Streptococcaceae - Cal State LA
advertisement

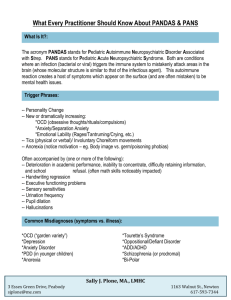
Streptococcaceae Streptococcaceae family Classification - Includes 7 genera: Streptococcus – a major cause of human infections Enterococcus – frequent cause of human infections Aerococcus – occasionally isolated from endocarditis, meningitis, or urinary tract infection Lactococcus – rare human pathogen Pediococcus – NF of lower GI tract, occasional isolate from abscesses Leuconostoc – infrequently isolated from blood, wounds, or abscesses Gemella – rare isolate of upper RT infection Streptococcaceae family We will focus only on Streptococci and Enterococci Preliminary differentiation is based on the hemolytic pattern they exhibit when grown on blood agar (,, or ) Serologic classification – was developed in the 1930’s by Lancefield. based on a precipitin reaction between a group specific antigen (C substance) which is a carbohydrate extracted from the cell wall, and specific antisera. test divides the Streptococci into serologic groups A through U. Some Strep don’t possess a group specific antigen and can’t be identified by this method. Streptococcaceae family Lancefield typing is used today primarily to distinguish between beta hemolytic Strep. Physiologic or biochemical characteristics can be used to differentiate species within the Streptococci and Enterococci genera and will be discussed later. In the future DNA probes and hybridization or PCR related tests will be used to differentiate the different species of Streptococci and Enterococci . Streptococcaceae family Morphology and General Characteristics Gram positive cocci that appear in pairs or chains (most often seen when grown in broth culture) because cell division occurs in only 1 plane. The length of the chain depends upon the firmness of attachment of the individual cells. Strep pneumoniae is a lancet shaped diplococcus. Strep quickly lose the ability to retain the crystal violet in the Gram stain as they age and will appear G- in old cultures. Gram stain of Strep. species grown in broth Strep pneumomiae Streptococcaceae family Many form capsules Streptococci are more fastidious than Staphylococci and require an infusion media or an enriched media such as blood agar to grow. Many are hemolytic on blood agar and the source of the blood (sheep vs. rabbits, etc.) may affect the type of hemolysis that the organism exhibits. Clinical labs all use 5% sheep RBCs in their blood agar. Types of hemolysis Streptococcaceae family The type of atmosphere in which the organism is grown may affect the type of hemolysis of Group A, beta hemolytic Strep. They produce two types of hemolysins: Streptolysin O which is oxygen labile Streptolysin S which is oxygen stable. Most strains produce both streptolysin S and O, but a few only produce streptolysin O which would not be detected if the organism is grown in the presence of oxygen. Stabbing the primary isolation plate after inoculation may provide the lower oxygen tension necessary to identify those strains that only produce streptolysin O. Streptococcaceae family Addition of trimethoprim-sulfamethoxazole (1.25 ug and 23.75 ug, respectively) to sheep blood agar may be used to suppress the growth of NF and allow better recovery of beta hemolytic Strep from cultures with a lot of NF such as those from the oropharynx. Strep are microaerophilic and for good growth require reduced oxygen tension such as what is found in a candle jar or in a CO2 incubator. Nutritionally deficient Strep may require vitamin B6 or pyridoxal for growth and may be found satelliting Staph aureus. Streptococcaceae family Strep pneumoniae is sensitive to the cold and may fail to grow in cultures that have been refrigerated. Biochemical identification Differentiation from other genera Other G+ cocci - Strep are catalase -, while Staph and Micrococci are catalase + Other cocci – Neisseria are G- cocci, but since Strep quickly lose their G + characteristic as they age, they may be confused with Neisseria. However, Neisseria are oxidase + and Strep are oxidase –. Streptococcaceae family Differentiation within the genus Once a clinical isolate is identified as a Streptococcus sp., before biochemical identification is done several things should be considered: Source of the specimen hemolytic Strep isolated from the respiratory tract are likely to be viridans group Strep which are NF, or Strep pneumoniae which may be a pathogen hemolytic Strep isolated from the GI tract is probably the NF Enterococcus. hemolytic Strep isolated from the respiratory tract are likely to be Strep pyogenes (group A) hemolytic Strep isolated from the genitourinary tract are likely to be Strep agalactiae (group B). Streptococcaceae family Differential diagnosis – certain Strep are more commonly associated with specific clinical syndromes group A with sore throat group B with neonatal meningitis Hemolysis – if the organism is beta hemolytic, test for Lancefield types A, B, C, D, F, and G Streptococcaceae family Group A (Strep pyogenes) biochemical differentiation (is hemolytic) Susceptibility to .04 units of bacitracin (done only on beta hemolytic Strep). Group A is sensitive and occasionally groups B, C or G are sensitive. SXT disks Resistance to SXT – both Groups A and B are resistant, others are sensitive Pyr test Production of pyroglutamyl aminopeptidase (pyr) – both group A Strep and Enterococci are +, others, including group B, are -. Streptococcaceae family Group B (Strep agalactiae) biochemical differentiation (is hemolytic) CAMP (Christie, Atkins, Munch-Peterson) test – tests for a diffusible, heat stable extracellular protein that enhances the hemolysis of sheep RBCs by the beta hemolysin of S. aureus. The synergistic action of the two hemolysins gives an arrowhead of hemolysis. This test is + for group B and – for all others. CAMP test Streptococcaceae family Hydrolysis of hippurate – due to the enzyme hippuricase. Group B is + while occasionally Enterococci and viridans group Strep are +, all others are -. Growth in 6.5% NaCl – Most group B are + as is Enterococcus, all others are -. Resistance to SXT – both Groups A and B are R, others are S Group D biochemical differentiation (may be , , or hemolytic). Includes both Enterococci and nonEnterococci species Bile esculin hydrolysis – all group D grow in the presence of bile esculin and are + for esculin hydrolysis, all other groups are - Bile esculin hydrolysis positive negative Streptococcaceae family To differentiate group D Enterococci from non-Enterococci: Pyr - + for Enterococci only Growth in 6.5% NaCl - + for Enterococci only To differentiate viridans group Streptococci from Strep pneumoniae (both are hemolytic): Optochin (ethyl hydrocupreine hydrochloride) susceptibility – optochin is a detergent that activates an autolytic enzyme that lyses the cell wall of Strep pneumoniae. Only Strep pneumoniae is S, viridans group Strep are R. Optochin disk (taxo P) test Streptococcaceae family Bile solubility- bile salts also activate the autolytic enzyme of Strep pneumoniae. Strep pneumoniae is soluble, viridans group Strep are not. The viridans group Strep don’t contain group specific C antigens and can’t be identified by serological tests. Most labs don’t speciate the viridans group Strep except for isolates from blood cultures or for epidemiologic purposes. Others ways to identify Streptococci Determination of serogroups – Lancefield typing based on C substance in cell wall Streptococcaceae family Determination of serotypes – Group A strep are divided into >80 different serotypes based on the type of M protein that they express. Quellung test – used in identifying the >84 different serotypes of Strep pneumoniae – is based on differences in the type of specific soluble substance (SSS) in their capsule. In the quellung reaction when specific antisera against SSS binds to the SSS, under the microscope it appears as if the capsule has swelled. This is due to a change in the refractive index that occurs when an antibody binds to its specific antigen. Quellung reaction Streptococcaceae family Mechanisms of pathogenicity Strep pyogenes – extracellular products Streptolysin S – alters membrane permeability and lyses RBCs, leukocytes, and other cells containing sterols in their membranes. Streptolysin O – forms membrane penetrating channels (porin) leading to membrane defects and cell lysis. In addition to RBCs, it is also cytotoxic to many tissue cells, and is particularly cardiotoxic. It is antigenic and during strep throat infections, but not during skin infections, antibodies are formed. An anti-streptolysin O titer (ASOT) can be used to diagnose a recent streptococcal infection. Streptococcaceae family Erythrogenic toxins – Act as superantigens and cause fever, are cardiotoxic, cause enhanced susceptibility to endotoxin shock, suppress antibody responses, and are indirectly responsible for the rash seen in scarlet fever. The rash is due to a delayed hypersensitivity reaction to other streptococcal antigens that is enhanced by the toxin. Toxin may be involved in causing a toxic shock like syndrome similar to the toxic shock syndrome caused by Staph. aureus. Streptokinase – causes lysis of fibrin clots by cleaving plasminogen to plasmin which then acts as a protease to lyse fibrin clots. Used in medicine to prevent heart attacks Streptococcaceae family Hyaluronidase DNAse – degrades accumulated inflammatory exudate DNA from leukocyte disintegration. Is antigenic and antibodies against it can be used to diagnose recent Strep infections, including skin infections. Strep pyogenes – cell associated factors M protein is a fibrous protein on the cell surface. Its presence is essential for virulence (it is the MAJOR virulence factor for group A Strep) and there are over 80 different types. is poorly immunogenic Antibodies, if made, are protective, long lasting, and type specific. Streptococcaceae family M protein protects the Strep from opsonization and, therefore, phagocytosis, by binding to fibrinogen. may also play a role in adherence. Some types of M protein can act as superantigens causing shock in the affected patient. Structure of Group A cell wall Streptococcaceae family Lipoteichoic acid (LTA) – mediates attachment to epithelial cells Hyaluronic acid capsule (note that this organism also produces a hyaluronidase). Antibodies to the capsule are not protective against infection. Strep agalactiae – extracellular products Hemolysin Toxin that either directly or indirectly causes an increase in vascular permeability in the lungs leading to respiratory distress Neuraminidase – cleaves sialic acid residues and may be involved in hyalin membrane disease (a lung problem) Hyaluronidase Streptococcaceae family Strep agalactiae – cell associated factors DNAse Protease Capsule – antibodies are type specific and protective LTA – for attachment Other beta hemolytic Strep – Some group C produce streptolysin O or S, streptokinase, or a capsule Some group G produce streptolysin O or S, streptokinase, DNAse, erythrogenic toxins or M protein Streptococcaceae family Strep pneumoniae – extracellular products Pneumolysin O – is cytolytic for RBCs and other tissue cells. is actually a cytoplasmic rather an extracellular protein. is only released when the bacteria lyse. acts as a porin to disrupt host cell membranes. Leukocidan Neuraminidase Hyaluronidase IgA protease - cleaves IgA Strep pneumoniae – cell surface structures Capsule – is the most important virulence factor. there are > 80 different types and antibodies against the capsule are type specific and protective. Strep pneumoniae with mucoid colonies due to capsule Streptococcaceae family Clinical significance – Strep are responsible for a wide variety of diseases. Many of the infections are characterized by pus producing lesions (suppurative) and manifestations suggesting toxemia (toxin involvement). Infants tend to be more susceptible to Strep infections with prolonged, low grade infections. Rarely do nephritis and rheumatic fever follow. In contrast, older children and adults tend to get more acute and self-limited infections, with nephritis and rheumatic fever as occasional complications (these are non-suppurative sequelae to be discussed later). Streptococcaceae family Beta hemolytic groups A, B, and C are the most virulent Strep, with the greatest number of Strep infections due to group A. Most alpha hemolytic and non hemolytic Strep are much less virulent. Alpha hemolytic Strep (viridans group Strep) are found as NF in the RT and GI tract. They are the most common cause of subacute bacterial endocarditis. In contrast, Strep pneumoniae infections are a leading cause of death throughout the world, particularly in the elderly and the very young. Streptococcaceae family Strep pyogenes infections Streptococcal pyoderma or impetigo – is a superficial skin infection characterized by a vesicular rash that becomes pustular and in later stages is covered with a thick crust. Staph aureus may be a secondary invader. is endemic in tropical areas and is caused by M serotypes different than those that cause pharyngitis. is spread by close, direct contact disease starts with skin colonization, followed by invasion through abrasions type specific antibodies to M are made, but antibodies to streptolysin O are uncommon The most serious complication is acute glomerulonephritis which may occur 2-3 weeks post infection. Impetigo Strep pyogenes infections Erysipelas – a diffuse, erythematous skin infection that is most often on the face and occurs following pharyngitis Strep pyogenes infections Wound infections – occasionally causes wound infections following trauma. Usually due to simple contamination of the wound. Cellulitis – an infection of subcutaneous tissue which may be accompanied by lymphangitis and abscess formation. Patients typically exhibit chills, fever, and marked signs of toxicity. Necrotizing fasciitis (”flesh eating bacteria”) – when there is destruction of the fibrous tissue deep in the skin. The sheath of tissue that covers the muscle is destroyed. Destruction is due to release of exotoxin A that stimulates production of cytokines damaging endothelial lining and leaking fluid into the extravascular space causing diminished blood flow, tissue hypoxemia, and tissue death. Can also be caused by Staph aureus and other bacteria. Necrotizing fasciitis Necrotizing fasciitis Flesh removed to stop spread Gangrene Strep pyogenes infections Myositis – is a result of Strep invasion of muscle tissue resulting in extensive muscle necrosis and overwhelming sepsis. This condition is usually fatal. Strep pyogenes infections Pharyngitis – Strep or sore throat – most common disease caused by Strep pyogenes. Is characterized by an abrupt onset of sore throat, malaise, headache and fever. The throat (pharynx) is erythematous (red) with a grayishwhite exudate. The tonsils and lymph nodes are enlarged and the tonsils may become infected chronically. Spread to the sinuses and middle ear may also occur. Disease is spread by droplets of respiratory secretions or via food or water. Secondary effects may include rheumatic fever (to be discussed later). Disease is usually self-limited, but penicillin should be used to prevent secondary complications from occurring. Pharyngitis Strep pyogenes infections Scarlet fever – results from URT infection with group A Strep that has been lysogenized by a phage which carries the gene for the erythrogenic toxin. Symptoms are similar to pharyngitis plus an erythematous rash that first appears on the upper chest and spreads to the rest of the body. Lasts about 1 week and is followed by several weeks of extensive desquamation of the skin. The tongue is also affected with red spots on a yellowishwhite colored tongue (strawberry) followed by peeling and a red beefy colored (raspberry) tongue. Immunity to the toxin is demonstrated by the Dick test – inject toxin and if local antibodies are absent, the patient will develop a local erythema. The erythrogenic toxin may also be involved in causing a toxic-shock like syndrome. Scarlet fever Strep pyogenes infections Non-suppurative complications of Strep infections – no purulent inflammatory response is seen and the diseases can’t be diagnosed by culturing the organism which is no longer present Rheumatic fever – is an inflammatory disease that may involve the heart, joints, subcutaneous tissue, and the CNS. It occurs primarily in children 6-15 years of age at a time period of 1-5 weeks after Strep throat, but not pyoderma. The major manifestations are polyarthritis, carditis, chorea, and erythema marginatum. Carditis can involve all layers of the heart (characteristic lesions are called Aschoff bodies or nodules) and can lead to rheumatic heart disease which is characterized by chronic, progressive damage to the heart and possibly death. The mechanism by which rheumatic fever is initiated is an autoimmune phenomena involving cross-reacting antibodies made against Strep, that react with self tissues. Rheumatic fever Antibody binding attracts host reactive cells, complement gets activated and this leads to cellular damage. Diagnosis is done using ASOT assays. This complication can be prevented by treating Strep throat with penicillin. Rheumatic fever Strep pyogenes infections Acute glomerulonephritis – this may occur 2-3 weeks following pharyngitis or pyoderma. It is characterized by edema, hypertension, headache, malaise, circulatory congestion, and hematuria. It is only associated with specific nephritogenic M serotypes of group A Strep. It is probably an immune complex disease resulting from deposition of circulating immune complexes of Strep antigens and antibodies in the basement membrane of the glomeruli of the kidney. Damage is probably due to the attraction of host reactive cells and subsequent complement activation. Streptococcaceae family Strep agalactiae (group B) infections – Group B Strep are part of the NF of the adult vagina, urethra, and rectum, and, occasionally, the pharynx. appears to be sexually transmitted. In adults it rarely causes URT infections, meningitis, bacteremia, and endocarditis. It used to be a major cause of puerperal sepsis (postpartum sepsis). The most serious cases of group B infections occur in the newborn. There are two types of disease in the newborn. Early onset disease – occurs when babies become infected in utero or at birth, with the organism gaining access through the respiratory tract. The disease has a high mortality rate and is characterized by respiratory disease and bacteremia. Septicemia and meningitis may also occur. Strep agalactiae (group B) infections Late onset disease – occurs 7-10 days after birth and the baby probably acquires the organism by direct contact with mucosal surfaces. The disease is characterized by meningitis or osteomyelitis and possibly bacteremia. The mortality rate is high, but lower than that for the early-onset disease. Other Streptococcal group infections – Group C – occasionally causes diseases similar to those caused by group A, but without the nonsuppurative sequelae complications. Group F – tend to form abscesses in patients with underlying disease or trauma. Streptococcaceae family Group D Enterococci and non-enterococci – are part of the NF of the GI tract, but are a common cause of UT infections, subacute bacterial endocarditis, abdominal abscesses, and wound infections. Finding Strep bovis in the blood suggests that the surfaces of the colon have been compromised and this has been associated with carcinoma of the colon. An early screen for colon cancer? Group G – rarely associated with disease except in those with underlying conditions such as tumors. In these individuals group G Strep can cause the same diseases associated with groups A and B Strep Streptococcaceae family Viridans group Strep – are NF of the RT, GI tract, and genital tract. Are the most common cause of subacute bacterial endocarditis where they colonize damaged heart valves. Strep mutans plays a role in dental decay. Strep pneumoniae – are found as part of the NF in the URT in 15% of children and 5% of adults. This carrier state is sporadic. It is probably a pathogen when it is the most predominant organism isolated. Pneumonia – is the leading cause of bacterial pneumonia, particularly in the very young, the elderly, and those with immunological deficiencies. Bacteremia is common and meningitis may occur. The mortality rate is 5-7%. Streptococcaceae family Streptococcaceae family Strep pneumoniae infections Meningitis – Not as common as other causes of meningitis except in children under 1 year of age where it is the second most common cause of meningitis. The mortality rate in this group is high. Otitis media – is the most common cause of middle ear infection in children (1/3 of cases). May also cause purulent sinusitis and peritonitis. Otitis media Streptococcaceae family Antimicrobial susceptibility – Use penicillin for groups A, B, C, and G. Enterococcus and other group D – must do sensitivity testing. Use erythromycin for individuals allergic to penicillin. Susceptibility testing is not necessary. There are now strains of Enterococcus faecalis that are resistant to all known antibiotics. Viridans group Strep – do sensitivity testing Streptococcaceae family Strep pneumoniae – used to always use penicillin, but now there are resistant strains, so sensitivity testing is necessary. Other treatments There is a polyvalent vaccine for strains of Strep pneumoniae that are most likely to cause pneumonia. is given to those most likely to be infected, i.e., young and old individuals and those with chronic respiratory problems.