Andrew Collins
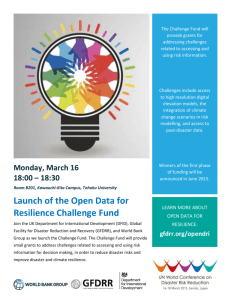
advertisement

Health Centred Disaster Risk Reduction (HCDRR) Theme, Background and Context Dealing with Disasters Conference 17th-18th September Prof. Andrew E. Collins Department of Geography / Disaster and Development Network (DDN) Northumbria University andrew.collins@northumbria.ac.uk Past Dealing with Disasters Conferences 2006: Planning Response and Investigation 2007: Resilience, Response and Investigation 2008: Putting Resilience into Response 2009: Resilience through Local Governance 2010: Linking Disasters and Development: the next 10 years 2011: Reflections on Recent Disasters: the last 10 years 2013: From Opportunity to Action: Bridging the Gap between Disaster Reduction and Development through Science(s), Technology and People Centred Actions 2014: Building Disaster Resilience is Everybody's Business 2015: Health Centred Disaster Risk Reduction: a new agenda for a new era 2 Suggested HCDRR Analytical Framework • How disasters impact on health? • How health mediates disaster and development? • How to deal with complex and uncertain health disasters? 3 Some Research Projects Informing Health Centred Disaster Risk Reduction (HCDRR) 1. Environmental Influences on the Distribution of Incidence of Cholera – spatio-temporal environmental analysis 2. Environment, Health and Population Displacement - hazard, vulnerability and context or health ecology 3. Infectious Disease Risk Management (IDRM) – ecological and social indicators to guide intervention strategies 4. Infectious Disease Risk Reduction – as for 3, concept and capacity 5. Health Security for Disaster Resilience – grounded research 6. Resilience to Wellbeing through Integrated Health Risk Reduction – concept/policy impact British Council UNICEF WHO 4 Simplified notion of change in health and wellbeing through critical incidents People’s resistance to physical and mental stresses or shocks, reduction of poverty and illhealth and presence of basic rights. C A X Y A = Point of disaster B = Lowest point of disaster C = Recovery point at x years Y = Change in (health) indicator due to disaster X = Rate of recovery B Time Collins, A.E. (2006) Health Security for Disaster Resilience, ESRC 5 Health as prerequisite and outcome of disaster and climate risk Health Prerequisite Disaster Risk Management Climate Risk Climate Change Mitigation Health Outcome Climate Change Adaptation Collins, A.E., Abrahams, J. and Murray, V. (2014) ‘Human health, climate risk management and disaster reduction post HFA’, a paper for the Global Assessment Report (GAR) on Disaster Risk Reduction, United Nations: Geneva. Systems of meaning for health disaster reduction and development Cosmology – Faith Based Beliefs – Existential Discourse – Aesthetic Goals Systems of Meaning and Social Relations as Societal Health Disaster and Development Outcomes mediated by: - power and structures - technology and education - human behaviour 7 Systems of meaning and social relations that mediate health, disaster and development Social Relations Support networks – social capital Communication Accountabilities Responsibilities Dependencies Emotional ties Kinship ties Symbioses Empathy Systems of Meaning Intrinsic value of natural systems Intrinsic value of human life Mediation and cooperation Hope and expectation Trust – Mistrust Consciousness Rationality Justice Rights 8 Awakening Healthy societies impact on disaster risk. These societies comprise people who are able to: - get out of the way of disaster - being mobile socially, economically and physically, whilst willing to help those who are not - offset risks with resilience to resurgent and emergent health hazards - maintain aspirations and decision making capacity - motivate towards greater survivability, sustainability and well-being … by dealing with the barriers and transitions within these processes? 9 Policy Implications and Drivers to Accommodate Systemic Progress in Disaster Risk Reduction • Understand boundaries and transitions in health centred disaster risk reduction • Cross disciplinary boundaries to understand influences on persistent, emergent and resurgent health risks • Link practice to theory change – practitioners alongside analysts, survivors, politicians and scientists • Research and learning that heightens awareness, brings behavioural change, enhances capacity building, communication, regulation, innovation and much better financing. 10