Neurological Assessment
advertisement
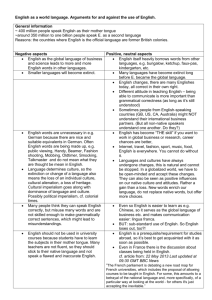
Neurological Assessment Dr. Belal Hijji, RN, PhD February 13 & 15, 2012 Learning Outcomes By the end of this lecture, students will be able to: 1. Describe the process of carrying out a neurologic assessment of an adult patient. 2 3 Neurologic Assessment 5 Components (4 are only included due to time restraints) • Examining the cerebral function – Mental status: Is the patient oriented to time, place, & person? – Intellectual function: Ask the patient to count backward from 100 or to subtract 7 from 100, then 7 from that, and so forth. – Thought content: During the interview, find out whether the patient’s thoughts are spontaneous, natural, clear, relevant, and coherent? Does the patient have any fixed ideas, illusions, or preoccupations? – Emotional status: Is the patient’s affect (external manifestation of mood) natural and even, or irritable and angry, anxious, apathetic or euphoric? Does his or her mood fluctuate normally, or does the patient unpredictably swing from joy to sadness during the interview? Are verbal communications consistent with nonverbal cues? 4 • Examining the cerebral function (Continued…) – Perception: Placing a familiar object (eg, key, coin) in the patient’s hand and having him or her identify it with both eyes closed is an easy way to assess tactile interpretation. – Motor ability: Ask the patient to perform a skilled act (throw a ball, move a chair). Successful performance requires the ability to understand the activity desired and normal motor strength. – Language ability: Does the patient answer questions appropriately? Can he or she read a sentence from a newspaper and explain its meaning? Can the patient write his or her name or copy a simple figure that the examiner has drawn? 5 • Examining the cranial nerves – I (olfactory): With eyes closed, the patient identifies familiar odors (coffee, tobacco). Each nostril is tested separately. – II (optic): Snellen eye chart (See next slide); visual fields; ophthalmoscopic examination. 6 What do the numbers mean in 20/20? The top number represents the distance between a person & chart. The bottom number represents how far away a person with normal vision can be from the chart and still read the letters in that line. 7 • A person with normal vision can read the 20/20 line from 20 feet away. A person with 20/10 vision has better-than-normal vision. He can read from 20 feet what a person with normal vision must move up to 10 feet away to read. Conversely, a person with 20/200 vision has poorer-than-normal vision. He must be closer to the chart – he must be only 20 feet away to clearly see what a normal person can read from 200 feet away. 8 • Examining the cranial nerves (Continued…) – (CN III, IV, VI): Hippus phenomenon: Apply pin light to pupils and note their brisk constriction followed by dilation and constriction. Normal doll’s eyes: Eyes deviate to side opposite from way head is turned. Abnormal doll’s eyes (eyes fixed): Damage to oculomotor nerves (CN III, IV, VI) or brainstem. –V (trigeminal): Ask patient to close eyes and tell you when he or she feels sensation on the face. Touch jaw, cheeks, and forehead with cotton wisp. Touch same areas with toothpick. Compare both bilaterally. – VII (facial): Sweet: Tip of the tongue. Sour []حامض: Sides of back half of tongue. Salty: Anterior sides and tip of tongue. Bitter: Back of tongue. Observe for symmetry while the patient performs facial movements: smiles, whistles, elevates eyebrows, frowns, tightly closes eyelids against resistance (examiner attempts to open them). 9 • Examining the cranial nerves (Continued….) –VIII (acoustic): Perform watch-tick test (left picture) by holding watch close to patient’s ear. The Weber test (See right picture below) is a hearing test for lateralization of sound. –IX (glossopharyngeal): Assess patient’s ability to discriminate between sugar and salt on posterior third of the tongue. –X (vagus): Depress a tongue blade on posterior tongue, or stimulate posterior pharynx to elicit gag reflex. Observe ability to cough, swallow, and talk. 10 • Examining the cranial nerves (Continued….) –XI (spinal accessory): Palpate and note strength of trapezius muscles while patient shrugs shoulders against resistance. Palpate and note strength of each sternocleidomastoid muscle as patient turns head against opposing pressure of the examiner’s hand. –XII (hypoglossal): While the patient protrudes the tongue, any deviation or tremors are noted. The strength of the tongue is tested by having the patient move the protruded tongue from side to side against a tongue depressor. 11 • Examining the motor system – Muscle strength: Ask the patient to flex or extend the extremities against resistance. Using a five-point scale, assess muscle strength. A 5, full range of motion against gravity and resistance; 4, full range of motion against gravity and a moderate amount of resistance; 3, full range of motion against gravity only; 2, full range of motion when gravity is eliminated; 1 indicates minimal contractile power—weak muscle contraction can be palpated but no movement is noted and 0, complete paralysis. – Coordination: Instruct the patient to pat his or her thigh as fast as possible with each hand separately. Then instruct him/ her to alternately pronate and supinate the hand as rapidly as possible. Lastly, ask the patient to touch each of the fingers with the thumb in a consecutive motion. Note speed, symmetry, and degree of difficulty. Have the patient touch the examiner’s extended finger and then his/ her own nose. This is repeated several times. This assessment is then carried out with the patient’s eyes closed. 12 • Examining the motor system (continued….) – Balance: Ask the patient to stand with feet together and arms at the side, first with eyes open and then with both eyes closed for 20 to 30 seconds. Slight swaying is normal, but a loss of balance is abnormal and is considered a positive Romberg test. 13 • Sensory examination: Eyes should be closed during exam. – Tactile sensation: Lightly touch a cotton wisp to corresponding areas on each side of the body. The sensitivity of proximal parts of the extremities is compared with that of distal parts. – Superficial pain perception: Ask the patient to differentiate between the sharp and dull ends of a tongue blade; using a safety pin is inadvisable because it breaks the integrity of the skin. – Position sense (proprioception): Ask the patient to close both eyes and indicate, as the great toe is alternately moved up and down, in which direction movement has taken place. 14