Survey final report - International Federation of Red Cross and Red
advertisement

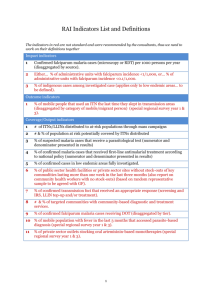
Survey of malaria indicators in Caprivi Regional Red Cross Society area, Namibia, using cell phone data entry — Preliminary report, 7 February 2012 RAMP (Rapid Mobile Phone-based) Survey Naemi Heita (1), Laimi Onesmus (1), Hilma Kambundu (1), Polly Helmut (2), David Simataa (2), Michael Charles (3), Bong Duke (4), Jenny Cervinskas (5), Jason Peat (5), Mac Otten (6) 1. Namibia Red Cross Society, Windhoek Namibia 2. Namibia Red Cross Society, Caprivi Region, Namibia 3. International Federation of the Red Cross, Johannesburg, South Africa 4. Consultant, International Federation of the Red Cross, Canada 5. Consultant, International Federation of the Red Cross, Nigeria 6. International Federation of the Red Cross, Geneva, Switzerland 7. Consultant, International Federation of the Red Cross, Atlanta, USA Executive Summary Background. The Namibia Red Cross sponsored a baseline survey for the second phase of a multi-year project among a population of 46,727 that lived in the Caprivi Region during 30 January to 3 February 2012 to examine important malaria indicators using several innovative data collection methods. Methods: The survey used probability-proportional-to-estimated-size (PPES) sampling of primary sampling units (PSUs) and PPES to select one segment from unequal-sized segments. Households were chosen from the segment using simple random sampling. The sample included 30 PSUs, 10 households per PSU, and 1283 persons. Cell phones were used by Namibia Red Cross volunteers to conduct the household interviews and enter survey data using EpiSurveyor software in real-time. Results: The gap in the number of LLINs needed to achieve universal coverage was 11,816 (48% of sleeping spaces). Since an estimated 4,824 ITNs were 36 month old and need to be replaced, the total ITNs needed to be distributed in 2012 is 16,640. An estimated 44% (95% confidence interval [CI] 36-51%) of persons of all ages slept under an ITN during the night before the survey and 94% of nets were used the previous night. Of children <5 years old with fever in the two weeks before the survey, 29% received an ACT and 22% received an ACT within 24 hours. Seventy-two percent of households received IRS in the previous year. Conclusion: The number of ITNs available to households needs to be doubled to achieve universal coverage (all persons sleeping under an ITN). Approximately onequarter of households still need to be reached with IRS. The innovative survey methodologies provided valuable health and malaria data rapidly. 2 Background The government of the Republic of Namibia (GRN) and partners are striving to reduce the number of cases and deaths from malaria by 50% by 2010 and by 75% by 2015 in line with Millennium Development Goals, World Health Assembly, Roll Back Malaria partners, and GRN goals. The Ministry of Health and Social Services (MOHSS) in Namibia is now stressing the importance of universal coverage of persons of all ages (100% of persons using an insecticide-treated bed net in endemic areas) as advocated by the World Health Organization (WHO) to achieve the disease-reduction goals. The two most important indicators of universal coverage with ITNs are: 1) the percentage of persons that had access to ITNs in the household (assuming that 1 ITN covers two persons), and 2) the percentage of all persons using ITNs the previous night. For treatment, all persons with malaria are supposed to receive an appropriate treatment within 24 hours, especially children <5 years old, the highest risk group for malariarelated mortality. In late 2009, WHO advocated parasite-based testing of all suspected malaria cases (including the use of rapid diagnostic tests—RDTs), even in high-burden African countries. Malaria continues to be a major public health problem in Namibia. The disease was the leading cause of illness and death from 1999 to 2002 and still remains one of the top five diseases of public health concern in the country. Malaria is endemic in Caprivi, Kavango, Kunene, Ohangwena, Omusati, Oshana, Oshikoto, and part of Otjozondjupa and Omaheke regions, where 65 percent of the Namibian population live and are at risk 3 of malariaa. The prevalence of malaria is highest between September to December. Preliminary MOHSS data shows that malaria cases reported from health facilities in the Caprivi Region declined from approximately 4000 cases in 2006 to 300 cases in 2010. This survey was carried out in Caprivi regionb, in the northeast of Namibia. Divided into the Kongola, Linyanti, Sibanda, Katima Mulilo Urban and Rural, and Kabbe constituenciesc, the region covers a total area of 14.528 km and accounts for 1.8% of the total land area of Namibia. It shares borders with four countries, being Angola and Zambia in the north, Botswana in the south, and Zimbabwe to the east. The administrative centre of the region is Katima Mulilo, the only town in the region. Six settlement areas serve as local administrative centers. These are Bukoalo, Chinchimani, Linyanti, Mafuta, Ngoma, and Omega III. Eastern Caprivi is subject to seasonal flooding and the Kabbe constituency comprises the eastern flood plains of the region, and is subject to seasonal flooding. There is an annual flood season with numerous flood-prone villages. In 2011, the flooding was widespread, and more than 1000 people had been “relocated permanently” from 32 flood-prone villages as the region prepared to meet a Zambezi river swollen to record-size for this time of the year as a result of torrential rains upstream (ref: www.irinnews.org/report.aspx?reportID=91770, accessed March 3, 2011). In 2011, more than 20 settlement camps were established on higher ground, with entire villages being relocated to these camps. A number of a Namibia Demographic and Health Survey 2006/2007 b Namibia is divided into 13 regions, and each one is further subdivided into electoral constituencies. The latest Namibian Census of Population and Housing for which the results were published was carried out in 2001. A national census was carried out in August 2011 and the results are expected to be released soon. c A constituency refers to a group or area from which voters in an election are drawn. The number and size of each constituency varies with the size and population of each region. There are a total of 102 constituencies in the country, and overall, the country is divided into 4002 enumeration areas (EAs) (Population Census 2001). 4 organizations, including the MOHSS and the Namibia Red Cross, provided services in the camps. In 2001, Caprivi Region had a population of 79,826 people (with a household population of 78,785 and 16,839 households), representing 4.4% of Namibia’s total (Population Census 2001). Twenty-eight percent of the population is urban and 72% rural. The average household size in Caprivi region is 4.7 persons compared to 5.1 persons nationally, and well below the average rural household size of 5.7. Femaleheaded households account for 49% of households, and 46% of households have orphans or children under the age of 18. The average number of children per women is 3.8 and 13% of the population is under five years. More than 95% of the populations speak one of several dialects of what is commonly lumped together as Caprivian. The main dialects are Sifwe, Subiya, Totela, and Yeyi. The 2006-07 Namibia Demographic and Health Survey showed that Caprivi was one of four regions in Namibiad that have the highest proportion of the population in the lowest wealth quintile of the wealth index and only a small proportion in the highest quintile. Insecticide-treated bed nets (ITNs) are distributed in Caprivi through the MOHSS routine health services. A pregnant woman is eligible to receive one free bed net during antenatal care services, and children under age five years that attend a health facility are also eligible to receive a free LLIN. Over the past few years the MOHSS and the Namibia Red Cross have distributed LLINs in the settlement camps established for those affected by the flooding of the Zambezi and the Chobe Rivers through mass distribution to targeted vulnerable groups (pregnant women, children under age five years, and elderly women aged 60 years and over). There has only been one regionwide mass campaign in Caprivi, with LLINs distributed in 2008 as part of the Zambezi d The other three are Kavango, Ohangwena and Omusati. 5 River Basin Initiative. Since 2009, the Namibia Red Cross (NRC) has been distributing LLINs in the camps. In addition to the MOHSS and the NRC, the NGO SMA (Social Marketing Associates) has been distributing LLINs in villages in some constituencies. SFH (Society for Family Health) sells LLINs through their social marketing program, and also distributes LLINs to the elderly when they receive their monthly government pension benefit. This malaria indicator survey will serve as a baseline for the next phase of the Namibia Red Cross project Communities Fighting Malaria that aims to improve the health and well-being and improve malaria control for persons in four of the constituencies in Caprivi Region where the Namibia Red Cross works--Kabbe, Katima Mulilo Rural, Kongola and Linyanti. In this project, the NRC, in collaboration with the village heads, will recruit 51 community volunteers who will serve as the project’s supervisors in the villages. Each supervisor will have the responsibility of supervising an average of about 10 community-based volunteers. A total of more than 500 volunteers will be trained by mid-2012 by these supervisors. In turn, each community-based RC volunteer is responsible for about 100 households. In addition to serving as the baseline for the next phase of the CFM project, this survey is the endline for the first phase of the project. A previous survey was carried out by the NRC and IFRC in May 2011. That survey was also carried out using the RAMP survey methodology. It is expected that the final evaluation will be done in November 2012. The sampling frame for the May 2011 RAMP malaria survey was not identical to the 2012 RAMP malaria survey because in the May 2011 survey, the Caprivi Region was devastated by floods, with over 90% of the Kabbe constituency flooded. More than 6 9,000 people were affected by the floods, and a total of 20 temporary camps and two permanent resettlements camps (Choi in Linyanti and Izwe in Kongola) had been established (Namibia Red Cross, personal communications). Of the 30 clusters selected, 12 of them were in the settlement camps. While the RAMP survey does not collect data on all the key indicators of the Communities Fighting Malaria project, it does collect data on many of the core indicators related to bed net ownership and usage, and to the treatment of fever in under-five year olds and the diagnosis of malaria. These include indicators that are aligned to the MOHSS Malaria Strategic Plan (2010-2016) and the MOHSS National Monitoring and Evaluation Plan (2010-2016). In addition, the survey collects data on indicators that measure universal coverage, a goal that the GRN is moving toward. The results of this survey can be used to adjust the MFC project and the malaria prevention and control program, if necessary, and to advocate for needed changes to support the provision of LLINs, and the provision of services for treating fever in children under age five years, to communities within the sample constituencies. Other investigations will be done by the NRC in 2012 to explore in more depth aspects of the CFM project that are related to behavior change and communications. The International Federation of the Red Cross (IFRC), with the support of DataDyne, WHO, and epidemiologists have been working for several years on a “management survey” concept that uses cell phones for data entry for surveys, primarily on the survey methodology and operations. In 2011, the management survey concept was successfully field tested in three African countries: Kenya in January, Namibia in May, and Nigeria in June. This concept includes use of cell phones and freely-available software to conduct health surveys rapidly, simply, at low cost, with minimal external 7 technical assistance. The survey sampling method avoids the main potential bias of the Expanded Programme on Immunization (EPI) cluster survey method (initial selection of the first household using a random direction from the center of the PSU). This survey approach is now called the RAMP (Rapid Mobile Phone-based) survey. IFRC will soon publish a technical reference manual and a training manual that will be readily accessible for those interested in carrying out a RAMP survey. This RAMP survey in Caprivi had the following innovations: 1) 30 clusters (like the EPI cluster survey)1, 2) total of 300 households in the sample (10 households per cluster), 3) use of the Episurveyor web-based tool to collaboratively design model malaria questionnaires (including responses and skip patterns) that can be easily adapted to local surveys and translated into local languages, 4) use of cell phones to enter data during the interview, 5) daily upload of data to an internet-based database, 6) daily data cleaning of uploaded data, 7) daily review and feedback of data quality issues to interviewers and team supervisors 8) daily analysis of uploaded data, and 9) completion of preliminary results bulletin within 24 hours of the last interview. 8 Methods The survey was conducted during 30 January to 3 February 2012 in the four constituencies in Caprivi Region where the Namibia Red Cross works--Kabbe, Katima Mulilo Rural, Kongola and Linyanti. The sampling frame was a list of communal lands, settlements, and mixed areas, from the 2008 sampling frame provided by the Namibian Bureau of Statistics, based on the latest census data (2001 national census) released by the GRN. The 2008 census estimation of population in the area was 46,727. Thirty primary sampling units (PSUs) were selected using probability proportional to estimated size. Using maps of each PSU that were obtained from the Namibia Central Bureau of Statistics, the selected PSUs in the settlements and communal lands were mapped and divided into 2-10 segments using natural boundaries. Once a segment was selected by PPES, all households were listed or mapped and 10 households were chosen by simple random sampling. Additional households were chosen in case members of selected households could not be reached. Data was collected on all persons sleeping in the household (“sharing a common cooking pot”) the previous night. The design resulted in an equal probability survey. Three questionnaires were developed online using the Episurveyor web-based questionnaire design tool (www.episurveyor.org)—household, person roster, and bed net roster. Questions were modeled after the Roll Back Malaria (RBM) Malaria Indicator Survey (2005).2 Principal component analysis was used to create the wealth quintiles index for each household. Analysis was performed in STATA version 11 (College Station, Texas, USA), taking into account the design of the survey. “Access” to an ITN was defined as the population that could have been covered by ITNs present in the households at the time of the survey. The ratio of persons that could have been 9 covered per ITN was calculated from the net roster data (1.88 persons/ITN). The crude estimate of access was the total number of ITNs in the households times 1.88 persons/ITN divided by total population. The ratio of persons to ITN (1.88) for this calculation was similar to the ratio of 2.0 used by WHO in its World Malaria Report 2010 to calculate access to ITNs.3 We estimated the number of ITNs needed for universal access, the number of ITNs currently in the whole survey domain, and the gap to be filled. The number of ITNs needed for universal access was calculated by dividing the sampling frame population by the average number of persons sleeping under ITNs during the survey (1.88). The number of ITNs currently present was estimated by multiplying the number of ITNs found in households by the survey weight (36.42). The total number of LLINs that need to be distributed in 2012 to achieve universal coverage needs to include nets that need to be replaced due to age (36 months or old nets). There are two new MERG indicators of access—by household and for populations. The indicator by households is the persons of households with sufficient nets to cover all inhabitants based on a ratio of 2 persons for one ITN. The indicators for populations is the number of persons with access to an ITN assuming that 2 persons can use each ITN. The indicator about protection of households by ITNs or IRS assumed that any ITN (even just one) in the household protected all inhabitants. In households with many people, a single ITN may provide only partial protection from malaria. Therefore, this indicator may over-estimate protection. 10 There was significant "heaping" of responses of the age of nets in months at 12 and 36 months. We counted "12" to be in the 12-23 month category and "36" to be in the 3647 month category. The questionnaires (see annex for a copy, exported from the EpiSurveyor form to Word format) on the mobile phones were in English, and the majority of the interviews were carried out in Silosi, the local language in Caprivi. Survey operations. The survey operations were led by the Namibia Red Cross. Training was provided for the 12 interviewers and six team supervisors during four days (23-27 January 2012). Survey field work took 5 days (30 January to 3 February 2012). Nokia-brand cell phones--Nokia 2730 ($80 USD, no keyboard, no GPS) and Nokia C-02 ($105 USD, no keyboard, no GPS) --were used to run DataDyne’s freelyavailable cell-phone-based EpiSurveyor software (http://www.datadyne.org/ and http://www.episurveyor.org/). Survey data were immediately entered into the cellphone database during the interview for the household questionnaire. Immediately before administering the person roster and the net roster questionnaires, a paper line list of persons that slept in the household the previous night was created by asking about each person who slept in the household the previous night so that the person line number/identifier was available during questions in the person roster, and for questions in the net roster about who slept under each net. Uploading of data on the cell-phone to the internet-based database using EpiSurveyor software required a 2G/GPRS cellnetwork connection. The field supervisors uploaded data at the end of the day upon their return to Katima Mulilo. Interviewers (and cell-phone data entry persons) were the Namibian Red Cross volunteers who serve as supervisors in the four constituencies included in the Communities Fighting Malaria project: Kabbe, Katima Rural, Kongola and Linyanti. The team supervisors were Namibian Red Cross supervisors that were involved in the Communities Fighting Malaria and other NRC projects. 11 Since the data were sent from the mobile phones each evening to an internet database, the local consultant and out-of-country consultants were able to perform data cleaning each evening. A Namibian analyst could not be located, so an out-of-country consultant analyzed the data each night. A survey-results bulletin was produced within 24 hours of the last interview using an Excel-based, 4-page “survey results bulletin” tool. The preliminary survey results (pages on four Excel worksheets were combined into a single PDF) were distributed to interviewers at an end-of-survey debriefing meeting within 15 hours of the last interview on 4 February 2012. A preliminary report was distributed to stakeholders within 72 hours on 6 February 2012. Report tables and graphs. The tables and graphs of the survey-results bulletin act as the tables and graphs for this preliminary reporte. Results Table 1 on the survey-results bulletin shows key descriptive information about the survey. The number of persons in the sample frame was 46,727. Data were collected on 1283 persons of all ages and 175 children <5 years old in 300 households. Ninetysix percent of the nets were permitted by the residents to be observed. Ninety-four percent of the ITNs were reported hung the night prior to the survey. There were enough nets to cover 48% of the sleeping places and enough hanging nets to cover 46% of the sleeping places. The main ITN indicators are shown in the figure on page one of the survey-results bulletin. The percentage of households with at least one ITN e The survey-results bulletin is a companion document to the survey report, and contains information, tables and graphs that show the survey findings. 12 was 62% (95% confidence interval [CI], 55-69%). The percentage of households with sufficient ITNs for all household members was 33% and percentage of the population with access to an ITN was 50%. The average number of persons sleeping under an ITN was 1.88. The percentage of persons that slept under an ITN last night was 44% (CI 36-51%) for all persons and was 55% (CI 48-62%) for children <5 years old. In households that owned at least one ITN, the percentage of children <5 years old that slept under an ITN increased to 79%. Seventy-two percent of households received indoor residual spraying with insecticide in the last 12 months. The percentage of children with fever in the previous two weeks that had a finger or heel stick for blood was 25%. The percentage of children with fever that received treatment with an ACT was 29% and the percentage that received an ACT within 24 hours of onset of fever was 22%. The estimated number of ITNs needed to provide access to all persons (based on 1.88 persons per ITN) in the entire sampling frame was 24,855. The number of nets currently in all households in the survey frame (those sampled and not sampled) was 13,038, 48% (n=24,855) of that needed to achieve universal access. The number of ITNs needed to fill the gap was 11,816. The percentage of nets that were 36 months and older was 37%. Therefore, an additional 4,824 ITNs need to be replaced immediately, bringing the total ITNs needed in 2012 to 16,640 (11,816 + 4,824). Table 2 shows key ITN indicator point estimates, confidence intervals, and data by wealth quintile. The ownership of ITNs was nearly the same across wealth quintiles. Table 3 shows the age of ITNs—15% of the ITNs were <12 months old, 26% were 3 years old, and 37% were ≥36 months old. Table 4 shows that recent home visits and visits to clinics where malaria was discussed were infrequent (17%). Table 5 shows additional ITN and IRS information. The greatest source of information about nets was from health center staff (44%) and radio (36%). Table 6 shows additional 13 information about treatment, including the rare use of chloroquine, quinine, and sulfadoxine-pyramethamine for treatment. The percentage of children <5 years old with fever in the previous two weeks was 49%. Twenty-five percent of children with fever reported to have received a malaria blood test, and, of those, 70% (19 of 27) were reported to be positive. Twenty-nine percent of children <5 years old with fever received an ACT. Table 7 shows the width of the 95% confidence interval and the design effect for 3 key variables. The confidence interval was ±8% for the percentage of persons using an ITN, ±7% for household ownership of at least one ITN, and ±7% for children using an ITN. The design effect was <2.0 for two key indicators and was 6.3 for ITN use in all ages. The graph on page 4 shows the age distribution of ITN use. Those 10-24 years old had lower use than other age groups. The supplemental analyses on page 4 showed that 97% of nets were LLINs and 20% of nets had 3 or 4 persons sleeping under them. Two-thirds of household heads were able to identify “mosquito bites” as the cause of malaria. Sixty-nine percent were able to identify mosquito nets as the main method to prevent malaria. Discussion This malaria survey showed similar ITN coverage as the survey 8 months previous— the number of ITNs in households needs to be doubled to achieve universal coverage— 16,640 LLINs need to be distributed in 2012 to fill the gap. Approximately half (44%) of the persons were sleeping under an ITN the previous night. A high percentage of ITNs were used the night before the survey (94%) so that there is only a small gap in ITN use given ownership. Therefore, the primary ITN gap is ownership and access, not ITN use. The age of ITNs may also be a significant issue since 37% of the ITNs 14 were reported to be 3 years old or older. Most of the nets (56%) were reportedly obtained from the health center and 24% from a mass distribution. About half of the nets from a mass distribution were received when LLINs were distributed in 2011 (either by the RGN or by NRC or NGOs) to populations that had been relocated due to flooding and were living in settlement camps. The percentage of children <5 years old with fever in the previous two weeks was high (49%) compared to 30% found in most other African countries (however, the percentage was also higher than average in Malindi, Kenya in January 2011 [40%] in the first pilot survey, and in the Namibia 2009 MIS survey the highest percent of under-fives with fever in the past two weeks was found to be in the Caprivi region, at 36%). The percent of children with fever may have been higher in the survey because, in this area, the local term for fever, “mena”, can also mean a runny nose without fever. Seventy-two percent of households had received IRS within the previous 12 months. The recommended coverage for IRS is >80% to have reasonable impact. A recent survey of IRS coverage found that 85% of the population had been protected by IRS in the latest round of MOHSS spraying in the Caprivi Region (MOHSS, personal communications). IRS is a primary malaria control tool in most low-incidence countries in southern Africa. The survey findings for some of the ITN indicators were similar to those in the 2008 DHS in Caprivi Region where it was reported that 55% of households owned an ITN, and the average number of ITNs per household was 1.0. While the 2008 DHS survey reported that 41% of children <5 years old slept under an ITN the night before the survey, the 2009 MIS survey reported this to be 35%, and the 2012 RAMP survey reported a value of 54% (up from the RAMP May 2011 finding of 42%). This figure rises to 79% when reporting ITN use in children under five years of age in households that own t least one ITN. 15 The survey findings for some of the ITN indicators were also similar to those in the 2009 Malaria Indicator Survey for the Caprivi Region. Fifty-seven percent of households owned at least one ITN, and the average number of ITNs per household was 1.0. However, the RAMP survey findings report that 55% of children <5 years old slept under an ITN the night before the survey, compared to a finding of 35% in the MIS survey. The 2009 MIS reported that 22% of all people slept under an ITN, while the 2011 RAMP survey reported this to be 38%, and the 2012 RAMP survey, 44%. This survey provided an excellent estimate of the number of LLINs that the project needs to obtain to achieve universal access: 16,640 (gap plus replacement of older nets). An advantage of this survey is that it provides a reasonably accurate estimate of the total number of existing ITNs, the gap that needs to be filled, and the number of ITNs that are ≥36 months old that also need immediate replacement. The confidence interval of ≤10% for 3 key indicators shows that the sample size and number of clusters were sufficient for most management decisions. The EPI cluster survey target precision is ±10%. Daily uploading of data to an internet database allowed an external analyst to complete most of the analytic tasks within 24 hours and send the results to local survey leaders to discuss with surveyors and stakeholders. 16 Conducting a health survey with precision of ±10% at low cost with rapid results is likely to be attractive to non-governmental organizations (NGOs) and ministries of health (MOHs). This survey and analysis had several limitations. First, the education and experience level of interviewers was substantially less than those of other more-expensive surveys such as national malaria indicator surveys and Demographic and Health Surveys. Second, the sample size of 300 households was too limited to provide estimates on pregnant women (3.5% of the population) and would be too small to allow high precision for extensively disaggregated analyses (for example, ITN use in children by wealth quintile for just females). However, the rapid mobile survey (RAMP) tools and methods are not limited to a single survey domain of 30 clusters and 300 households. NGOs and MOHs can use any sample size and number of clusters that they feel is appropriate. In conclusion, this survey successfully met its objective of rapidly measuring baseline malaria intervention coverage prior to the start of a new project cycle at low cost. 17 References World Health Organization. The EPI coverage survey. www.who.int/immunization_monitoring/routine/EPI_coverage_survey.pdf. Accessed 30 January 2011. Roll Back Malaria. Malaria Indicator Survey: Basic Documentation for Survey Design and Implementation. http://www.rbm.who.int/partnership/wg/wg_monitoring/docs/mis2005/cc1.pdf. Accessed 30 January 2011. World Health Organization. World Malaria Report 2010. Geneva, Switzerland. 2006-07 Namibian DHS. Ministry of Health and Social Services. Republic of Namibia. Malaria Strategic Plan (2010-2016). November 2010. Windhoek, Namibia: Ministry of Health and Social Services Ministry of Health and Social Services. Republic of Namibia. National Malaria Monitoring and Evaluation Plan (2010-2016). December 2010. Windhoek, Namibia: Ministry of Health and Social Services Ministry of Health and Social Services. Republic of Namibia. National Malaria Policy. Windhoek, Namibia: Ministry of Health and Social Services. National Planning Commission (NPC), Central Bureau of Statistics, 2002. 2001 Population and Housing Census. Windhoek, Namibia: National Planning Commission. 18 Acknowledgements The assistance provided by the Namibia Central Bureau of Statistics for the survey sampling was invaluable. A special thanks goes to Mr. Weerasinghe, CBS, Windhoek and Ms. Benitha Kwala, GIS analyst, CBS Caprivi branch for their collaboration and assistance. The support of the MOHSS in this survey was also greatly appreciated. In Windhoek, the MOHSS took part in reviewing the survey questionnaires, while in Katimi Mulilo, the survey benefited from the information and collaboration provided by Mr. Albius Maswahu, Caprivi Region Health Director. Mr. Jamela Dube and Ms. Agnes Mwilima served as resource persons during the training of the enumerators and team supervisors, and we are grateful for their excellent presentations and support provided. The insights provided by Dr. Dube when the preliminary survey results were presented to the survey field teams was also of great value. 19 Annex 1. Questionnaires Survey Name : 1_HHold_Nam_01_2012 No of Questions:39 ======================================================================= 1:NAMIBIA RAMP SURVEY HOUSEHOLD QUESTIONNAIRE (label) 2:Consent Obtained? (multi) Data Field Name : consent Possible responses: - Yes - No 3:CLUSTER and HOUSEHOLD NUMBER questions follow next (label) 4:Cluster number (number) Data Field Name : hh_clusternumber 5:Household number (number)Data Field Name : hh_hhnumber 6:Name of head of household (text) Data Field Name : hh_hhname 7:Household in a rural or urban area? (Urban defined as a town with >=5000 persons) (multi) Data Field Name : rural_urban Possible responses: - Rural - Urban 8:How many kilometers is your household from the nearest health facility or hospital? (98=do not know). If less than 1 km, put "1". (number) Data Field Name : num_km_to_facility 9:How many minutes does it take to walk to the nearest health facility? (98=do not know). If less than 1 min, put "1". (number) Data Field Name : min_to_health_facility 10:BEDNET questions follow next (label) 11:Number of people of all ages who slept in this household last night? (do NOT include usual members of this household who slept somewhere else last night) (number) 20 Data Field Name : totalpersons 12:Last night, how many sleeping spaces were there (both inside and outside if someone slept outside)? (Sleeping space defined as a place where people sleep that could be covered by a single net). (number) Data Field Name : numhhsleepingspaces 13:Has anyone visited this household in the last 6 months to talk about malaria or bednets? (multi) Data Field Name : visithomemalaria Possible responses: - Yes - No - Do not know 14:Has anyone in this household visited a health facility where they discussed malaria or bednets in the last 6 months? (multi) Data Field Name : visitclinicmalaria Possible responses: - Yes - No - Do not know 15:In your opinion, what is the main cause of malaria? (multi) Data Field Name : cause_of_malaria Possible responses: - Mosquito bites - Eating immature sugarcane - Eating watermelon - Eating other dirt food - Drinking dirty water - Getting soaked with rain - Cold or changing weather - Witchcraft - Others - Do not Know 16:In your household, what is the main method used to protect against getting malaria? (multi) 21 Data Field Name : protection_against_malaria Possible responses: - Sleep under a mosquito net - Sleep under an insecticide-treated mosquito net - Use mosquito repellent - Take preventive medication - Spray houe with insecicide - Keep house surroundings clean - Other - Do not know 17:What is your main source of information about the use of bednets? (multi) Data Field Name : itn_netinfosource Possible responses: - Radio - Health facility - Community-based volunteer - Community leader - Neighbor - Relative - Television - Other - No information 18:Indoor Residual Spraying (IRS) question follow next (label) 19:At any time in the past 12 months, has anyone sprayed the interior walls of your dwelling against mosquitoes? (multi) Data Field Name : irsyn Possible responses: - Yes - No - Do not know 20:HOUSEHOLD ASSET questions follow next (label) 22 21:Does your household have electricity? (multi) Data Field Name : wlth1 Possible responses: - Yes - No 22:Radio? (multi) Data Field Name : wlth2 Possible responses: - Yes - No 23:Television? (multi) Data Field Name : wlth3 Possible responses: - Yes - No 24:Refrigerator? (multi) Data Field Name : wlth4 Possible responses: - Yes - No 25:Electric iron? (multi) Data Field Name : wlth5 Possible responses: - Yes - No 26:Electric fan? (multi) Data Field Name : wlth6 Possible responses: - Yes - No 23 27:Bicycle? (multi) Data Field Name : wlth7 Possible responses: - Yes - No 28:Motorcycle or scooter? (multi) Data Field Name : wlth8 Possible responses: - Yes - No 29:Car or truck? (multi) Data Field Name : wlth9 Possible responses: - Yes No 30:Cow, goat, or sheep? (multi) Data Field Name : wlth10 Possible responses: - Yes - No 31:Canoe or boat? (multi) Data Field Name : wlth11 Possible responses: - Yes - No 32:Phone? (multi) Data Field Name : wlth12 Possible responses: 24 - Yes- No 33:Domestic worker (unrelated to head of household)? (multi) Data Field Name : wlth_domesticworker Possible responses: - Yes - No 34:Do members of this household work on agricultural land OWNED BY themselves or their family? (multi) Data Field Name : wlth_hhagland Possible responses: - Yes - No 35:What is the principal household source of drinking water? (multi) Data Field Name : wlth_hhwater Possible responses: - Tap water into residence - Protected well in residence - Unprotected well in residence - Open well in yard - Protected well in yard - Unprotected public well - Protected public well - Tap in yard - Tanker truck - Bottled water - Public tap - Rain water - Surface water (eg. River Lake Stream) - Spring 36:What is the principal type of toilet/sanitary facility used by members of your household? (multi) 25 Data Field Name : wlth_hhtoilet Possible responses: - Own flush toilet - Shared flush toilet - Own pit latrine - Own improved pit latrine - Shared pit latrine - Shared improved pit latrine - Bush or field - Other 37:What is the principal type of flooring in your house (interviewer may choose to observe)? (multi) Data Field Name : wlth_hhfloor Possible responses: - Dirt or sand - Dung/wood/palm/bamboo - Cement including vinyl - Cement including parquet - Tile (e.g. ceramic/mable) - Carpeted - Other 38:What is the principal type of cooking fuel in your house? (multi) Data Field Name : wlth_hhcook Possible responses: - Wood or dung - Kerosene - Charcoal - Electricity - Gas - Solar Energy 26 39: This portion of the interview is complete. Close this questionnaire by clicking ``Finish for now`` on next screen. If consent was NOT obtained, proceed to next HH. If consent was obtained, proceed to the ``Person Roster Questionnaire. (label) Survey Name : 2_Person_Nam_01_2012 No of Questions:16 ===================================================================== 1:PERSONS ROSTER. Ask about persons slept here last night including non-family members. Start with head of HH or oldest person. Do NOT include usual members of HH if they DID NOT sleep here last night (label) 2:Cluster Number (same as in Household questionnaire) (number) Data Field Name : rp_clusternumber 3:Household number (same as in Household questionnaire) (number) Data Field Name : rp_hhnumber 4:Name of the person (text) Data Field Name : rp_name 5:Line Number of the person in the household (Obtain this from paper Person Roster, column 1, Person Number) (number) Data Field Name : rp_hhpersonnumber 6:Gender (multi) Data Field Name : rp_gender Possible responses: - Male - Female 7:Age in YEARS—Mark zero(0) if less than 12 months old. (Estimate if they do not know, especially for adults) (number) Data Field Name : rp_age 8:Did the child <5 years old have a fever in the last two weeks? (multi) Data Field Name : childfever Possible responses: - Yes - No 27 - Do not know 9:What was done for the child that had fever? (multi) Data Field Name : childfever_typetreat Possible responses: - No treatment - Treated at home - Taken to a health facility - Taken to a chemist or private practitioner - Taken to traditional medicine person 10:Did the child with fever receive a finger or heel stick for blood testing for malaria? (multi) Data Field Name : childfever_blood Possible responses: - Yes - No - Do not know 11:Did the child test positive for malaria? (multi) Data Field Name : Child_malaria_result Possible responses: - Yes - No - Do not know 12:Did the child with fever receive ANY malaria drugs for the fever? (multi) Data Field Name : childfever_anyam Possible responses: - Yes - No - Do not know 13:Did the child with fever receive ACT for the treatment of fever? (multi) Data Field Name : childfever_act 28 Possible responses: - Yes <<>> - No <<>> - Do not know <<>> 14:Did the child with fever receive ACT within 24 hours of having a fever? (multi) Data Field Name : childfever_act24 Possible responses: - Yes - No - Do not know 15:If the child with fever received some malarial drug but not ACT, what was the other malaria drug? (multi) Data Field Name : childfever_otheram Possible responses: - Chloroquine - SP_Fansidar - Quinine - Others - Do not know 16:IF there IS another person who slept here last night click ``Add New Record`` on the next screen. IF NO MORE people, close this questionnaire by clicking option `` Finish for now`` on the next screen. Then proceed to ``Net Roster`` questionnaire. (label) Survey Name : 3_Net_Nam_01_2012 No of Questions: 17 ================================================================ 1:ROSTER OF NETS. I would like to ask you about each bednet that you have in the household (includes all nets that were owned and present in the household last night—Interviewer must enter a new record for each net) (label) 2:Cluster number (same as in Household questionnaire) (number) Data Field Name : rn_clusternumber 3:Household number (same as in Household questionnaire) (number) Data Field Name : rn_hhnumber 29 4:INTERVIEWER ONLY: What net are you collecting information about? If the first net PUT number 1, if the second net PUT number 2, etc. (Use consecutive numbers) (number) Data Field Name : Interviewer_net_info 5:INTERVIEWER ONLY: Ask if you can see this net. Did you observe the net? (multi) Data Field Name : RN_OBSERVENET Possible responses: - Yes - No 6:Was this net hung last night? (Look for evidence of hanging and observe or ask if the net was hanging) (multi) Data Field Name : rn_hangingnet Possible responses: - Yes - No - Do not know 7:How many months ago did your household obtain the mosquito net? (RECORD IN MONTHS. Put "36" for 3 yrs, "48" for 4 yrs, and "60" for >=5yrs. 98=NOT SURE) (number) Data Field Name : re_netagemonths 8:LLIN (Long Lasting Insecticidal Net): is a factory treated net that does not require any further treatment. (label) 9:From where did you obtain this net? (multi) Data Field Name : rn_srce Possible responses: - Mass distribution in a settlement camp in 2011 - Other Mass Distribution - Market/Retail shop - Health facility - Pharmacy - Friend/Relative - Other 10:Brand of the net? (Observe or ask for the brand of net. If the brand is unknown, and you cannot observe the net, show pictures of typical net types/brands to respondent) (multi) Data Field Name : rn_brandnet Possible responses: 30 - Dawa - Permanet - Tana - SuperNet Plus - Other LLIN - Other Non-LLIN - Do not know brand 11:Did anyone sleep under this net last night? (multi) Data Field Name : rn_sleeplastnightyn Possible responses: - Yes - No - Not sure 12:Line number of the first person that slept under this net. (Get this from the paper job aid) (number) Data Field Name : rn_personone 13:Line number of the second person that slept under this net. (Get this from the paper job aid) (number) Data Field Name : rn_persontwo 14:Line number of the third person that slept under this net. (Get this from the paper job aid) (number) Data Field Name : rn_personthree 15:Line number of the fourth person that slept under this net. (Get this from the paper job aid) (number) Data Field Name : rn_personfour 16:Line number of the fifth person that slept under this net. (Get this from the paper job aid) (number) Data Field Name : rn_personfive 17:IF there is another bednet in the household click ``Add New Record`` on the next screen. IF there are NO MORE bednets, close this questionnaire by clicking "Finish for now". Proceed to the NEXT household. (label) 31 1 World Health Organization. The EPI coverage survey. www.who.int/immunization_monitoring/routine/EPI_coverage_survey.pdf. Accessed 30 January 2011. 2 Roll Back Malaria. Malaria Indicator Survey: Basic Documentation for Survey Design and Implementation. http://www.rbm.who.int/partnership/wg/wg_monitoring/docs/mis2005/cc1.pdf. Accessed 30 January 2011. 3 World Health Organization. World Malaria Report 2010. Geneva, Switzerland. 32