PowerPoint
advertisement
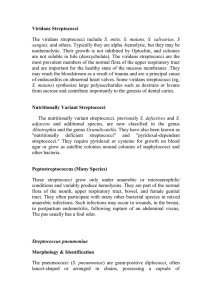
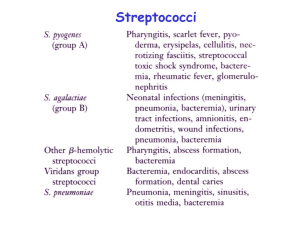
Streptococci & Enterococci David A. Wininger, MD Internal Medicine Residency Program Director Associate Professor, Clinical Internal Medicine Division of Infectious Diseases The Ohio State University Wexner Medical Center 614-293-3989 David.wininger@osumc.edu Learning Objectives Recognize the structure and microbial physiology of Streptococci and Enterococci and integrate this information with the human pathophysiologic correlates Define the structure and composition of Streptcocci and Enterococci Recognize the underlying genetic mechanisms of antibacterial resistance in Streptococci and Enterococci Describe the nature and mechanisms of action of Streptococcal and Enterococcal virulence factors Identify the normal human immune response to Streptococcal and Enterococcal infections Learning Objectives Recognize the epidemiology and ecology of Streptococcal and Enterococcal infections Describe and differentiate the principles of laboratory diagnosis for Streptococcal and Enterococcal infections Define the principles of infection prevention for Streptococcal and Enterococcal infections Recognize treatment options and accurately evaluate their role in the therapy of infections due to Streptococci and Enterococci Streptococci Gram Stain Catalase negative Classification of Streptococci Hemolytic pattern Alpha Beta Gamma (On sheep blood agar) Lancefield Groups: Cell wall carbohydrates by serologic tests Groups A-H, K-M, O-V Biochemical properties – see discussion by species Downloaded from: Principles and Practice of Infectious Diseases (on 17 January 2005 06:10 PM) Group A Streptococci (S. pyogenes) Sheep Blood Agar Plate Beta hemolysis Bacitracin inhibits growth PYR positive Downloaded from: Principles and Practice of Infectious Diseases (on 17 January 2005 06:10 PM) © 2004 Elsevier Group A Streptococci – Structure & Virulence Factors • M-protein • Lipoteichoic acid • F-protein • Capsule Group A Streptococci – Virulence Factors Toxins Pyrogenic exotoxins (SpeA, SpeB, SpeC, SpeF) Super-antigens Streptococcal Toxic Shock Syndrome, Scarlet Fever Enzymes Streptolysin S Lyses red blood cells Streptolysin O Basis of ASO test Streptokinases Lyses clots DNases Thins out pus C5a peptidase Block chemotaxis Group A Streptococci – Clinical Syndromes Acute Streptococcal Pharyngitis (“Strep Throat”) Group A Streptococci – Clinical Syndromes Scarlet Fever (Group A Strep strains producing SPE) Strawberry Tongue Desquamation (recovery phase) Group A Streptococci – Clinical Syndromes Impetigo Erysipelas CDC/Dr. Thomas F. Sellers/Emory University Cellulitis Group A Streptococci – Clinical Syndromes Rheumatic Fever & Rheumatic Carditis (Non-suppurative, post-streptococcal) Valvulitis (Mitral valve) Erythema marginatum Group A Streptococci – Clinical Syndromes Acute Post-Streptococcal Glomerulonephritis (APSGN) Post-Streptococcal Non-Suppurative Complications Rheumatic Fever Mostly strep throat M-types Acute Post-Streptococcal Glomerulonephritis (APSGN) Some after dermal infection Rationale for finishing full antibiotic course Penicillin G works in preventing Rheumatic Fever, BUT NOT APSGN Group B Streptococci (S. agalactiae) Laboratory Diagnosis: Culture shows a Beta-hemolytic Streptococci expressing “Group B” cell wall carbohydrate. Requires enriched media for optimal growth. Main Virulence factor: Capsule that prevents phagocytosis Epidemiology and Ecology: GI & GU tract colonization Vulnerable populations: Neonates, colonized women post-partum, older patients with cancer or diabetes Treatment: Easily treated with penicillins (i.e. Penicillin G, Ampicillin) Cephalosporins or Vancomycin for penicillin-allergic patients Group B Streptococci – Clinical Syndromes Clinical Disease in Peri-partum Period Neonatal sepsis (early and late) Neonatal meningitis Post-partum sepsis Prevention of Peri-partum Infections Pre-partum vaginal screening cultures Carriers receive antibiotics in labor Prophylaxis has reduced neonatal sepsis rates No vaccine is available Group B Streptococci – Clinical Syndromes Non-pregnant Adults Urinary tract infections Bacteremia and sepsis Soft tissue infections Musculoskeletal infections Mainly in patients compromised by: Age Diabetes mellitus Cancer Streptococcus pneumoniae Gram Stain Laboratory Diagnosis Downloaded from: Principles and Practice of Infectious Diseases (on 17 January 2005 06:09 PM) Gram (+) diplococci “Lancet shaped” Alpha-hemolytic Fastidious nutritional req. Susceptible to optochin Bile soluble © 2004 Elsevier S. pneumoniae – Structure & Virulence Factors Capsule Key virulence factor Anti-phagocytic For sero-typing Basis for vaccination Rough strains (avirulent) Other Virulence Factors Downloaded from: Principles and Practice of Infectious Diseases (on 17 January 2005 06:11 PM) Surface adhesins Pneumolysin (cytotoxin) sIgA Protease Teichoic Acid H2O2 © 2004 Elsevier S. pneumoniae – Clinical Syndromes Pneumococcal Pneumonia Downloaded from: Principles and Practice of Infectious Diseases (on 17 January 2005 06:09 PM) © 2004 Elsevier S. pneumoniae – Clinical Syndromes Lung Tissue No Pneumonia Acute Pneumococcal Pneumonia Acute Left Maxillary Sinusitis S. pneumoniae – Clinical Syndromes Other associated infections Acute Otitis Media Acute Bacterial Meningitis Bacteremia (with pneumonia or meningitis) Pneumococcal sepsis CDC S. pneumoniae – Treatment & Antibacterial Resistance Historically highly susceptible to penicillins Increasing rates of penicillin resistance due to altered penicillin binding proteins (PBPs). Serious disease Need susceptibilities to rule out penicillin resistance Primary empiric treatment usually consists of a 3rd Generation Cephalosporin (i.e. Ceftriaxone, Cefotaxime) Alternative treatments include: Vancomycin “Respiratory” (anti-pneumococcal) Fluroquinolones (i.e. Moxifloxacin, Levofloxacin) S. Pneumoniae – Normal Human Immune Response & Prevention Humoral immunity is key Anticapsular antibodies are protective Basis for vaccination Asplenics are at increased risk for serious sepsis!!! Vaccinate patients prior to elective splenectomy 23-valent vs. 13-valent conjugate vaccine Acute inflammatory response during disease Neutrophils Viridans Streptococci A heterogeneous group (not a single species) Often alpha hemolytic (“Viridis” – Green) S. mitior, S. mutans, and numerous others S. bovis bloodstream infections occult colon cancer!! Laboratory Diagnosis Culture “Viridans”- grouping is often enough Speciation Biochemicals and Mass Spectroscopy Epidemiology/Ecology Normal flora or colonizers of oral, GI and GU tracts Viridans streptococci Clinical Syndromes Endocarditis, bacteremia, dental abscess and intra-abdominal abscess. (No noteworthy virulence factors) Normal Human Immune Response/Prevention Ubiquitous organisms that take advantage of breaks in normal mucosal surfaces, triumphing due to sheer numbers and structural defects of the host (bad teeth, abnormal heart valves, prosthetic materials) but can be cleared with acute inflammation (neutrophils) Treatment Often penicillin susceptible, but resistance happens; can add aminoglycoside (for synergy) or use vancomycin while awaiting MIC’s. Enterococci Gram Stain E. faecalis and E. faecium Most common pathogenic species Laboratory Diagnosis Group D “strep” Usually alpha hemolytic (can vary!) Hardy: grows in wide temp range, pH range, salt concentrations, bile salts, aerobic and anaerobic conditions PYR positive Catalase negative Enterococci Ecology and Epidemiology Fecal flora (GI tract) and can colonize GU tract Overgrow when antibiotics eliminate other endogenous flora Spreads patient to patient Virulence Factors Adherence and biofilm formation (pili, surface proteins, etc.) Clinical Syndromes Urinary Tract Infections Bacterial endocarditis and other bacteremias Abdominal wounds and intra-abdominal infections Enterococci – Antibacterial Resistance & Treatment Inherent resistance to some classes (i.e. cephalosporins) Intrinsic decreased susceptibility to others (i.e. penicillins) Multidrug resistance, including to Vancomycin (VRE) Most commonly seen in E. faecium strains Treatment depends on susceptibility Penicillin G or Ampicillin Vancomycin Synergy with aminoglycosides (i.e. Gentamicin, Streptomycin) VRE – Mechanism of Resistance Vancomycin Resistant Enterococci (VRE) Antimicrobial Treatment Options Linezolid Daptomycin Tigecycline Quinupristin/Dalfopristin Infection Control Precautions Minimize antibiotic “pressure” Contact isolation precautions Summary – Streptococci & Enterococci Gram positive cocci in pairs or chains Targeted sites of infection depending on the species Pathogenesis merger of the sites of initial contact or colonization and the virulence features of the species Diagnosis based on Gram stain morphology, hemolysis pattern on Sheep Blood Agar and presence or absence of characteristic cell wall carbohydrates Penicillin optimal treatment for a subset of the strep species Enterococci Restricted antimicrobial treatment options Thank you for completing this module • • If you have any questions, write to me at david.wininger@osumc.edu Phone messages can be left at 614-293-3989. David Wininger, MD References Medical Microbiology, 7th Ed. Murray, Rosenthal & Pfaller; Chapter 19, pages 188-204; Chapter 20, pages 205-208. Survey We would appreciate your feedback on this module. Click on the button below to complete a brief survey. Your responses and comments will be shared with the module’s author, the LSI EdTech team, and LSI curriculum leaders. We will use your feedback to improve future versions of the module. The survey is both optional and anonymous and should take less than 5 minutes to complete. Survey