ONE2_12_Hand
advertisement
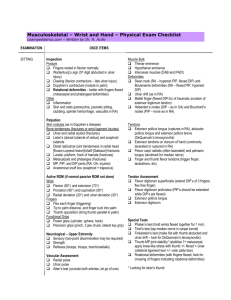
Hand Orthopedic Tests Anterior Aspect Thenar Eminence Antero-Lateral aspect of the hand in anatomical position. Three muscles that move the thumb: Abductor pollcis brevis, opponens pollicis, and flexor pollicis. Innervated by a branch of the median nerve. Prolonged median nerve compression in the carpal tunnel may cause the muscles to atrophy. Thenar Eminence Palpation Palpate the thenar eminence. Look for atrophy in comparison to the opposite hand. If atrophy is present with pain and paresthesia along the medial nerve distribution, suspect compression of the median nerve in the carpal tunnel. Thenar Eminence Hypothenar Eminence Antero-medial aspect of the hand. Three muscles: Abductor digiti minimi, opponens digiti minimi, and flexor digiti minimi. Innervated by a branch of the ulnar nerve. Prolonged compression of the ulnar nerve in Guyon’s tunnel or more proximally in the extremity can cause muscle atrophy. Hypothenar Eminence Palpation Palpate the hypothenar eminence. Look for hypertrophy or atrophy in comparison to the opposite hand. Atrophy may indicate compression of the ulnar nerve in the tunnel of Guyon or more proximally in the extremity. Hypothenar Eminence Posterior Aspect Extensor Tendons The extensor mechanism consists of ligaments, fascial bands, and tendons. They run along the entire length of the posterior aspect of the hand and digits. Trauma can strain or rupture the tendons. Rheumatoid arthritis can displace the tendons. Extensor Tendon Palpation With the patient’s fingers and wrist extended, palpate the length of each tendon of the extensor digitorum communis from the base of the wrist to the proximal phalanx. Note tenderness, cysts, or loss of continuity of the tendons. Tenderness and displacement – rheumatoid arthritis. Extensor Tendon Palpation Loss of continuity after trauma – rupture of tendon Small cysts may develop between the 2nd and 3rd metacarpal bones. Extensor Tendons Metacarpals and Phalanges The metacarpal bones and phalanges are easily palpable from the posterior aspect. Held together by ligaments and joint capsules. Susceptible to traumatic fractures. Common site for rheumatoid arthritis. Palpation of Metacarpals and Phalanges Palpate each individual digit and metacarpal bone. Look for tenderness, swelling, temperature differences, and bony nodules. Tenderness and swelling after trauma – fracture. Swelling around the joint capsule – inflammatory process such as rheumatoid arthritis. Bony nodules (Heberden’s nodes) – osteoarthritis. Palpation of Metacarpals and Phalanges Joint Instability The interphalangeal joints are the most common site of joint injuries to the hand. Joint stability is maintained by the collateral ligaments and the volar plate (three sided box around the joints). The index and little finger are the most affected. Joint instability is usually due to dislocation. Varus and Valgus Stress Test Procedure: Grasp the joint with a pinch grip and with the other hand grasp the adjoining bone. Apply varus and valgus stress to the joint. Positive Test: If pain is elicited, suspect a capsule sprain, subluxation or dislocation. Laxity could be a tear to the joint capsule or collateral ligaments. Varus and Valgus Stress Test Thumb Ulnar Collateral Ligament Laxity Test Procedure: Carpometacarpal joint in extension. Stabilize the metacarpal with a pinch grip. With the opposite hand, grasp the proximal phalanx and push the phalanx radially. Repeat in flexion. Positive Test: When the thumb is fully extended, it normally has 6 degrees of laxity. Greater than 6 degrees – the ulnar collateral ligament and volar plate are damaged. Lax in flexion – ulnar collateral ligament is damaged. No damage in flexion and greater than 30 degrees in extension, damage is limited to volar plate. Thumb Ulnar Collateral Ligament Laxity Test Joint Capsule Tests If the joint capsules are tight, they may have decreased joint motion. Limitations of the intrinsic muscles of the hand or tight collateral ligaments. Rheumatoid arthritis and osteoarthritis can cause this. If the joint capsules are loose, they may have increased joint motion. Bunnel-Littler Test Procedure: Instruct the patient to extend the MCP joint slightly. Attempt to move the proximal interphalangeal joint into flexion. Repeat with the joint in flexion. Positive Test: If the joint does not flex with the MCP in slight extension – tight intrinsic muscle or contracture of the joint capsule. If the joint fully flexes with the MCP in flexion – the intrinsic muscles are tight. Positive test indicates an inflammatory process such as rheumatoid arthritis or osteoarthritis. Bunnel-Littler Test Tendon Instability Tendon instability may be caused by vascular impairment, tenosynovitis, overstretch, or trauma. Trauma to the forearm may injure one or more of the long tendons, which originate in the forearm and flex and extend all of the joints of the fingers. Profundus Test Procedure: Instruct the patient to flex the suspected distal phalanx while you stabilize the proximal phalanx. Positive Test: Inability to flex the distal phalanx indicates a divided flexor digitorum profundus tendon. Profundus Test Flexor and Extensor Pollicis Longus Test Procedure: Stabilize the proximal phalanx of the thumb. Instruct the patient to flex and extend the distal phalanx. Positive Test: Inability to flex the digit – injured flexor pollicis longus. Inability to extend the digit – injured extensor pollicis longus. Flexor and Extensor Pollicis Longus Test Extensor Digitorum Communis Test Procedure: With the fingers flexed, instruct the patient to extend the fingers. Positive Test: Inability to extend any of the fingers indicates an injury to that particular portion of the extensor digitorum communis tendon. Extensor Digitorum Communis Test