fenigidinum E. Molsidominum ANSWER: B Which preparation is drug of choice at attack of angina pectoris? A. Sustac B. Molsidominum C. Nitroglycerine D. Anaprilinum E. Fenigidinum ANSWER: C Why is not it impossible to apply nitroglycerine in case of high intracranial pressure? A. Increase АP B. Causes bradycardia C. Increase intracranial pressure D. Decrease intracranial pressure E. Provoke angina pectoris ANSWER: C Indicate possible side effect of propranolol? A. Hypertension B. Tachycardia C. Bradycardia D. Оrtostatic collapse E. Development of tolerance ANSWER: C Patient entered the cardiologic department with the attack of angina pectoris, where a medical treatment was appointed to him. After injection of medicines patient noted a strong headache and nausea. For what group of antianginal drugs is character such side effect? A. Blockers of calcium channels B. Beta – adrenergic blockers C. Nitrates D. Vasodilators action on the coronal vessels E. Beta – adrenergic stimulants ANSWER: C To indicate mechanism of Са2+ antagonists hypotensive action A. Decrease the tonus of vasomotor centers B. Block the postsynaptic beta-adrenoreceptors C. Block the sympathetic ganglions D. Block the calcium channels E. Stimulate the production of prostaglandins ANSWER: D To indicate side effect of Clophellinum (Clonidine) A. Increasing of arterial pressure B. Increasing of intraocular pressure C. Dryness in the mouth D. Increasing of glands secretion E. Increasing of intestine motility ANSWER: C To indicate the antihypertensive drug used for the medical treatment of hypertensive disease with tachycardia and extrasystoles. A. Methyldopa B. Reserpinum C. Bisoprolol D. Clophelinum E. Dibazolum ANSWER: C What diuretic is used for the removal of hypertensive crisis? A. Furosemide B. Mannitum C. Triamteren D. Dichlothiazide E. Spironolactonum ANSWER: A To indicate the drug – blocker of angiotensin converting enzyme. A. Anaprilinum B. Lisinopril C. Methyldopa D. Reserpinum E. Dibazolum ANSWER: B To indicate calcium channels blocker hypotensive drug A. Nifedepine B. Captopril C. Reserpinum D. Anaprilinum E. Dibazolum ANSWER: A The 45 years old patient has diagnosis Angina pectoris. Cardiosclerosis. Arrhythmia. Hypertensive disease, Choose the drug for treatment? A. Nebivolol B. Suprastine C. Potassium chloride D. Strophantine E. Lidocaine ANSWER: A At the patient after injecting drug for the medical treatment of hypertensive crisis tachycardia, and orthosthatic hypotension in the vertical position has developed. What drug was injected? A. Reserpine B. Clophelinum C. Magnesium sulfate D. Dibazolum E. Verapamilum ANSWER: B To the patient with hypertensive disease was prescribed a drug from the adrenotropic group. After some time the pressure normalized, but developed bradycardia (50 beats on minute) and the atrio-ventricar block. What drug was prescribed? A. Propranolol B. Papaverinum C. Clophelinum D. Mesatonum E. Verapamilum ANSWER: A The 45 years old patient with the hypertensive disease has been taking antihypertensive drug during 4 days. The blood pressure normalized but somnolence and dry cough developed. What drug has been taking the patient? A. Clophelinum B. Prazosinum C. Enalapril D. Aspirine E. Adrenaline ANSWER: C Patient with diagnosis of pheochromocytoma suffers from the high blood pressure which outgrows in hypertensive crisis. What group of drugs will help in this situation? A. Beta- adrenoblockers B. Ganglionblockers C. Sympatolitics D. alpha-adrenoblockers E. Calcium channels blockers ANSWER: D To indicate diuretic drug that is used for the removal of hypertensive crisis. A. Oxytocine B. Dichlothiazide C. Triamteren D. Spironolactonum E. Furosemide ANSWER: E To indicate what diuretics is used in the complex therapy of hypertensive crisis. A. Spironolactonum B. Furosemide C. Manit D. Dichlothiazide E. Triamterene ANSWER: B Which of the following nitrate preparations or dosage forms has the longest duration of action? A. Sublingual nitroglycerin B. Sublingual isosorbide dinitrate C. Oral isosorbide dinitrate D. Transdermal nitroglycerin patch E. Validolum ANSWER: D In order to prevent the development of tolerance, the pharmacist instructs the patient to: A. Apply the nitroglycerin patch every other day B. Switch to sublingual nitroglycerin when the patient's systolic blood pressure elevates to >140 mm Hg> C. Apply the nitroglycerin patch for 14 hours each and remove for 10 hours at night D. Use the nitroglycerin patch for acute episodes of angina only E. Apply the nitroglycerin patch 2 times per day ANSWER: C Before administering isosorbide mononitrate, a priority assessment would include: A. Serum electrolytes B. Blood urea nitrogen (BUN) and creatinine C. Blood pressure D. Level of consciousness E. Pressure within the heart ANSWER: C The patient asks how nitroglycerin should be stored while traveling. The pharmacist's best response would be: A. "You can protect it from heat by placing the bottle in an ice chest." B. "It's best to keep it in its original container away from heat and light." C. "You can put a few tablets in a resealable bag and carry in your pant's pocket." D. "It's best to lock them in the glove compartment of your car to keep them away from heat and light." E. "Keep the tablets locked in a safe place until you need them." ANSWER: B Patient teaching regarding sublingual nitroglycerin should include which of the following statements: A. "You can take up to five doses every 3 minutes for chest pain." B. "Chew the tablet for the quickest effect." C. "Keep the tablets locked in a safe place until you need them." D. "Sit or lie down after you take a nitroglycerin tablet to prevent dizziness." E. "You can protect it from heat by placing the bottle in an ice chest." ANSWER: D What is the best way to prevent tolerance to nitrates when using the transdermal patches? A. Leave the old patch on for 2 hours when applying a new patch B. Apply a new patch off for 24 hours once a week C. Leave the patch off for 24 hours once a week D. Remove the patch at night for 8 hours, and then apply a new patch in the morning E. Leave the patch off for 12 hours once a week ANSWER: D An annoying side effect of ACE inhibitors that may be minimized by switching to an angiotensin receptor blocking agent includes: A. Orthostatic hypotension B. A dry, nonproductive cough C. Fatigue D. Hypokalemia E. Hyperkalemia ANSWER: B Which of the following should not be taken concurrently with ACE inhibitors? A. Lasix B. Morphine C. Potassium D. Natrium E. Vicasolum ANSWER: C Labetalol and carvedilol are classified as: A. Beta-blocking agents B. Alpha1-blocking agents C. Combined alpha- and beta-blocking agents D. Calcium channel blockers E. Fibrinolytics ANSWER: C During assessment of a patient diagnosed with pheochromocytoma, the doctor auscultates a blood pressure of 210/110 mm Hg. The nurse would expect to administer which of the following medications? A. nadolol (Corgard) B. phentolamine (Regitine) C. dobutamine (Dobutrex) D. verapamil (Calan) E. validolum ANSWER: B The pharmacist would monitor for reflex tachycardia in a patient receiving which classification of antihypertensive agents? A. Calcium channel blockers B. Cardioselective beta-blockers C. Nonselective beta-blockers D. Direct-acting vasodilators E. Neuroleptics ANSWER: D ACE inhibitors and angiotensin receptor blockers both work to decrease blood pressure by: A. Preventing the formation of angiotensin II B. Enhancing sodium and water resorption C. Increasing the breakdown of bradykinin D. Inhibiting aldosterone secretion E. All of the above ANSWER: D