7. practice 2011
advertisement

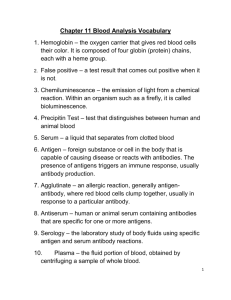
Immunological techniques based on primary antigen-antibody reactions (2.) 7th week practice immunoblot immunhistochemistry flow cytometry The sensitivity of immunoassays Characterization of antigens by Western blotting Anode(+) steps: 1. sample preparation (cells, tissues) 2. gel electrophoresis 3. blotting 4. labeling 5. development Cathode(-) usage: identification of defined components from protein mixtures by antigen specific antibodies Western Blot • The use of antibodies in molecular biology is widespread • It is probably most often encountered in Western analysis • SDS-PAGE gel resolved into single protein bands (overlap possible) • Presence of a protein is determined by hybridizing the proteins, transferred or applied to a membrane, with the relevant antibody Protein Standard sample Antibody recognizes epitope in specific protein SDS-PAGE Membrane Western blot Western Blot • Used to detect specific proteins in a sample • Proteins separated by Sodium Dodecyl Sulfate-Polyacrylamide Gel Electrophoresis (SDSPAGE), transferred to a membrane • Primary (1st) antibody (monoclonal or polyclonal) used to detect protein • Enzyme linked 2nd antibody (e.g. horseradish peroxidase-linked) used to detect 1st antibody Enhanced chemiluminescence (ECL) Immobilized proteins Primary Fabantibody Fc •In the presence of H2O2, horseradish peroxidase (HRP) oxidizes diacylhydrazides such as luminol • Directly after oxidation, luminol is in an exited state, and emits a photon to return to the ground state • This photon can be detected with a film or a camera • Light emission can be enhanced by ~1000-fold with phenolic compounds such as 6-hydroxybenzothiazole (enhancer) Horseradish peroxidase H2O2 Epitope on protein surface Secondary antibody Membrane H2O luminol luminol h enhancer Detection ‘Brute-force’ or ‘High throughput’ cytokine detection (1.) Cytokine array Simultaneous detection of multiple cytokines (the process is similar to the procedures of Western-blot after the blotting step) multiple antigen specific antibodies bound to membrane labeled antibody mixture (+) IL-2 IL-4 unknown cytokine containing solution … … MIP3β IFN … ( -) Disadvantage – defined volume sample needed to cover the surface of the membrane cytokine production of moDC activated by CD40L and CD40L+SLAM combination Réthi és mtsi. 2006 Immunohistochemistry Labeled antibodies added to fixed tissue sections detect the distribution of the chosen antigen within the tissue or within the cells of a particular tissue • Immunofluorescence •Fluorescent dye coupled to antibody FITC – fluorescein isothiocyanate (green) PE – phycoerythrin (orange) • Immunoenzyme method • enzyme-coupled antibody P – peroxidase PA – alkaline phosphatase (Substrates converted into an insoluble compound) Immunohistochemistry Fixation Tissue sample Freezing Sectioning Section before staining Immunohistochemistry ABC Method Enzim X Avidin Biotin Secondary antibody Primary antibody Slide Cells Tissue sample Classical histochemistry Acute bronchopneumonia (hematoxilin- eozin staining) Only few cell types could be identified Immunohistochemistry (CD68+ macrophages and lymphocytes, granuloma) Antinuclear (ANA) autoantiboies from the serum of a SLE patient can be visualized in cell culture (Hep-2) by indirect fluorescent labeling (immunofluorescence) Immunohistochemistry using fluorescent detection (TRITC) Detection of actin microfilaments A fixed and permeabilized skin fibroblast. Mitochondria were labeled with mouse IgG (anti–OxPhos Complex V) and visualized using goat anti–mouse IgG conjugated with orange-fluorescent Alexa Fluor 555. F-actin was labeled with green-fluorescent Alexa Fluor 488 phalloidin (a mushroom toxin), and the nucleus was stained with TO-PRO-3 iodide Peroxisome labeling in fixed and permeabilized pulmonary artery endothelial cell. Peroxisomes were labeled using an antibody directed at peroxisomal membrane protein 70 and detected with Alexa Fluor 488–labeled goat anti–mouse IgG. Mitochondria were stained with MitoTracker Red prior to fixation; nuclei were stained with blue-fluorescent DAPI. Flow cytometry An immunofluorescent method that mutually complements the fluorescent microscopy • Investigation of different cells or particles travelling high velocity in flow • Detects fluorescence intensity and scattered light of the labeled cells • Can investigate enormous number of cells in short period of time Why flow cytometry Most cells in the immune system can be found in free or loosely adherent form. They can be easily suspensed and labeled by fluorescent antigen specific antibodies, and then they can be examined cell by cell. The cells’ light scatter and immunofluorescent properties can be analyzed statistically (eg. percentages of different cell populations) Rare cell populations can be identified and examined (eg. antigen specific lymphocytes) The method provide qualitative and quantitative data – it can detect the presence of different antigens in the cell, and the expression levels of these antigens. Changes in the expression of certain molecules can be followed after different treatment of the specimen. (eg. cell activation, disease progression) Benchtop flow cytometer Sorter - flow cytometer (FACS station) Example Chanel Layout for Laser-based Flow Cytometry The emited fluorescent light can be separeted to components by special mirrors and filters photodetectors PMT 4 cell suspension in tube flow cell PMT 3 PMT 2 PMT 1 forward light scatter detector Laser (PMT=photo-multiplayer tube) The scattered light and multiple fluorescent color can be measured. It can be considered as a fluorescent microscope with flow sample – but only with light intensity detection, no imaging Light scatter and fluorescence Forward angle light scatter sensor (FSC, FALS) Laser Can be loosely considered as a representation of the particle size Side light scatter(SSC) and fluorescence detectors SSC represents the granularity of the cells Multocolor staining can be used to identify cell sub-populations (autofluorescence – presence of piridins and flavins) Immunophenotyping Example: Measurement of CD4+ (helper) and CD8+ (cytotoxic) T cell ratio (eg. monitoring AIDS progression) Labeling: FITC labeled anti-CD4 antibody(α-CD4-FITC) PE labeled anti-CD8 antibody (α-CD8-PE) Th NK Tc Lymphocytes in the periferial blood Fluorescent microscopy B high velocity flow stream detecting CD4-FITC labeled (TH) cell (in cuvette or stream in air) detector signal processing unit CD8 PE screen increasing light intensity a dot representing a CD4+ CD8- cell CD4 FITC microscopy: detecting the PE labeled cell (CD8-PE) CD8 PE detector signal processing unit increasing light intensity CD4 FITC detecting the unlabeled cell (eg.B cell) by autofluorescence CD8 PE detector Signal processing unit increasing light intensity microscopy: dim (autofluorescent) cell CD4 FITC CD8 PE 18% 44% 0% quadrant statistics CD4 38% FITC Graphical representations 1. dot-plot contourplot densityplot Graphical representations 2. Histogramm Numeral intensity values: ~7 ~ 1300 homogenous cell population is normally distributed (Gaussian) Different cell types - characteristic light scattering granulocytes side light scattering (SSC) (e.g. granulated) monocytes lymphocytes forward light scattering (FSC) („size”) Examination of peripheral blood by haematology automats Measured parameters: peroxydase staining (the presence of myeloperoxydase, x – axis) light scatter (high on large granular cells, y – axis) 1 Noise 2 Nucleated Red Blood Cells 3 Platelet Clumps 4 Lymphocytes and Basophils 5 Large Unstained Cells 6 Monocytes 7 Neutrophils 8 Eosinophils Only the major cell types can be identified Characterisation of immune cells using cell surface markers Cell types, differentiation stages can be identified using a combination of cell surface markers. Used in diagnostics: - ratio of different cell types - altered expression of cell surface markers Examples: - Inflammatory processes – increased neutrophil numbers - HIV progression – decrease of CD4+ T cell count CD4+ : CD8+ = 1.6 Normal CD4+ T cell count = 600 – 1400/l AIDS = CD4+ T cell count <200/l - increase of CD5+ B cells – typical for some B cell Leukemias Diagnosis of immunodeficiency by flow cytometry WAS: Wiscott-Aldrich Syndrome A typical symptome: Lacking or decreased CD43 expression XLA: X-linked Agammaglobulinemia Inhibited B cell development: lack of CD19+ B cells CD antigen cell type function ligand CD3 T cells TCR signalling - CD4 helper T sejtek, (monocytes, T cell coreceptor, (HIV receptor) MHC- II, HIV pDC) CD5 T cells, (B cell subset: B1) adhesion, activation signals CD72 CD8 cytotoxic T cells, (NK, T cells) T cell coreceptor MHC I CD14 monocytes, macrophages, some granulocytes LPS binding LPS, LBP CD19 B cells part of CR2, B cell coreceptor C3d, C3b CD28 T cells costimulatory signals to T cells (B7-1, B7-2) CD80, CD86 CD34 hematopoietic progenitor cell adhesion CD62L (L-selektin) CD56 NK cell, (T and B cell subset) homoadhesion (N-CAM isoform) APC: DC, B, monocyte, macrophage costimulatory signals CD80, CD86 (B7-1, -2) CD28, CD152 ‘Brute-force’ or ‘High throughput’ cytokine detection (2.) Cytometric multiplex bead array (CBA) Flow cytometric method with principles similar to cytokine array. Cytokines are determined not by their positions on the membrane but the fluorescent color intensities of the cytokine capture beads. IL-2 cytokine array CBA IL-4 IL-8 … … IL-12 IL-23 IL-17 … … Cytometric Bead Array The presence and the quantity of the cytokine can be shown by a light intensity of the reporter antibody labeled with different fluorescent color reporter antibody citokine citokine capture bead Cytokine standards for evaluating the concentrations IL-2 IL-4 … … Works with small volumes (5-20l), but requires special instruments Cytometric bead array (CBA) The principle of CBA is comparable with the sandwich ELISA Sandwich ELISA CBA IL-2 IL-4 IL-2 IFN Cytokine quantity TNFα IL-6 IL-8 IL-12 IL-10 IL-1β 500pg/ml 250pg/ml 125pg/ml 62pg/ml 31pg/ml 16pg/ml Cytokine standard dilution series 8pg/ml 0 Acquired Immune Deficiency Syndrome – AIDS Certain infectious microorganisms can supress or subvert the immune system. At the beginning of the last century, when tuberculosis was the leading cause of death and fully half the population was tuberculin-positive, it was well-known that an intercurrent measles infection would cause a well-contained tuberculosis infection to run rampant and result in death. The mechanism responsible is now known to be the supression of IL-2 synthesis after binding of measles virus to CD46 or CD150 (SLAM) on macrophages. Some of the microorganisms that supress immunity act by infecting lymphocytes. The human immunodeficiency virus (HIV) presents a chilling example of the consequences of infection and destruction of immune cells by a microorganism. The T-cell surface CD4 molecule acts as a receptor for HIV. CD4 is also expressed on the surface of cells of the macrophage lineage and they too can be infected by this virus. The clinical latency is long, usually it means several years. During this period, the level of CD4+ cells and virus particles in the blood changes. When the rate at which CD4+ cells are being destroyed exceeds the capacity of the host to replenish them, their number decreases to a point where cell-mediated immunity falters. The failure of cell-mediated immunity renders to the host susceptible to fatal opportunistic infections. Case study: The Pinkerton-family: infected blood caused tragedy Benjamin Pinkerton was a US-navy lieutenant who saw service at Japan. He married with a japanese woman during his service, who gave birth two healthy girls in 1987. She bore a boy four years later, who seemed healthy, as well. The boy got the routine DPT-vaccination and an oral polio-virus immunization. These vaccinations had no side-effect and the boy grew normally. At the age of six months he got sick and started to lose weight. He had severe, chronic diarrhea with fever. Besides a chronic oral candidiasis, the boy got two otitis, one after the other . The navy doctors examined the baby several times and prescribed antibiotic but it proved ineffectual. Results of somatic examination: - body-temperature 38oC; - candidiasis on the lateral sides of tongue and on the mucosal surface of the oral cavity; - „diaper-pimples”, which is also caused by Candida infection; - at respiration a subtle, slurping noise was heard in each pulmonary lobes; Oral candidiasis esophageal candidiasis Diaper pimples Laboratory: - normal amount of leukocytes (6500/l); - normal rate of leukocytes (neutrophyl 62%; lymphocyte 30%; monocyte 5%; eosinophyl 2%; basophyl 1%); - normal serum immunoglobulin levels: - serum IgG: 997 mg/dl (phys.: 800-1000 mg/dl); - serum IgM: 73 mg/dl (phys.: 50-150 mg/dl); - IgA: 187 mg/dl (phys.: 150-300 mg/dl); - normal amount of CD8 + T-cells, but the rate of CD4+ T-cells is very low, only 85/l (phys.: 1000-1200/l); - intradermal Candida-antigen did not evoke late-type hypersensitvity reaction; - results of ELISA and Western-blot analysis: HIV-antibodies in the serum; METHOD ELISA Western blot EXAMINED PROTEINS SAMPLE DETECTION Anti-HIV IgG and IgM antibodies serum (sometimes saliva or urine) with secondary (conjugate-) anti-IgG antibodies HIV capsid-proteins: p17, p24 , p6, p7 Envelop: gp41, gp120, gp160; serum with secondary (conjugate-) anti-IgG antibodies During HIV-diagnostics samples are always analyzed firstly by ELISA-method. In case of reactivity (serum positive) two more measurements are needed (2nd and 3rd analysis). If the 2nd and 3rd measurements show reactivity as well, the subject’s sample must be verificated: usually a Western blot or another ELISA is performed. After this finding they verified the parents: Both of them were HIV-positive. HIV supplemental confirmatory tests: Western-blot: The solid phase antigens are derived from LAV strain of HIV-1 grown in the CEM cell line. You can obtain pre-wet blot membrane strips and incubate with the examined serum. HIV specific serum antibodies result specific bands on the Western blot. At least two envelop protein specific band or one envelop specific and the p24 antigen specific band can be considered as positive test. Immunofluorescent assay (IFA): The assay uses immortalized human T-cells which express HIV-1 antigens on their surface. The cells are fixed to the surface of an IFA glass slide. Fixed, uninfected T-cells are provided as a control. The serum or plasma sample HIV- I antibodies comes in contact with the HIV-1 antigens on the slide. Fluorescent secondary antibodies detects them. The interpretation of the degree and pattern of fluorescence of the infected cells of the IFA slide compared to the uninfected cells determines the confirmed HIV-1 status of the sample. While Pinkerton was healthy, his wife was feeling unwell and complained about the swelling of her cervical lymphatic nodes. It turned out, that she was pregnant right before the boy’s birth. At the end of pregnancy the fetus had died and had to be removed by caesarean section. The operation was going well but – because of the loss of blood – she needed blood-transfusion (she got two units of blood). The boy got two severe infections in turn: Pneumocystis carinii- and Pseudomonas aeruginosa. He had serious cough with bloody spit (hemoptysis). A week after this he died. The parents got AZT- (zidovudin) therapy. While his wife died soon in respiratory failure, the lieutenant – in spite of his high serum HIV-antibody level – has not had symptoms yet. Special cytometers New fast computers and high speed imaging opened the possibility to record the investigated cells’ images during flow cytometry. Morphological data can be obtained by flow cytometry Good tool to investigate some cellular function (See on the coming pictures or the next seminars) Imaging cytometry, LSC (detailed morphology) www.amnis.com