Schizophrenia and Schizoaffective Disorders
advertisement

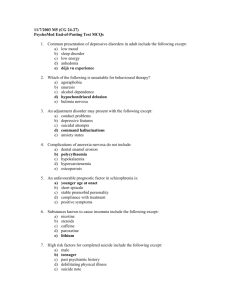
Running Head: Schizophrenia and Schizoaffective Disorders Schizophrenia and Schizoaffective Disorders Rachel Krogstie Dr. Atwater NUR 4/24/2015 1 Schizophrenia and Schizoaffective Disorders Schizophrenia and Schizoaffective Disorders In the newest version of the Diagnostic Statistical Manual of Mental Disorders, the 5th edition (DSM-5), made some notable changes to the diagnoses of schizophrenia and schizoaffective disorder (Malaspina, et al., 2013). For example, for schizophrenia, there is no longer a specific subtypes (Malaspina, et al., 2013). Also, in schizoaffective disorder, the diagnosis goes from an episodic diagnosis to a lifetime diagnosis. This writer will briefly describe the etiology, signs and symptoms, and treatment of both schizophrenia and schizoaffective disorders. Schizophrenia Schizophrenia is a mental disease that affects a person’s thought processes, emotional and social health, and decision making (National Alliance on Mental Illness, 2015). This illness affects about 1% of the population of the United States (National Alliance on Mental Illness, 2015). Etiology Researchers have found no exact cause of schizophrenia. However, there are several different theories on the etiology. Some of these theories include: genetics, environment, brain chemistry, and drug use (National Alliance on Mental Illness, 2015). Signs and symptoms People who have mental illnesses experience signs and symptoms in different ways. Clients with schizophrenia could experience symptoms like: hallucinations, delusions, disorganized thinking, anosognosia, and various negative symptoms (National Alliance on Mental Illness, 2015). Hallucinations can include auditory, visual, and olfactory disturbances (National Alliance on Mental Illness, 2015). Delusions are false beliefs that do not change even 2 Schizophrenia and Schizoaffective Disorders 3 when presented with new (or truthful) ideas (National Alliance on Mental Illness, 2015). This can even manifest in anosognosia, or an unawareness of their illness (National Alliance on Mental Illness, 2015). Schizophrenic clients also display negative symptoms such as flat affect or dull speech (National Alliance on Mental Illness, 2015). Treatment and Nursing Care There are several different routes to treat schizophrenia, but the most common is the pharmacological route. Anti-psychotic medications can relieve the symptoms of psychosis. However, non-pharmacological routes can be just as effective, if not more effective. Nonpharmacological interventions can include psychosocial treatment, psychotherapy, and family support (National Alliance on Mental Illness, 2015). Schizoaffective Disorder Schizoaffective disorder is a chronic mental health condition that is comprised of the symptoms of schizophrenia and a mood disorder (National Alliance on Mental Illness, 2015). Many people are misdiagnosed because this illness shares symptoms from many different conditions (National Alliance on Mental Illness, 2015). Etiology Much like schizophrenia, researchers have not pinpointed an exact cause of schizoaffective disorder. Some of the causes that may contribute to the development of this illness are: genetics, brain chemistry and structure, stress, or drug use (National Alliance on Mental Illness, 2015). Schizophrenia and Schizoaffective Disorders 4 Signs and symptoms The signs and symptoms of schizoaffective disorder are a lot like schizophrenia except with the added signs and symptoms of a mood disorder, like bipolar disorder with mania or depression. The specific symptoms associated with schizoaffective disorder could be depressed mood or manic behavior along with the common symptoms of hallucinations and delusions of schizophrenia (National Alliance on Mental Illness, 2015). Treatment and Nursing Care There are two main therapies for schizoaffective disorder, medication and psychotherapy. There is only one medication approved by the FDA to treat schizoaffective disorder, paliperidone (Invega) (National Alliance on Mental Illness, 2015). However, there are several classes of medication that can treat the symptoms, such as antipsychotics, antidepressants, and mood stabilizers (National Alliance on Mental Illness, 2015). Conclusion In conclusion, while these two illnesses may look a lot alike, they are completely different diagnoses. They have different treatments and managements, and now the DSM-5 reflects those changes. Some of the treatments have severe interactions or contraindications with other treatments and should be monitored closely. It would behoove healthcare professionals, no matter in which field they serve, to be aware of the clinical manifestations and treatments of these illnesses. Schizophrenia and Schizoaffective Disorders 5 References Malaspina, D., Owen, M. J., Heckers, S., Tandon, R., Bustillo, J., Schultz, S., . . . Carpenter, W. (2013). Schizoaffective Disorder in the DSM-5. Schizophrenia Research. Retrieved from http://dx.doi.org/10.1016/j.schres.2013.04.026 National Alliance on Mental Illness. (2015, March). Schizoaffective Disorder. Retrieved from NAMI: National Alliance on Mental Illness: https://www.nami.org/Learn-More/MentalHealth-Conditions/Schizoaffective-Disorder National Alliance on Mental Illness. (2015, March). Schizophrenia. Retrieved from NAMI: National Alliance on Mental Illness: https://www.nami.org/getattachment/LearnMore/Mental-Health-Fact-Sheet-Library/Schizophrenia-Fact-Sheet.pdf Tandon, R., Gaebel, W., Barch, D. M., Bustillo, J., Gur, R. E., Heckers, S., . . . Carpenter, W. (2013). Definition and description of schizophrenia in the DSM-5. Schizophrenia Research. Retrieved from http://dx.doi.org/10.1016/j.schres.2013.05.028 Townsend, M. C. (2014). Essentials of Psychiatric Mental Health Nursing. Philadelphia: F.A. Davis Company. Schizophrenia and Schizoaffective Disorders 6 Appendix A: DSM-5 Criteria Table 1 DSM-5 criteria for Schizoaffective Disorder A. An uninterrupted period of illness during which there is a Major Mood Episode (Major Depressive or Manic) concurrent with Criterion A of Schizophrenia. Note: The Major Depressive Episode must include Criterion A1. B. Depressed mood. Delusions or hallucinations for 2 or more weeks in the absence of a Major Mood Episode (Depressive or Manic) during the lifetime duration of the illness. C. Symptoms that meet criteria for a Major Mood Episode are present for the majority of the total duration of the active and residual portions of the illness. D. The disturbance is not attributable to the effects of a substance or another medical condition. Specify whether: Bipolar Type: This subtype applies if a Manic Episode is part of the presentation. Major Depressive Episodes may also occur. Depressive Type: This subtype applies if only Major Depressive Episodes are part of the presentation. With catatonia: This specifier, which applies to both 295.70 (F25.1) Schizoaffective Disorder, with prominent depressive symptoms, and 295.70 (F25.0) Schizoaffective Disorder, with prominent Manic Symptoms, may be used to specify a current episode with at least three of the following: catalepsy, waxy flexibility, stupor, agitation, mutism, negativism, posturing, mannerisms, stereotypies, grimacing, echolalia, and echopraxia. (Tandon, et al., 2013) Table 2 DSM-5 criteria for Schizophenia A. Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated). (1) Delusions At least one of these should include 1–3 a. Delusions b. Hallucinations c. Disorganized speech d. Grossly disorganized or catatonic behavior e. Negative symptoms (Diminished emotional expression, etc.) B. Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning, such as work, interpersonal relations, or self-care, are markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, failure to achieve expected level of interpersonal, academic, or occupational achievement). C. Duration: Continuous signs of the disturbance persist for at least 6 months. This 6month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or by two or more symptoms listed in Criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences). Schizophrenia and Schizoaffective Disorders 7 D. Schizoaffective and major mood disorder exclusion Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out because either (1) no major depressive or manic episodes have occurred concurrently with the active phase symptoms; or (2) if mood episodes have occurred during active-phase symptoms, their total duration has been brief relative to the duration of the active and residual periods E. Substance/general mood condition exclusion Substance/general medical condition exclusion: The disturbance is not attributed to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition. F. Relationship to Global Developmental Delay or Autism Spectrum Disorder — If there is a history of autism spectrum disorder or other communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations are also present for at least 1 month (or less if successfully treated). (Malaspina, et al., 2013)