neuro 566 to 591 [3-26
advertisement

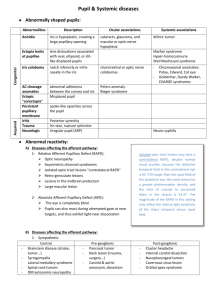
Neuro Pg 566-591 Eye Movements and Pupillary Control Extraocular muscles – muscles that move eye in socket Internal ocular muscles – control pupillary size and lens accommodation Eye movement disorders and pathways separated into o Nuclear and infranuclear pathways – involve brainstem nuclei of CN III, IV, and VI; peripheral nerves arising from these nuclei; and eye movement muscles o Supranuclear pathways – involve brainstem and forebrain circuits that control eye movements through connections with nuclei of CN III, IV, and VI Extraocular Muscles, Nerves, and Nuclei Rectus muscles originate in common tendonous ring at orbital apex and insert onto sclera Superior oblique originates on sphenoid bone in posterior medial orbit and passes anteriorly through trochlea (pulley-like fibrous loop on medial superior orbital rim); inserts on superior surface of eye to produce intorsion Inferior oblique has no trochlea; originates along anterior medial orbital wall and inserts on iniferior surface of eye to produce extorsion Superior oblique causes depression when eye adducted; inferior oblique causes elevation when eye adducted Inferior division of oculomotor nerve supplies medial rectus, inferior rectus, and inferior oblique muscles; carries preganglionic PNS fibers to pupillary constrictor and ciliary muscles Superior division of oculomotor nerve supplies levator palpebrae superioris and superior rectus CN III, CN IV, CN VI, and CN XII make up somatic motor column of CN nuclei; all lie near midline, adjacent to ventricular system, and fibers exit brainstem ventrally near midline (except CN IV which exits dorsally) Fascicles of oculomotor nerve exit brainstem as CN III in interpeduncular fossa between posterior cerebral and superior cerebellar arteries Edinger-Westphal nuclei, containing preganglionic PNS fibers, form V shape as they curve over dorsal aspect of oculomotor nuclei and fuse anteriorly in midline PNS fibers controlling pupil constriction run in superficial and medial portion of oculomotor nerve as it travels in subarachnoid space; susceptible to compression from aneurysms, particularly in posterior communicating artery Oculomotor nerve enters cavernous sinus and continues to orbit via superior orbital fissure Nuclear lesion of oculomotor nucleus can’t cause unilateral ptosis, unilateral dilated unresponsive pupil, or unilateral superior rectus palsy, since crossing fibers traverse oculomotor nucleus before exiting in fascicles Trochlear nuclei bounded ventrally by fibers of medial longitudinal fasciculus; only cranial nerves to exit brain dorsally; exit brainstem in completely crossed fashion; travel caudally for short distance and cross to opposite side before exiting at level of anterior medullary velum, where they are susceptible to compression from cerebellar tumors; very thin and relatively easily damaged by shear injury from head trauma o Travel through subarachnoid space along underside of tentorium cerebelli and enter cavernous sinus to reach orbit via superior orbital fissure Abducens nuclei on floor of 4th ventricle under facial colliculi in mid-to-lower pons; fibers travel ventrally to exit at pontomedullary junction; nerve exits dura to enter Dorello’s canal, running between dura and skull, under petroclinoid ligament; passes over petrous tip of temporal bone to reach cavernous sinus (long vertical course explains why it is highly susceptible to downward traction injury produced by elevated intracranial pressure) o Enters orbit via superior orbital fissure Diplopia Diplopia can be caused by mechanical problems (orbital fracture with muscle entrapment), disorders of EOMs (thyroid disease or orbital myositis (orbital pseudotumor)), disorders of neuromuscular junction (myasthenia gravis), disorders of CN III, IV, VI, and their central pathways Can occasionally be caused by disorders involving supranuclear oculomotor pathways such as internuclear ophthalmoplegia (INO), skew deviation, and ingestion of toxins (alcohol or anticonvulsant meds) If diplopia goes away when patient covers one eye, it’s caused by eye movement abnormality Monocular diplopia or polyopia (3+ images) can be caused by ophthalmological disease, disorders of visual cortex, or psychiatric conditions, but not eye movement abnormalities Image further from midline and towards direction of attempted gaze is always one seen by abnormal eye (when looking at object to right, if one eye doesn’t move to right, it will form second image that appears displaced to the right) Red glass test – transparent piece of red glass or plastic held over one eye and small white light held directly in front of patient; image seen by eye behind glass is red, and other is white; patient can then report locations of red and white images Exotropia – abnormal lateral deviation of one eye Esotropia – abnormal medial deviation of one eye Hypertropia – vertical deviation of one eye Cover-uncover test – visual input helps maintain eyes yoked in same direction, so when an eye covered while looking in direction of weak muscle, it may drift slightly back toward neutral position (exophoria or esophoria) Strabismus – dysconjugate gaze Amblyopia – decreased vision in one eye Oculomotor Palsy (CN III) Only remaining movements of eye are some abduction and some depression and intorsion; eye may stay down and out at rest Complete ptosis because of paralysis of levator palpebrae superior Pupil dilated and unresponsive to light Diplopia worse when looking at near objects and better when looking at distant objects Diagonal diplopia that is most severe when looking up and medially with affected eye Commonly caused by diabetic neuropathy or other microvascular neuropathy associated with hypertension or hyperlipidemia or head trauma Can be caused by compression of nerve by intracranial aneurysms, most often arising from junction of posterior communicating artery with internal carotid artery o Aneurysms classically cause painful oculomotor palsy that involves pupil; consider them to have PComm aneurysm until proven otherwise o PNS fibers located near surface of nerve, and if nerve compression severe enough to cause complete paralysis of muscles innervated by CN III, pupillary fibers should be involved as well o Partial oculomotor palsy that spares pupil and is painful – suspect aneurysm Can be damaged by abnormalities in subarachnoid space, cavernous sinus, or orbit (infection, tumor, or venous thrombosis) Herniation of medial temporal lobe over edge of tentorium cerebelli can compress oculomotor nerve Ophthalmoplegic migraine causes reversible oculomotor nerve palsy (usually seen in children) Lesions of midbrain such as lacunar infarcts or other infarcts involving oculomotor nucleus or exiting nerve fascicles, can cause oculomotor palsy Painless and complete oculomotor palsy that spares pupil not caused by aneurysms (with rare exceptions); usually caused by diabetes or other microvascular neuropathy Lesions of CN III can sometimes affect superior division or inferior division in isolation o Lesion of superior division causes weakness of superior rectus and levator palpebrae superior; more often caused by mass in or near orbit rather than diabetic neuropathy Trochlear Palsy (CN IV) Produces depression and intorsion of eye; causes vertical diplopia; if weakness severe, may show hypertropia o May be extorsion of eye Improve diplopia by looking up (chin tuck) and by tilting head away from affected eye Vertical diplopia most severe when affected eye looking downward and toward nose Have patient look at horizontal line or pen; lower line will be tilted with CN IV palsy; 2 lines form an arrowhead pointing toward affected side Head movement always in direction of action normally served by affected muscle (right trochlear palsy: head held down and tilted to left; normal action of right superior oblique is depression and intorsion of eye) Trochlear nerve most commonly injured cranial nerve in head trauma; can also be caused by pathology in subarachnoid space, cavernous sinus, or orbit; microvascular damage to nerve by diabetes Vascular or neoplastic disorders in midbrain or near tectum (pineal gland or anterior cerebellum) can also affect trochlear nuclei or nerve fascicles Congenital 4th nerve palsy fairly common cause of superior oblique weakness; latent for years except minor head tilt and can later decompensate, leading to diplopia in adult Skew deviation – vertical disparity in position of eyes of supranuclear origin; typically but not always relatively constant in all positions of gaze; can be caused by lesions of cerebellum, brainstem, or inner ear Abducens Palsy (CN VI) Horizontal diplopia; in some cases esotropia of affected eye Diplopia better when viewing near objects and worse when viewing far objects Milder palsy may be incomplete burial of sclera on lateral gaze Because of long course along clivus and over sharp ridge of petrous temporal bone, nerve particularly susceptible to injury from downward traction caused by elevated intracranial pressure; early sign of supratentorial or infratentorial tumors, pseudotumor cerebri, hydrocephalus, and other intracranial lesions Can be unilateral or bilateral, even if caused by increased intracranial pressure May result from microvascular neuropathy as seen in diabetes Pontine infarcts or other disorders affecting exiting abducens fascicles in pons cause weakness in ipsilateral eye o Lesions of nucleus produce horizontal gaze palsy in direction of lesion (movements of both eyes decreased in that direction) o Lesions of nucleus often affect nearby fibers of CN VII in facial colliculus, resulting in ipsilateral facial weakness Pupils and Other Ocular Autonomic Pathways Pupillary constriction – light activates retinal ganglion cells, which project to both optic tracts because of fibers crossing in optic chiasm o o Fibers in extrageniculate pathway continue in brachium of superior colliculus to reach pretectal area After synapsing, axons continue bilaterally to Edinger-Westphal nuclei, which contain preganglionic PNS Some crossing fibers travel in posterior commissure o Preganglionic PNS travel bilaterally from Edinger-Westphal nuclei via CN III to ciliary ganglia in orbit o Postganglionic PNS continue to pupillary constrictor muscles o Causes consensual response in other eye as well because info crosses bilaterally During accommodation response (when shifting focus from far to near) results in pupillary constriction, accommodation of lens ciliary muscle, convergence of eyes Viewing close object Viewing distant object o o Visual signals relayed to visual cortex; pretectal nuclei activated, causing bilateral pupillary constriction mediated by PNS pathways shown above Contraction of ciliary muscle mediated by PNS of same pathway; lens normally under tension from suspensory ligament; ciliary muscle acts as sphincter When contracted, causes suspensory ligament to relax, producing rounder, more convex lens shape Descending SNS pathway from several hypothalamic nuclei travels in lateral brainstem to T1-T2 o o o o Same location in brainstem as spinothalamic tract (associated with Horner’s syndrome) Preganglionic SNS join paravertebral sympathetic chain via white rami communicantes Axons ascend to synapse in superior cervical ganglion Postganglionic SNS go through carotid plexus along walls of internal carotid artery to cavernous sinus, ultimately reaching pupillary dilator muscle SNS pathway important in controlling smooth muscle superior tarsal muscle (Müller’s), which elevates upper lid, causing wide-eyed stare in conditions of increased SNS outflow o Also innervate smooth muscle orbitalis (Müller’s), which prevents eye from sinking back in orbit, as well as cutaneous arteries and sweat glands in face and neck o Impaired in Horner’s syndrome Pupillary Abnormalities Can be caused by peripheral or central lesions, SNS or PNS lesions, disorders of iris muscle or visual pathways Anisocoria – pupillary asymmetry Oculomotor nerve lesion – can cause impaired pupillary constriction, resulting in unilateral dilated pupil o Decreased or absent direct response when light shone in affected eye o Decreased or absent consensual response when light shone in opposite eye Horner’s syndrome – disruption of SNS to eye and face; unilateral ptosis (loss of innervation to Müller’s smooth muscle in upper lid) , miosis (pupil constriction; loss of innervation to pupillary dilator), and anhidrosis o Pupil still has direct and consensual constricting response to light; dilation lag relative to normal pupil when light removed, and pupillary size reduced o Testing ciliospinal reflex (pinch neck to activate SNS outflow, causing pupillary dilation on normal side, but not side with Horner’s syndrome) o Preganglionic lesions can be distinguished from postganglionic lesions using hydroxyamphetamine eye drops, which stimulate norepi release and dilate pupil for preganglionic (not postganglionic) lesions o Postganglionic lesions not usually associated with anhidrosis because SNS for sudomotor innervation diverge from oculosympathetic pathway before superior cervical ganglion Pontine pupils – large bilateral lesions of pons; both pupils small but reactive to light; bilateral disruption of descending SNS pathways Afferent pupillary defect (Marcus Gunn pupil) – direct response to light in affected eye decreased or absent, consensual response of affected eye to light normal o Caused by decreased sensitivity of affected eye to light resulting from lesions of optic nerve, retina, eye o Lesions at or behind optic chiasm would affect inputs from both eyes, and so wouldn’t do this o Normal pupil will dilate if shining light into affected eye o Hippus – normal brief oscillation of pupil size that sometimes occurs in response to light Ptosis Benign (essential, physiological) anisocoria – slight pupillary asymmetry of less than 0.6 mm seen in 20% of general population; no associated abnormal findings Pharmacological miosis and mydriasis – opiates cause bilateral pinpoint pupils o Barbiturate overdose can cause bilateral small pupils (mimic pontine lesions) o Anticholinergic agents affecting muscarinic receptors (atropine) cause dilated pupils o Pupillary dilation may be unilateral if one eye exposed topically (mimics uncal herniation) o Pilocarpine causes pupillary constriction in PNS lesions but can’t overcome pharmacological muscarinic blockade (helps for atropine overdose) Light-near dissociation – pupils constrict much less in response to light than to accommodation o Argyll Robertson pupil – associated with neurosyphilis; pupils small and irregular o Seen in diabetes and Adie’s myotonic pupil; part of Parinaud’s syndrome (associated with compression of dorsal midbrain) Adie’s myotonic pupil – degeneration of ciliary ganglion or postganglionic PNS neurons, resulting in mid-dilated pupil that reacts poorly to light; some constriction elicited with accommodation response, but pupil remains constricted and dilates very slowly (myotonic pupil) Midbrain corectopia – lesions of midbrain cause unusual pupillary abnormality in which pupil assumes irregular, off-center shape Frontalis muscle is accessory eye opener; orbicularis oculi performs eye closure; both innervated by CN VII Pseudoptosis – redundant skin folds associated with aging Ptosis in Horner’s syndrome mild; oculomotor lesions cause mild to severe ptosis Causes of bilateral ptosis without loss of consciousness include nondominant parietal lobe stroke, severe neuromuscular disorders, dorsal lesions of oculomotor nuclei affecting central caudal nucleus, voluntary eye closure associated with photophobia Cavernous Sinus and Orbital Apex CN III, IV, and VI all pass through this region Cavernous sinus consists of collection of venous sinusoids located on either side of pituitary that receives venous blood from eye and superficial cortex and ultimately drains via several pathways into internal jugular vein o Between periosteal and dural layers of dura mater o Surrounds carotid siphon, CN VI (closest to carotid), CN III, CN IV, and CN V1 (ophthalmic), which run on lateral wall Above pass forward to enter orbital apex via superior orbital fissure o CN V2 (maxillary) skirts lower portion of cavernous sinus and runs through it for short distance before exiting via foramen rotundum o SNS fibers traveling in carotid plexus traverse cavernous sinus o CN II lies just above cavernous sinus and enters orbital apex (region where nearly all nerves, arteries, and veins of orbit converge before communicationg with intracranial cavity via optic canal and superior orbital fissure) via optic canal Cavernous Sinus Syndrome and Orbital Apex Syndrome Orbital apex lesions often associated with proptosis due to mass effect in orbit; CN V2 spared since it exits cranium via foramen rotundum Cavernous sinus syndrome can affect V2; Horner’s syndrome can occur because of disruption of ocular SNS, but may be difficult to appreciate in setting of 3rd nerve lesion (sometimes apparent in affected eye in dark) Both can be affected by single lesion since they are contiguous Impaired venous drainage in both/either disorder can cause vascular engorgement of orbital structures Cavernous carotid aneurysms or fistulas, abducens often involved first because it lies closest to carotid artery In pituitary apoplexy, there is hemorrhage within pituitary gland, often in setting of pituitary tumor, which can extend into adjacent cavernous sinus Medical emergencies that require prompt recognition, diagnosis, and treatment Supranuclear Control of Eye Movements Saccades – rapid eye movements; bring targets of interest into field of view; vision transiently suppressed during saccadic eye movements; only type of eye movement that can easily be performed voluntarily Smooth pursuit – eye movements ont under voluntary control; allow stable viewing of moving objects Vergence – eye movements maintain fused fixation by both eyes as targets move toward or away from viewer Reflex – include optokinetic nystagmus and vestibule-ocular reflex o Nystagmus – rhythmic form of reflex eye movements composed of slow eye movements in one direction interrupted repeatedly by fast saccade-like eye movements in opposite direction Medial longitudinal fasciculus (MLF) interconnects oculomotor, trochlear, abducens, and vestibular nuclei; yokes eyes together, resulting in conjugate gaze in all directions o Abducens nucleus is horizontal gaze center, controlling horizontal movement of both eyes in direction ipsilateral to side of nucleus o Some neurons in abducens nucleus project to ipsilateral lateral rectus muscle, while others project via MLF to contralateral oculomotor nucleus, which in turn activates contralateral medial rectus muscle In pontine tegmentum near abducens nucleus, paramedian pontine reticular formation (PPRF) provides inputs from cortex and other pathways to abducens nucleus, resulting in lateral horizontal gaze Brainstem Lesions Affecting Horizontal Gaze Lesions of abducens nerve cause impaired abduction of ipsilateral eye (CN VI palsy); lesions of abducens nucleus produce ipsilateral lateral gaze palsy (involves both eyes through MLF) Lesions of PPRF cause ipsilateral lateral gaze palsy With lesions of MLF, there is nystagmus of opposite eye (mechanisms trying to bring eyes back into alignment) Internuclear ophthalmoplegia (INO) – neurologic syndrome produced by MLF lesion o Side of INO is side of lesion in MLF o Since ascending MLF crosses almost immediately after leaving abducens nucleus, side of INO is also side on which eye adduction is weak o Eye adduction on affected side impaired with horizontal gaze but often spared during convergence because inputs to oculomotor nucleus mediating convergence arise from pretectal region and don’t travel in caudal MLF If lesion involves both MLF and adjacent abducens nucleus or PPRF, there is combination ipsilateral INO and ipsilateral lateral gaze palsy (one-and-a-half syndrome); ipsilateral eye cannot move at all horizontally, and contralateral eye loses half its movements, preserving only ability to abduct Brainstem Circuits for Vertical and Vergence Eye Movements Brainstem centers controlling vertical eye movements located in rostral midbrain reticular formation and pretectal area; ventral portion mediates downgaze, and dorsal region mediates upgaze o Rostral interstitial nucleus of MLF mediates downgaze Progressive supranuclear palsy associated with impaired vertical eye movements and midbrain atrophy In locked-in syndrome, large pontine lesions can disrupt bilateral corticospinal tracts and abducens nuclei, eliminating body movements and horizontal eye movements; sometimes vertical eye movement centers in midbrain spared, allowing patient to communicate entirely through vertical eye movements Vertical eye movements normally closely coordinated with movement of upper eyelids except during blinking; coupling mediated by M-group of neurons located in midbrain near nuclei for vertical eye movements o Eyelid abnormalities in Parinaud’s syndrome likely arise from damage to M-group of neurons in rostral midbrain Convergence of eyes produced by medial recti; divergence by lateral recti o Separate pools of neurons in midbrain reticular formation mediating either convergence or divergence o Vergence movements under control of descending inputs from visual pathways in occipital and parietal cortex and constitute part of accommodation response Parinaud’s Syndrome Constellation of eye abrnomalities usually seen with lesions compressing dorsal midbrain and pretectal area o Impairment of vertical gaze, especially upgaze; may be due to compression of dorsal part of vertical gaze center o Large, irregular pupils that don’t react to light but sometimes may react to near-far accommodation; light-near dissociation results from disruption of optic tract fibers traveling to Edinger-Westphal nuclei via dorsal pathways including posterior commissure, while fibers descending from visual cortex take different route and are spared o o Eyelid abnormalities – bilateral lid retraction (Collier’s sign) or tucking to bilateral ptosis Impaired convergence and sometimes convergence-retraction nystagmus; eyes rhythmically converge and retract in orbits, especially on attempted upgaze Commonly caused by pineal region tumors, hydrocephalus, MS or vascular disease of midbrain and pretectal area Hydrocephalus can cause dilation of suprapineal recess of 3rd ventricle, which pushes downward onto collicular plate (tectum) of midbrain; produces bilateral setting-sun sign (eyes deviated inward and downward) o Can be seen in thalamic hemorrhage as well Control of Eye Movements by Forebrain Descending cortical pathways travel either directly to brainstem centers for horizontal, vertical, or convergence eye movements or via relays in midbrain superior colliculi Frontal eye fields – junction between superior frontal sulcus and precentral sulcus; overlap premotor and prefrontal cortices because of roles in eye movements and selective attention o Generate saccades in contralateral direction via connections to contralateral PPRF More posterior cortical regions of parieto-occipito-temporal cortex primarily responsible for smooth pursuit movements in ipsilateral direction via connections with vestibular nuclei, cerebellum, and PPRF o Makes some contribution to contralateral eye movements Cortical descending control of eye movements heavily influenced by visual inputs arriving at primary visual cortex and visual association cortex Basal ganglia play role in modulatory control of eye movements Right-Way Eyes and Wrong-Way Eyes Lesions of cerebral hemispheres normally impair eye movements in contralateral direction, often resulting in gaze preference toward side of lesion; typically accompanied by weakness contralateral to cortical lesion (if corticospinal pathways involved), so eyes look away from side of weakness (right-way eyes) Wrong-way eyes (looking toward side of weakness) caused by seizure activity in cortex (drives eyes in contralateral direction because of activation of frontal eye fields while also causing abnormal or decreased movements of contralateral side of body because of involvement of motor association cortex and other structures) o Thalamic hemorrhage can disrupt corticospinal pathways of internal capsule, causing contralateral weakness, but may also cause eyes to deviate toward side of weakness; thalamic lesions usually accompanied by deep coma Lesions of pontine basis and tegmentum can cause wrong-way eyes because of disruption of corticospinal fibers causing contralateral hemiplegia, while involvement of abducens nucleus or PPRF causes ipsilateral gaze weakness Cerebellar, Vestibular, and Spinal Control of Voluntary and Reflex Eye Movements Cerebellum, vestibular nuclei, and cervical spinal proprioceptors influence ongoing voluntary eye movements and contribute to several forms of reflex eye movements Optokinetic nystagmus (OKN) – can elicit this by moving thick ribbon with vertical stripes (OKN strip) horizontall in front of eyes; eyes alternate between smooth pursuit movements in direction of stripe movement and backup (corrective) saccades opposite direction of stripe movement in attempt to stabilize image o Slow phase (smooth pursuit) mediated by ipsilateral posterior cortex, with connections to vestibular nuclei and flocculonodular lobe of cerebellum projecting to PPRF and abducens nuclei; disrupted by lesions in smooth pursuit pathways o Fast phase (saccadic) mediated by frontal eye fields projecting ultimately to contralateral PPRF; lesions of frontal cortex or anywhere in saccadic pathway disrupt fast phase of OKN Vestibule-ocular reflex (VOR) stabilizes eyes on visual image during head and body movements o Inputs from vestibular nuclei, especially medial vestibular nuclei, travel in MLF to control extraocular nuclei o In patients who are comatose and therefore lack visual fixation; integrity of brainstem circuits mediating VOR tested with oculocephalic maneuver to elicit doll’s eyes or with cold water calorics o In normal awake individual, cerebellar circuits involving flocculus and nodulus (vestibulocerebellum) enable visual fixation to overcome VOR; oculocephalic testing won’t produce doll’s eyes o Visual fixation can suppress nystagmus evoked by caloric testing o In VOR suppression test, patients fixate on object moving with head as it rotates (put straw in patient’s mouth and ask them to focus on end of straw as they turn their head back and forth); presence of nystagmus indicates cerebellar dysfunction Proprioceptive inputs help stabilize eyes on visual image, especially during head and neck movements