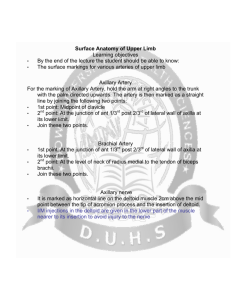
Upper Limb Objectives
advertisement
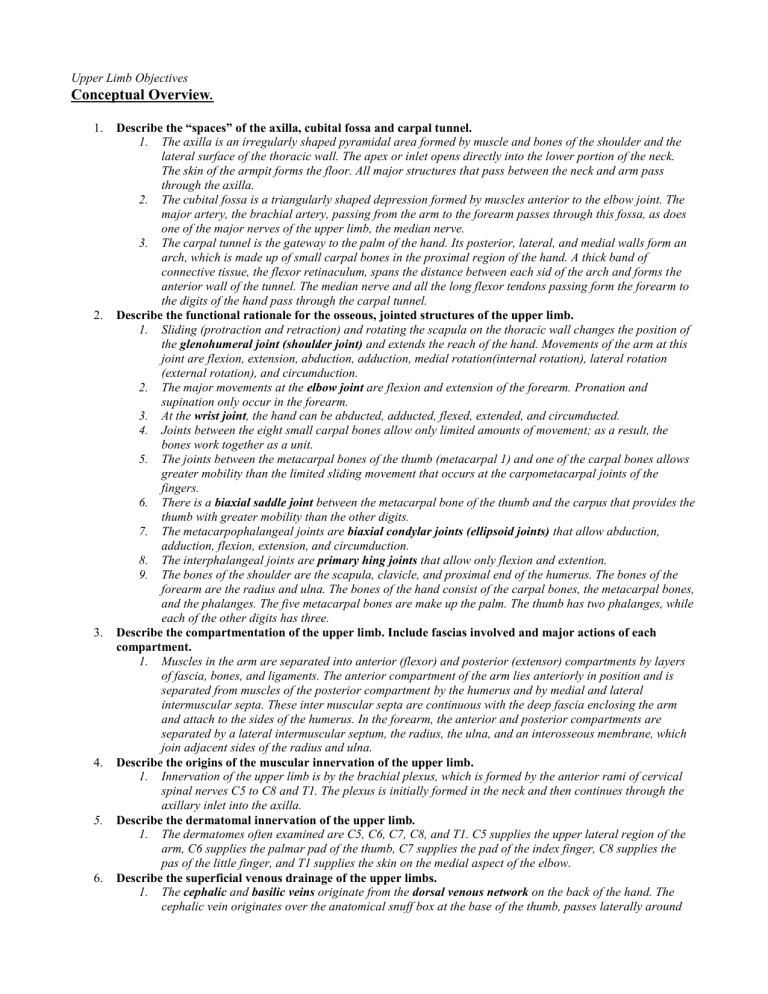
Upper Limb Objectives Conceptual Overview. 1. 2. 3. 4. 5. 6. Describe the “spaces” of the axilla, cubital fossa and carpal tunnel. 1. The axilla is an irregularly shaped pyramidal area formed by muscle and bones of the shoulder and the lateral surface of the thoracic wall. The apex or inlet opens directly into the lower portion of the neck. The skin of the armpit forms the floor. All major structures that pass between the neck and arm pass through the axilla. 2. The cubital fossa is a triangularly shaped depression formed by muscles anterior to the elbow joint. The major artery, the brachial artery, passing from the arm to the forearm passes through this fossa, as does one of the major nerves of the upper limb, the median nerve. 3. The carpal tunnel is the gateway to the palm of the hand. Its posterior, lateral, and medial walls form an arch, which is made up of small carpal bones in the proximal region of the hand. A thick band of connective tissue, the flexor retinaculum, spans the distance between each sid of the arch and forms the anterior wall of the tunnel. The median nerve and all the long flexor tendons passing form the forearm to the digits of the hand pass through the carpal tunnel. Describe the functional rationale for the osseous, jointed structures of the upper limb. 1. Sliding (protraction and retraction) and rotating the scapula on the thoracic wall changes the position of the glenohumeral joint (shoulder joint) and extends the reach of the hand. Movements of the arm at this joint are flexion, extension, abduction, adduction, medial rotation(internal rotation), lateral rotation (external rotation), and circumduction. 2. The major movements at the elbow joint are flexion and extension of the forearm. Pronation and supination only occur in the forearm. 3. At the wrist joint, the hand can be abducted, adducted, flexed, extended, and circumducted. 4. Joints between the eight small carpal bones allow only limited amounts of movement; as a result, the bones work together as a unit. 5. The joints between the metacarpal bones of the thumb (metacarpal 1) and one of the carpal bones allows greater mobility than the limited sliding movement that occurs at the carpometacarpal joints of the fingers. 6. There is a biaxial saddle joint between the metacarpal bone of the thumb and the carpus that provides the thumb with greater mobility than the other digits. 7. The metacarpophalangeal joints are biaxial condylar joints (ellipsoid joints) that allow abduction, adduction, flexion, extension, and circumduction. 8. The interphalangeal joints are primary hing joints that allow only flexion and extention. 9. The bones of the shoulder are the scapula, clavicle, and proximal end of the humerus. The bones of the forearm are the radius and ulna. The bones of the hand consist of the carpal bones, the metacarpal bones, and the phalanges. The five metacarpal bones are make up the palm. The thumb has two phalanges, while each of the other digits has three. Describe the compartmentation of the upper limb. Include fascias involved and major actions of each compartment. 1. Muscles in the arm are separated into anterior (flexor) and posterior (extensor) compartments by layers of fascia, bones, and ligaments. The anterior compartment of the arm lies anteriorly in position and is separated from muscles of the posterior compartment by the humerus and by medial and lateral intermuscular septa. These inter muscular septa are continuous with the deep fascia enclosing the arm and attach to the sides of the humerus. In the forearm, the anterior and posterior compartments are separated by a lateral intermuscular septum, the radius, the ulna, and an interosseous membrane, which join adjacent sides of the radius and ulna. Describe the origins of the muscular innervation of the upper limb. 1. Innervation of the upper limb is by the brachial plexus, which is formed by the anterior rami of cervical spinal nerves C5 to C8 and T1. The plexus is initially formed in the neck and then continues through the axillary inlet into the axilla. Describe the dermatomal innervation of the upper limb. 1. The dermatomes often examined are C5, C6, C7, C8, and T1. C5 supplies the upper lateral region of the arm, C6 supplies the palmar pad of the thumb, C7 supplies the pad of the index finger, C8 supplies the pas of the little finger, and T1 supplies the skin on the medial aspect of the elbow. Describe the superficial venous drainage of the upper limbs. 1. The cephalic and basilic veins originate from the dorsal venous network on the back of the hand. The cephalic vein originates over the anatomical snuff box at the base of the thumb, passes laterally around 7. the distal forearm to reach the anterolateral surface of the limb, and then continues proximally. It crosses the elbow, then passes up the arm into a triangular depression—the clavipectoral triangle (deltopectoral triangle) –between the pectoralis major muscle, deltoid muscle, and clavicle. In this depression, the vein passes into the axilla by penetrating deep fascia just inferior to the clavicle. The basilic vein originates from the medial side of the dorsal venous network of the hand and passes proximally up the posteromedial surface of the forearm. It passes onto the anterior surface of limb just inferior to the elbow and then continues proximally to penetrate deep fascia about midway up the arm. At the elbow, the cephalic and basilic veins are connected by the median cubital vein, which crosses the roof of the cubital fossa. Describe the lymphatic drainage pattern of the upper limb (both right and left). 1. Lymphatic drainage from the right arm drains into the right subclavian trunk and the left arm drains into the left subclavian trunk. Both trunks join their respective right and left subclavian veins. Lymphatic drainage from lateral and superior parts of the breast is predominantly into lymph nodes in the axilla. Several arteries and veins that supply or drain the gland also originate from, or drain into, major axillary vessels. Regional Anatomy of the Upper Limb Shoulder 1. Describe the osseous anatomy of the upper limb. What structures are most at risk in a fracture involving the: surgical neck of the humerus, midshaft humerus, medial epicondyle of the humerus? a. Boney framework of the shoulder consists of the clavicle and scapula (forming the pectoral/ shoulder girdle) and the proximal end of the humerus. i. Clavicle – only boney attachment btwn trunk and UL. S-shaped contour with forward-facing convex portion medial. Medial/ sternal end articulates with the manubrium of the sternum (and 1st costal cartilage), is quadrangular shaped and more robust than the later/acromial end which is flat. Acromial end has small facet for articulation with the median surface of the acromion. Inferior surface of lateral 1/3 has conoid tubercle (attachment of conoid ligament) and trapezoid line (attachment of trapezoid ligament). ii. Scapula – large, flat, triangular. 3 angles (lat, sup, inf), 3 borders (lat, sup, medial), 2 surfaces (costal, posterior) and 3 processes (acromion, spine, coracoid process). Glenoid cavity at lateral angle articulates with the head of the humerus (glenohumeral joint). Infraglenoid tubercle (inferior to glenoid cavity) is the site of attachment for the long head of the triceps brachii muscle. The superglenoid tubercle (superior to the glenoid cavity) is the site of attachment for the long head of the biceps brachii. On the posterior surface – prominent spine begins at medial border and slopes superiolaterally dividing the posterior surface into supraspinous fossa and infraspinous fossa. Porjecting anterolaterally from the spine is the acromion which arches over the glenohumeral joint and articulates with the clavicle. Btwn the lateral angle and spine is the greater scapular notch. On the costal surface – note the subscapular fossa. Lateral border is strong and thick, medial is thin and sharp, superior border contains suprascapular notch just medial to the coracoid process, hook like anterolateral projection (falls inferior to clavicle). iii. Proximal humerus – head is half-sphere, project medial and superiorly to articulate with glenoid cavity of the scapula. anatomical neck is a norrow constriction just distal to the head. greater (lateral) and lesser (anterior) tubercles serve as attachment sitmes for the 4 rotator cuff muscles. Greater tubercle – superior facet attachment of supraspinatus, middle facet attachment of infraspinatus, inferior facet attachment of teres minor. Lesser tubercle – subscapularis attaches. Intertubercular sulcus (bicipital groove) btwn the tubercles, extends inferiorly and provides attachment sites for (lateral to medial) pectoralis major, teres major, and latissimus dorsi. Also holds the tendons of the long head of the biceps brachii and is continuous inferiorly with the V-shaped deltoid tuberosity (attachment of deltoid m.). On medial surface at approx. same level is an attachment site for the corachobrachialis. Surgical neck in horizontal plane btwn head and shaft. The axillary n. and post circumflex humeral artery pass posterior to the surgical neck. Weaker area of the bone. Fractures at… i. Surgical neck – common bc it is a weaker part of the bone. The associated axillary nerve and posterior (and I suppose anterior) circumflex humeral artery can be damaged (but this rarely happens). Test axillary nerve before relocation. ii. Midshaft humerus – radial nerve at risk (in radial groove) with profunda brachii artery iii. Medial epicondyle – The ulnar nerve passes from the arm into the forearm around the posterior surface of the medial epicondyle and can be palpated against the bone in this location (funny bone). iv. supracondylar area – median nerve Describe the attachments, actions and innervation of the muscles of the shoulder. Realize that most should muscles are innervated by C5, C6 – this will be critical to understanding the effects of an upper brachial plexus injury. a. Muscles of the shoulder i. Trapezius 1. Proximal attachment: Superior nuchal line, external occipital protuberance, medial margin of the ligamentum nuchae, spinous processes of CVII to TXII and the related supraspinous ligaments 2. Distal attachment: Superior edge of the crest of the spine of the scapula, acromion, posterior border of lateral one-third of clavicle 3. Innervation: Motor spinal part of accessory nerve [XI]. Sensory (proprioception) anterior rami of C3 and C4 4. Arterial supply: superficial branch of the transverse cervical artery 5. Function: Powerful elevator of the scapula; rotates the scapula during abduction of humerus above horizontal; middle fibers retract scapula; lower fibers depress scapula ii. Deltoid 1. Proximal attachment: Inferior edge of the crest of the spine of the scapula, lateral margin of the acromion, anterior border of lateral one-third of clavicle 2. Distal attachment: Deltoid tuberosity of humerus 3. Innervation: Axillary nerve [C5, C6] 4. Arterial supply: Deltoid branch of the thoracoacromial artery 5. Function: Major abductor of arm (abducts arm beyond initial 15° done by supraspinatus); clavicular fibers assist in flexing the arm; posterior fibers assist in extending the arm iii. Levator scapulae 1. Proximal attachment: Transverse processes of CI and CII vertebrae and posterior tubercles of transverse processes of CIII and CIV vertebrae 2. Distal attachment: Posterior surface of medial border of scapula from superior angle to root of spine of the scapula 3. Innervation: Branches directly from anterior rami of C3 and C4 spinal nerves and by branches [C5] from the dorsal scapular nerve 4. Arterial supply: dorsal scapular artery 5. Function: Elevates the scapula iv. Rhomoid major 1. Proximal attachment: Spinous processes of TII-TV vertebrae and intervening supraspinous ligaments 2. Distal attachment: Posterior surface of medial border of scapula from the root of the spine of the scapula to the inferior angle 3. Innervation: Dorsal scapular nerve [C4, C5] 4. Arterial supply: Dorsal scapular artery 5. Function: Elevates and retracts the scapula v. Rhomboid minor b. 2. 1. b. c. Proximal attachment: Lower end of ligamentum nuchae and spinous processes of CVII and TI vertebrae 2. Distal attachment: Posterior surface of medial border of scapula at the root of the spine of the scapula 3. Innervation: Dorsal scapular nerve [C4, C5] 4. Arterial supply: Dorsal scapular artery 5. Function: Elevates and retracts the scapula Muscles of the posterior scapular region i. Supraspinatus 1. Proximal attachment: Medial two-thirds of the supraspinous fossa of the scapula and the deep fascia that covers the muscle 2. Distal attachment: Most superior facet on the greater tubercle of the humerus 3. Innervation: Suprascapular nerve [C5, C6] 4. Arterial supply: Suprascapular artery 5. Function: Rotator cuff muscle; initiation of abduction of arm to 15° at glenohumeral joint ii. Infraspinatus 1. Proximal attachment: Medial two-thirds of the infraspinous fossa of the scapula and the deep fascia that covers the muscle 2. Distal attachment: Middle facet on posterior surface of the greater tubercle of the humerus 3. Innervation: Suprascapular nerve [C5, C6] 4. Arterial supply: Suprascapular and circumflex scapular arteries 5. Function: Rotator cuff muscle; lateral rotation of arm at the glenohumeral joint iii. Teres minor 1. Proximal attachment: Upper two-thirds of a flattened strip of bone on the posterior surface of the scapula immediately adjacent to the lateral border of the scapula 2. Distal attachment: Inferior facet on the posterior surface of the greater tubercle of the humerus 3. Innervation: Axillary nerve [C5, C6] 4. Arterial supply: Subscapular and circumflex scapular arteries 5. Function: Rotator cuff muscle; lateral rotation of arm at the glenohumeral joint iv. Teres major 1. Proximal attachment: Elongate oval area on the posterior surface of the inferiorangle of the scapula 2. Distal attachment: Medial lip of the intertubercular sulcus on the anterior surface of the humerus 3. Innervation: Inferior subscapular nerve [C5, C6, C7] 4. Arterial supply: Subscapular and circumflex scapular arteries 5. Function: Medial rotation and extension of the arm at the glenohumeral joint v. Long head of triceps brachii 1. Proximal attachment: Infraglenoid tubercle on scapula 2. Distal attachment: Common tendon of insertion with medial and lateral heads on the olecranon process of ulna 3. Innervation: Radial nerve [C6, C7, C8] 4. Arterial supply: Branches of deep brachial artery 5. Function: Extension of the forearm at the elbow joint; accessory adductor and extensor of the arm at the glenohumeral joint Brachial plexus injury – diagnosis requires meticulous clinical history taking and examination. Nerve conduction studies and electromyography are used to assess latency of muscle contraction when nerve is artificially stimulated. Usually blunt force trauma and devastating to function of the UL. Spinal cord 3. 4. injuries (spinal nerves), direct pulling injuries (roots of brachial plexus), trauma to the first rib (trunks), dislocation of glenohumeral joint (divisions and cords) can all affect brachial plexus. Identify the muscles that compose the rotator cuff. What is their importance regarding the glenohumeral (shoulder) stability? What rotator cuff muscle is most often involved in pathology and why? a. Subscapularis i. Proximal attachment: Medial two-thirds of subscapular fossa ii. Distal attachment: Lesser tubercle of humerus iii. Innervation: Upper and lower subscapular nerves [C5,C6, (C7)] iv. Arterial supply: Subscapular artery v. Function: Rotator cuff muscle; medial rotation of the arm at the glenohumeral joint b. Supraspinatus i. Proximal attachment: Medial two-thirds of the supraspinous fossa of the scapula and the deep fascia that covers the muscle ii. Distal attachment: Most superior facet on the greater tubercle of the humerus iii. Innervation: Suprascapular nerve [C5, C6] iv. Arterial supply: Suprascapular artery v. Function: Rotator cuff muscle; initiation of abduction of arm to 15° at glenohumeral joint c. Infraspinatus i. Proximal attachment: Medial two-thirds of the infraspinous fossa of the scapula and the deep fascia that covers the muscle ii. Distal attachment: Middle facet on posterior surface of the greater tubercle of the humerus iii. Innervation: Suprascapular nerve [C5, C6] iv. Arterial supply: Suprascapular and circumflex scapular arteries v. Function: Rotator cuff muscle; lateral rotation of arm at the glenohumeral joint d. Teres minor i. Proximal attachment: Upper two-thirds of a flattened strip of bone on the posterior surface of the scapula immediately adjacent to the lateral border of the scapula ii. Distal attachment: Inferior facet on the posterior surface of the greater tubercle of the humerus iii. Innervation: Axillary nerve [C5, C6] iv. Arterial supply: Subscapular and circumflex scapular arteries v. Function: Rotator cuff muscle; lateral rotation of arm at the glenohumeral joint e. Glenohumeral stability – the multi-axial, synovial, ball in socket joint has a wide range of motion at the cost of skeletal stability. Joint stability is provided by these rotator cuff muscles, the long head of the biceps brachii, related bony processes, and extracapsular ligaments. The tendonds of these rotator cuff muscles blend with the joint capsule and form musculotendinous collar that surrounds the posterior, superior, and anterior aspects of the joint. These muscles stabilize the joint and hold the head of the humerus in the glenoid cavity without compromising range of motion. f. Rotator cuff disorders (p675) – Impingement and tendinopathy. Supraspinatus is most commonly involved as it passes beneath the acromion and acromioclavicular ligament (fixed dimention). Swelling of muscle, excessive fluid in the subacromial/subdeltoid bursae, or acromial bony spurs cause impingent during abduction. Blood supply to the supraspinatus tendon is poor, repeat trauma = degenerative changes and pain. Can result in partial- or full- thickness tears. Trouble with combing hair (abduction). Common is older patients. Discuss the structure/ function relationship between the deltoid and rotator cuff musculature. Which initiates abduction and takes arm to ~15 deg? Which is mainly abduction ~15 to ~90 deg? What muscles and actions are necessary for abduction above 90 degrees? a. First 15 degrees of abduction = supraspinatus b. Beyond 15 through 90 degrees of abduction = deltoid c. Abduction above 90 degrees = trapezius and serratus anterior (abduction above 90 requires upward rotation of the scapula) 5. 6. 7. Discuss the serratus anterior relative to attachments, innervation, and function. What is the clinical scenario when this muscle or nerve is damaged? How can this be assessed by a clinician? What are typical mechanisms of injury? a. Serratus anterior: i. Proximal attachment (posterior): Costal surface of medial border of scapula ii. Distal attachment (anterior/ lateral): Lateral surfaces of upper 8-9 ribs and deep fascia overlying the related intercostal spaces iii. Innervation: Long thoracic nerve [C5, C6, C7] iv. Arterial supply: Circumflex scapular artery v. Function: Protraction and rotation of the scapula; keeps medial border and inferior angle of scapula opposed to thoracic wall b. Damage to the long thoracic nerve (p690) – descends on the lateral thoracic wall, on the external surface of serratus anterior, JUST DEEP TO SKIN AND SUBQ FASCIA, it’s vulnerable! Loss of muscle function allows medial border, esp inferior angle, of the scapula to elevate away from the thoracic wall. Normal elevation of the arm is no longer possible. When a patient pushes forward with the arm they will demonstrate “winging” of the scapula. c. Mechanisms of injury – A blow to the ribs under an outstretched arm, carrying heavy bags over the shoulder for a prolonged time, radical mastectomy w/ removal of axillary node in treatment of breast cancer. Describe the formation of the quadrangular and triangular spaces and identify the structures that traverse them. a. Quadrangular space: i. formed by: 1. the inferior margin of the subscapularis muscle; 2. the surgical neck of the humerus; 3. the superior margin of the teres major muscle; and 4. the lateral margin of the long head of the triceps brachii muscle ii. Passing through the quadrangular space are the axillary nerve and the posterior circumflex humeral artery and vein. b. Triangular space: i. formed by: 1. the medial margin of the long head of the triceps brachii muscle; 2. the superior margin of the teres major muscle; and 3. the inferior margin of the subscapularis muscle. ii. The circumflex scapular artery and vein pass into this space. c. Triangular interval: i. formed by: 1. the lateral margin of the long head of the triceps brachii muscle; 2. the shaft of the humerus; and 3. the inferior margin of the teres major muscle (Fig. 7.45). ii. The radial nerve passes out of the axilla traveling through this interval to reach the posterior compartment of the arm. Profunda brachii artery passes to posterior compartment here. Describe the arterial anastomosis around the shoulder. What segment of the axillary artery could be ligated if necessary while still retaining collateral blood supply to the distal portions of the upper limb? a. Anastomoses in posterior scapular region - Suprascapular artery anastomoses with the circumflex branch of the subscapular a. and the dorsal scapular a. to form the scapular anastomosis. anterior circumflex humeral a. anastomoses with the posterior circumflex humeral a. in the quadrangle space b. Ligation of axillary artery is possible even in most proximal portion because of extensive collateral circulation that exits between thyrocervical trunk of the subclavian artery (suprascapular artery from here) and the subscapular artery, which is branch of distal axillary artery. This anastomosis allows flow w/in subscapular artery to reverse and blood to reach the distal portion of the axillary artery. 8. Understand the clinical items in the section in order to place them in the scenario of a patient presentation – anatomical/ clinical rationale, patient complaints (effects on patient), physical findings (eg gross loss of sensation, muscle weakness…), items pertinent in history (eg, mechanism of injury, typical age/sex/occupation for pathology). a. All summarized in clinical anatomy portion of objectives… Axilla and Pectoral Describe and discuss the regional anatomy of the axilla – structures involved and borders of the region.The axilla is an area of transition between the neck and the arm and is formed by the clavicle, the scapula, the upper thoracic wall, the humerus and related muscles. The axilla is therefore an irregularly-shaped pyramidal space with four sides, an inlet and a base. The axilllary inlet is continuous superiorly with the neck and the lateral part of the floor opens into the arm. The axillary inlet is located superiorly with the following borders: lateral border of rib 1 (medial border), posterior surface of the clavicle (anterior border) and the superior border of the scapula up to the coracoid process (posterior margin). Major vessels and nerves pass over the lateral border of rib 1 (axillary inlet) in order to pass between the neck and arm. The subclavian artery, the major blood vessel supplying the upper limb, becomes the axillary artery as it crosses into the axillary inlet. At the axillary inlet, the axillary vein is anterior to the axillary artery, which is anterior to the trunks of the brachial plexus. The inferior trunk of the brachial plexus lies directly on rib 1 in the neck, as does the subclavian artery and vein. As these vessels pass over rib 1, the vein and artery are separated by the anterior scalene muscle. The axilla has anterior, medial, lateral and posterior walls that are bounded by muscles and fascia. 1. Wall Name of structure Pectoralis major m. Anterior Pectoralis minor m. Subclavius m. Clavipectoral fascia Serratus anterior m. Medial Lateral Intercostobrachial nerve. Intertubercular sulcus of humerus Subscapularis m. Posterior Teres major m. Latissimus dorsi m. Long head of triceps brachii m. Description of these muscles are included in a separate document. There are various triangles, spaces and “gateways” into the axilla, all of which are described below. Name of “Gateway” Borders Contents Quadrangular Space Inferior margin of subscapularis m. Axillary nerve Surgical neck of humerus Posterior circumflex artery Superior margin of teres major m. Lateral margin of long head of triceps Triangular space brachii m. Posterior circumflex vein Medial margin of long head of triceps brachii m. Circumflex scapular artery Superior margin of teres major m. Circumflex scapular vein Inferior margin of subscpularis m. Triangular Interval = deltopectoral triangle Lateral margin of log head of triceps brachii m. Shaft of the humerus Radial nerve Inferior margin of the teres major m. 2. Realize the communication between the axilla and the neck and the structures connecting these two regions. Passing through the axilla are the major vessels, nerves,and lymphatics of the upper limb. The space contains the proximal parts of two muscles of the arm, the axillary process of the breast and collections of lymph nodes. The proximal parts of the bicels brachii and coracobrachialis muscles pass through the axilla. The biceps brachii muscle has two proximal attachments: the short head attaches to the apex of the coracoid process of the scapula and passes vertically through the axilla and into the arm. The long head originates as a tendon from the supraglenoid tubercle of the scapula, passes of the head of the humerus and enters the intertubercular sulcus, passing through the axilla at this point. Further notes on the biceps brachii are included in the muscle/structure document. The coracobrachialis m. originates from the apex of the coracoid process and passes vertically through the axilla to insert on the small linear roughening on the medial aspect of the humerus. In the axilla, the medial surface of the coracobrachialis muscle is pierced by the musculocutaneous nerve that innervates and then passes through this muscle to enter the arm. Other structures that pass through the axilla were mentioned earlier: the axillary artery/vein and their branches (superior thoracic artery, thoracoacromial artery, lateral thoracic artery, subscapular artery, anterior circumflex humeral artery, posteiror circumflex humeral artery & cephalic vein). The brachial plexus and its roots, trunks, divisions, cords and branches. The lymph nodes and the axillary process of the breast are structures attached to the axilla but do not connect with the neck but rather to the thorax. 3. Describe the formation, course, relationships to other structures and termination of the axillary artery and distribution of its branches. The axillary artery supples the walls of the axilla and related regions and continues as the major blood supply to the more distal parts of the upper limb. The subclavian artery becomes the axillary artery at the lateral margin of rib 1 and becomes the brachial artery at the inferior margin of the teres major m. The axillary artery is separated into 3 parts by the pectoralis minor muscle, which crosses anteriorly to the vessel. The first part is proximal to the pectoralis minor m., the second part of the axillary artery is posterior to the muscle, and the third part is distal to the muscle. Part of the Axillary artery Branch of the axillary artery 1st part (proximal to pectoralis minor m.) nd 2 part (posterior to pectoralis minor m.) Superior thoracic artery Thoraco-acromial artery Lateral thoracic artery Subscapular artery 3rd part (distal to the pectoralis minor m.) Anterior circumflex humeral artery Posterior circumflex humeral artery Superior thoracic artery—originates at anterior surface of 1st part of axillary artery and supplies the upper regions of the medial and anterior axillary walls. Thoraco-acromial artery—originates from the anterior surface of the 2nd part of axillary artery. It then curves around the superior margin of the muscle, penetrates the clavipectoral fascia and immediately divides into four branches: the pectoral, deltoid, clavicular and acromial branches. These supply the anterior axillary wall. The pectoral branch goes on to supply the breast and the deltoid branch passes into the clavipectoral triangle where it accompanies the cephalic vein and supplies the adjacent structures. Lateral thoracic artery—arises from the anterior surface of the 2nd part of the axillary artery and follows the margin of the muscle to the thoracic wall and supplies the medial and anterior walls of the axilla. In women , branches emerge from around the inferior margin of the pectoralis major m. and contribute to the vascular supply of the breast. Subscapular artery—originates from the posterior surface of the 3rd part of the axillary artery and is the largest branch of the axillary artery and is the major blood supply to the posterior wall of the axilla. It also contributes to the blood supply of the posterior scapular region. It follows the inferior margin of the subscapularis m. and then divides into two terminal branches: the circumflex scapular artery and thoracodorsal artery. ◦ The circumflex scapular artery passes through the triangular space and posteriorly, it passes below the origin of the teres minor m. to enter the infraspinous fossa. It anastomoses with the suprascapular artery and the deep branch of the transverse cervical artery (dorsal scapular artery). ◦ The thoracodorsal artery follows the lateral border of the scapula to the inferior angle. It contributes to the vascular supply of the posterior and medial walls of the axilla. Anterior circumflex humeral artery—originates from the lateral side of the 3rd part of the axillary artery and passes anterior to the surgical neck of the humerus. It also anastomoses with the posterior circumflex humeral artery. It supplies the glenohumeral joint and the head of the humerus. Posterior circumflex humeral artery—originates from the lateral surface of the 3rd part of the axillary artery immediately posterior to the origin of the anterior circumflex humeral artery. It passes through the quandrangular space and curves around the surgical neck of the humerus, supplying the surrounding muscles and the glenohumeral joint. It anastomoses with the anterior circumflex humeral artery, with branches from the suprascpular and thoraco-acromial arteries. 4. Describe the formation of the axillary vein and list its major tributaries. The axillary vein begins at the lower margin of the teres major m. and is the continuation of the basilic vein. The basilic vein is a superficial vein that drains the posteromedial surface of the hand and forearm and penetrates the deep fascia in the middle of the arm. The axillary vein passes through the axilla medial and anterior to the axillary artery and becomes the subclavian vein as it crosses the lateral border of rib 1. Tributaries of the axillary vein generally follow the branch of the axillary artery. Other tributaries include brachial veins that follow the brachial artery and the cephalic vein. The cephalic vein is a superficial vein that drains the lateral and posterior part of the hand, the forearm and the arm. In the axillary, it passes into the clavipectoral triangle that is bordered by the deltoid m., pectoralis major m. and the clavicle. The cephalic vein passes deep to the clavicular head of the pectoralis major m. and pierces the clavipectoral fascia to join the axillary vein. 5. Describe and discuss the lymphatic drainage of the upper limb and the drainage from these nodes as they reach the central venous circulation. All lymphatics from the upper limb drain into lymph nodes in the axilla. Axillary nodes receive drainage from the adjacent trunk such as regions of the upper back and shoulder, the lower neck, the chest and the upper anterolateral abdominal wall. The 20-30 axillary nodes are generally divided into 5 groups on the basis of location. Humeral (lateral) nodes: posteromedial to the axillary vein and receive most lymphatic drainage from the upper limb. Pectoral (anterior) nodes: along the inferior margin of the pectoralis minor and receives drainage form the abdominal wall, chest and mammary gland. Subscapular (posterior) nodes: on the posterior axillary wall and are associated with the subscapular vessels. These drain the posterior axillary wall and receives lymphatics from the back, shoulder and the neck. Central nodes: embedded in axillary fat, they receive tributaries from humeral, subscapular and pectoral groups of nodes. Apical nodes: most superior group of nodes and drains all other groups of nodes in the region. They receive lymphatic vessels that accompanies the cephalic veins that drain the superior region of the mammary gland. Vessels from the apical group converge to form the subclavian trunk, and joins the venous system at the junction between the right subclavian vein and the right internal jugular vein in the neck. On the left side, the subclavian trunk usually joins the thoracic duct in the base of the neck. 6. Describe and discuss the attachments, actions, and innervation of the muscles in the axillary region. See muscle chart in attached document. 7. Describe the attachments of the fascia which surrounds the pectoralis minor m., its specific specializations. The clavipectoral fascia is a thick sheet of connective tissue that connects the clavicle to the floor of the axilla. It encloses the subclavius m. and pectoralis minor m. and spans the gap between them. Structures pass through the clavipectoral fascia either between the pectoralis minor m. and subclavius m. or inferior to the pectoralis minor m. Important structures that pass between the subclavius and pectoralis minor m. include the cephalic vein, the thoraco-acromial artery and the lateral pectoral nerve. The lateral thoracic artery passes through the fascia inferior to the pectoralis minor m. The medial pectoral nerve penetrates directly through the pectoralis minor m. to supply this muscle and to reach the pectoralis major. 8. 9. Revisit objective #5 from “shoulder”. See objective #5 from shoulder. Understand the clinical items in the section in order to place them in the scenario of a patient presentation— anatomical.clinical rationale, patient complaints, physical findings, items pertinent in history. Damage to the long thoracic nerve—because the long thoracic nerve passes down the lateral thoracic wall on the external surface of the serratus anterior m. This nerve is vulnerable to damage, and loss of function of this muscle causes the medial border of the scapula (particularly the inferior angle) to elevate away from the thoracic wall, resulting in “winging” of the scapula, when the patient is asked to push off a wall with his arms. Furthermore, normal elevation at the arm is not longer possible. The cephalic vein is a superficial vein that drains the lateral and posterior parts of the hand, the forearm and the arm. It passes into the clavipectoral triangle between the deltoid m., pectoralis major m. and the clavicle. In the superior part of the clavipectoral tirangle, the cephalic vein passes deep to the clavicular head of the pectoralis major m. and pierces the clavipectoral fascia to join the axillary vein. Many patients who are critically unwell have lost blood of fluid, which requires replacement. Access to the peripheral vein is necessary to replace fluid; typical sites for venous access are the cephalic vein adjacent to the anatomical snuffbox or the antecubital veins. Imaging the blood supply of the upper limb—Ultrasound is useful tool for carrying assessment of the vessels of the upper limb. Angiography is carried out in certain cases. The femoral artery is punctured below the inguinal ligament, a long catheter is placed through the iliac arteries and around the arch of the aorta to enter either the left subclavian artery or the brachiocephalic trunk and then the right subclavian artery. Contrast agents pass first through the arteries, then the capillaries and finally the veins. Fracture of rib 1—as the subclavian artery passes out of the neck and into the axilla, it is fixed in position by the surrounding muscles in the superior surface of rib 1. A rapid deceleration injury involving upper thoracic trauma may cause a first rib fracture, which may significantly compromise the distal part of the subclavian artery or the first part of the axillary artery. There are anastomotic connections between branches of the subclavian artery and the axillary artery. The arm is therefore rarely rendered completely ischemic. Anterior dislocation of the humeral head—this injury may compress the axillary artery resulting in vessel occlusion. It may be necessary to surgically reconstruct the axillary artery to obtain pain-free function. The axillary artery is also intimately related to the brachial plexus, which may be damaged at the time of anterior dislocation. Subclavian pinch-off syndrome—the “subclavian route” is often the most commonly used route of obtaining venous access for clinicians. This is actually a misnomer since the clinician is using the axillary vein and not the subclavian vein. There are a number of patients that require catheterization of the subclavian/axillary vein. This route is popular for long-term venous access, such as Hickmann lines, and for shorter-term access where multiplelumen catheters are inserted. This site is also the preferred site for insertion of pacemaker wires. A sharp needle used to puncture the skin at the infrascapular region, aimed superomedially. The vein should be punctured in the midclavicular line or lateral to this line. The vein passes anterior to the artery, superior to the first rib and inferior to the clavicle. Beneath the clavicle is situated the subclavius m. Should the puncture of the vein enter where the subclavius m. is related to the axillary vein, the catheter or wire may become kinked at this point and the constant contraction and relaxation of the muscle will induce fatigue in the line and wire, which will ultimately lead to a fracture in the wire. A fractured pacemaker wire or a rupture in a chemotherapy catheter can have severe consequences for the patient. Brachial Plexus: Netter’s Image 1.Describe the formation of the brachial plexus in terms of its roots, trunks, divisions, cords, and branches The brachial plexus is a somatic plexus formed by the anterior rami of C5 to C8, and most of the anterior ramus of T1. It originates in the neck, passes laterally and inferiorly over rib I, and enters the axilla. The parts of the brachial plexus, from medial to lateral, are roots, trunks, divisions, and cords. All major nerves that innervate the upper limb originate from the brachial plexus, mostly from the cords. Proximal parts of the brachial plexus are posterior to the subclavian artery in the neck, while more distal regions of the plexus surround the axillary artery. Roots The roots of the brachial plexus are the anterior rami of C5 to C8, and most of T1. Close to their origin, the roots receive gray rami communicantes from the sympathetic trunk. These carry postganglionic sympathetic fibers onto the roots for distribution to the periphery. The roots and trunks enter the posterior triangle of the neck by passing between the anterior scalene and middle scalene muscles and lie superior and posterior to the subclavian artery. Trunks The three trunks of the brachial plexus originate from the roots, pass laterally over rib I, and enter the axilla • superior trunk is formed by the union of C5 and C6 roots; • middle trunk is a continuation of the C7 root; • inferior trunk is formed by the union of the C8 and T1 roots. Divisions Each of the three trunks of the brachial plexus divides into an anterior and a posterior division Cords The three cords of the brachial plexus originate from the divisions and are related to the second part of the axillary artery • lateral cord results from the union of the anterior divisions of the upper and middle trunks and therefore has contributions from C5 to C7-it is positioned lateral to the second part of the axillary artery; • medial cord is medial to the second part of the axillary artery and is the continuation of the anterior division of the inferior trunk-it contains contributions from C8 and T1; • posterior cord occurs posterior to the second part of the axillary artery and originates as the union of all three posterior divisions-it contains contributions from all roots of the brachial plexus (C5 to T1). Generally, the nerves associated with the anterior compartments of the upper limb arise from the medial and lateral cords and nerves associated with the posterior compartments originate from the posterior cord. 2.Describe the branches from the plexus; including the root origin (ex. C5, C5 for axillary nerve), origin from plexus portions (ex. Axillary nerve from posterior cord, suprascapular nerve from superior trunk), and the compartment/function/muscles served by the branches Answer in next paragraph below. Also, see Table below. 3.Describe the compartmental innervations of the upper limb provided by the terminal branches of the brachial plexus. Understanding & utilizing compartmentalization is critical to efficient studying of the limb. Branches The suprascapular nerve (C5 and C6): • originates from the superior trunk of the brachial plexus; • innervates the supraspinatus and infraspinatus muscles; and • is accompanied by the suprascapular artery. nerve to subclavius muscle (C5 and C6) is a small nerve that: • originates from the superior trunk of the brachial plexus; • passes anteroinferiorly over the subclavian artery and vein; and • innervates the subclavius muscle. Branches of the lateral cord Three nerves originate entirely or partly from the lateral cord • lateral pectoral nerve is the most proximal of the branches from the lateral cord. It innervates the pectoralis major muscle. • musculocutaneous nerve - Innervates all three flexor muscles in the anterior compartment of the arm • lateral root of median nerve is the largest terminal branch of the lateral cord and passes medially to join a similar branch from the medial cord to form the median nerve. Branches of the medial cord The medial cord has five branches: • The medial pectoral nerve is the most proximal branch • The medial cutaneous nerve of arm (medial brachial cutaneous nerve) passes through the axilla. Fibers of the medial cutaneous nerve of arm innervate the upper part of the medial surface of the arm and floor of the axilla. • The medial cutaneous nerve of forearm (medial antebrachial cutaneous nerve) originates just distal to the origin of the medial cutaneous nerve of arm. It innervates skin over the medial surface of the forearm down to the wrist. • The medial root of median nerve passes laterally to join with a similar root from the lateral cord to form the median nerve. • The ulnar nerve is a large terminal branch of the medial cord. The ulnar nerve passes through the arm and forearm into the hand where it innervates all intrinsic muscles of the hand (except for the three thenar muscles and the two lateral lumbrical muscles). On passing through the forearm, branches of the ulnar nerve innervate the flexor carpi ulnaris muscle and the medial half of the flexor digitorum profundus muscle. The ulnar nerve innervates skin over the palmar surface of the little finger, medial half of the ring finger, and associated palm and wrist, and the skin over the dorsal surface of the medial part of the hand. Median nerve The median nerve is formed anterior to the third part of the axillary artery by the union of lateral and medial roots originating from the lateral and medial cords of the brachial plexus. The median nerve continues into the hand to innervate: • the three thenar muscles associated with the thumb; • the two lateral lumbrical muscles associated with movement of the index and middle fingers; and • the skin over the palmar surface of the lateral three and one-half digits and over the lateral side of the palm and middle of the wrist. Branches of the posterior cord Five nerves originate from the posterior cord of the brachial plexus: • the superior subscapular nerve; • the thoracodorsal nerve; • the inferior subscapular nerve; • the axillary nerve; • the radial nerve a. The superior subscapular nerve is short and passes into and supplies the subscapularis muscle. b. The thoracodorsal nerve is the longest of these three nerves. It penetrates and innervates the latissimus dorsi muscle. c. The inferior subscapular nerve innervates the subscapularis and teres major muscles. d. The axillary nerve passes posteriorly around the surgical neck of the humerus and innervates both the deltoid and teres minor muscles. The axillary nerve is accompanied by the posterior circumflex humeral artery. e. The radial nerve is the largest terminal branch of the posterior cord. The radial nerve and its branches innervate: • all muscles in the posterior compartments of the arm and forearm; and • the skin on the posterior aspect of the arm and forearm, the lower lateral surface of the arm, and the dorsal lateral surface of the hand. 4. Which nerves (ex. Median) innervate specific compartments & limb muscles is required knowledge & the overall root levels (ex. C5-T1 for median) that form the nerve are required knowledge. The specific segmental innervations of all muscles is NOT required however (ex. The fact that flexor pollicis longus is only supposedly supplied by C7, C8 fibers from median nerve) Table for Branches of Brachial Plexus Branch (cutaneous) Dorsal scapular Origin: C5 root Spinal segment: C5 Function: motor Rhomboid major, rhomboid minor Function: motor Long thoracic Origin: C5 to C7 roots Serratus anterior Spinal segments: C5 to C7 Suprascapular Origin: Superior trunk Spinal segments: C5, C6 Function: motor Supraspinatus, infraspinatus Nerve to subclavius Origin: Superior trunk Spinal segments: C5, C6 Function: motor Subclavius Function: motor Lateral pectoral Origin: Lateral cord Pectoralis major Spinal segments: C5 to C7 Function: motor Musculocutaneous Origin: Lateral cord All muscles in the anterior compartment of the arm Spinal segments: C5 to C7 Function: sensory Skin on lateral side of forearm Medial pectoral Origin: Medial cord Spinal segments: C8, T1 Function: motor Pectoralis major, pectoralis minor Medial cutaneous of arm Origin: Medial cord Spinal segments: C8, T1 Function: sensory Skin on medial side of distal one-third of arm Medial cutaneous of forearm Origin: Medial cord Spinal segments: C8, T1 Function: sensory Skin on medial side of forearm Median Origin: Medial and lateral cords Spinal segments: (C5), C6 to T1 Function: motor All muscles in the anterior compartment of the forearm (except flexor carpi ulnaris and medial half of flexor digitorum profundus), three thenar muscles of the thumb and two lateral lumbrical muscles Function: sensory Skin over the palmar surface of the lateral three and one-half digits and over the lateral side of the palm and middle of the wrist Ulnar Origin: Medial cord Spinal segments: (C7), C8, T1 Function: motor All intrinsic muscles of the hand (except three thenar muscles and two lateral lumbricals); also flexor carpi ulnaris and the medial half of flexor digitorum profundus in the forearm Function: sensory Skin over the palmar surface of the medial one and one-half digits and associated palm and wrist, and skin over the dorsal surface of the medial one and one-half digits Superior subscapular Origin: Posterior cord Spinal segments: C5, C6 Function: motor Subscapularis Function: motor Thoracodorsal Origin: Posterior cord Latissimus dorsi Spinal segments: C6 to C8 Inferior subscapular Origin: Posterior cord Spinal segments: C5, C6 Function: motor Subscapularis, teres major Axillary Origin: Posterior cord Spinal segments: C5, C6 Function: motor Deltoid, teres minor Function: sensory Skin over upper lateral part of arm Radial Origin: Posterior cord Spinal segments: C5 to C8, (T1) Function: motor All muscles in the posterior compartments of arm and forearm Function: sensory Skin on the posterior aspects of the arm and forearm, the lower lateral surface of the arm, and the dorsal lateral surface of the hand 5.Examine the course of the plexus & its branches in relation to surrounding structures in order to understand common injury scenarios found in the clinical correlation section. Injuries to the brachial plexus The brachial plexus is an extremely complex structure. When damaged, it requires meticulous clinical history taking and examination. Assessment of the individual nerve functions can be obtained by nerve conduction studies and electromyography, which assess the latency of muscle contraction when the nerve is artificially stimulated. Brachial plexus injuries are usually the result of blunt trauma producing nerve avulsions and disruption. These injuries are usually devastating for the function of the upper limb and require many months of dedicated rehabilitation for even a small amount of function to return. Spinal cord injuries in the cervical region and direct pulling injuries tend to affect the roots of the brachial plexus. Severe trauma to the first rib usually affects the trunks. The divisions and cords of the brachial plexus can be injured by dislocation of the glenohumeral joint Arm(brachium) 1. Describe the attachments, action, and innervation of the muscles of the brachium. The muscles of the arm are broken into compartments -anterior contains the coracobrachialis, brachialis, and biceps brachii (two heads) muscles. -posterior contains the triceps brachii (three heads) see attached muscle document 2. Describe the course of nerves from the brachial plexus as they course through the brachium in order to understand their susceptibility to common injury scenarios presented in the text and clinical correlations Four terminal nerve branches travel through the brachium -musculotaneous nerve -passes through the coracobrachialis muscle then diagonally down the arm between the biceps and brachialis muscles -continues as the lateral cutaneous nerve of the forearm -innervates muscles of the anterior arm and sensory innervation to the skin on lateral forearm -median nerve -enters brachium at inferior margin of the teres major muscle and travels vertically down the medial portion of the anterior compartment of arm -in proximal regions is immediately lateral to brachial artery and in distal regions the nerve crosses to the medial side of the brachial artery and lies anterior to the elbow joint. -ulnar nerve -enters arm with median nerve and axillary artery. It then penetrates the medial intermuscular septum where it enters the posterior compartment and lies anterior to the medial tricep head. It passes posteriorly to the medial epicondyle of the humerus and into the anterior compartment of the forearm. -no branches in the brachium -radial nerve -enters arm crossing the inferior margin of the teres major muscle where it lies posterior to the brachial artery. -the profunda brachii artery travels with the radial nerve as it passes the posterior compartment of the arm through the triangular interval. In the posterior compartment it passes diagonally from medial to lateral and lies in the radial groove on the humerus. -On the lateral portion of the arm, the radial nerve passes anteriorly through the intermusclular septum. Here it lies between the brachialis muscle and the muscles of the posterior compartment of the forearm. It enters the forearm anteriorly to the lateral epicondyle of the humerus. -muscular branches in the arm include those to the triceps brachii, brachioradialis, and extensor carpi radialis longus muscles. It also innervates the lateral part of the brachialis. -cutaneous branches of the radial nerve originate in the posterior compartment and include the inferior lateral cutaneous nerve of the arm and the posterior cutaneous nerve of the forearm. Both travel through the lateral head of the tricep to become subcutaneous. 3. Describe the arterial distribution of the brachium and sites for obtaining a patient pulse. Two major arteries of the upper arm -brachial artery -found in anterior compartment and is a continuation of the axillary artery beginning at the lower border of the teres major muscle. It ends just distal to the elbow where it becomes the radial and ulnar arteries. -In proximal arm the brachial artery lies on the medial side but then moves laterally to travel between the epicondyles on the humerus where it crosses the elbow joint anteriorly just medial to the tendon of the biceps brachii. -can be palpated along its length and blood pressure is taken here as the artery can be compressed against the medial side of the humerus. -branches of the brachial artery include some to adjacent muscles as well as two ulnar collateral vessels and the profunda brachii artery. Some branches also supply blood to the humerus. -profunda brachii artery -largest branch of the brachial artery supplies the posterior compartment of the arm by entering this compartment with the radial nerve as they pass through the triangular interval. They pass along the radial groove. -branches supply adjacent muscles and anastomose with the posterior circumflex humeral artery. 4. Identify the arteries of the brachium that participate in anastomis of the elbow. What is the significance of this arrangement. The superior and inferior ulnar collateral arteries that branch from the brachial artery pass the elbow on the medial portion of the arm. The recurrent radial artery and the middle collateral artery (posterior surface) which are the profunda brachii artery that splits into two, travel down the lateral portion of the arm around the elbow joint. The importance of this arrangement is that when the arm is flexed and the brachial artery is pinched, there is still blood supply entering the forearm through the tributaries mentioned above. 5. Describe and discuss the superficial and deep venous circulation of the upper limb and the formation of the axillary vein from its major tributaries Deep paired brachial veins pass along side of the brachial artery in the deep arm. There are two large subcutaneous veins -basilic -this vein passes vertically in the distal half of the arm and penetrates the deep fascia to become medial to the brachial artery. The deep brachial veins join the basilic vein just above the elbow -cephalic -this vein passes superiorly on the anterolateral portion of the arm The basilic vein is what the axillary vein is renamed once it travels out of the axilla region. Before the name change, the cephalic vein branches off the axillary vein superiorly to the pectoral minor muscle. Cubital fossa. 1. 2. Identify and describe the boundaries and contents of the cubital fossa. How can this information assist in competent venipuncture in this region? 1. The lateral border is the brachioradialis muscle, the medial border is the pronator teres muscle, and the base of the triangular cubital fossa is an imaginary horizontal line between the medial and lateral epicondyles. The floor of the fossa is formed by the brachialis muscle. The roof of the cubital fossa is formed by superficial fascia and skin. 2. The major contents, from lateral to medial, are: (1) the tendon of biceps brachii muscle, (2) the brachial artery, and (3) the median nerve. The radial nerve runs deep the brachioradialis muscle and divides into superior and deep branches at the fossa. The roof contains the medial cubital vein, the medial cutaneous and the lateral cutaneous nerves of the forearm. 3. The bicipital aponeurosis covers the brachial artery and median nerve in the distal part of the cubital fossa. The bicipital aponeurosis is between the medial side of the tendon of biceps brachii muscle and deep fascia of the forearm. The structure may be palpable. It separates the median cubital vein from the brachial artery and median nerve. 4. The cephalic vein is used for venipuncture. It courses over the lateral edge of the cubital fossa. Identify the vascular structures that cross the roof of the cubital fossa. How could an aberrant superficial ulnar artery in this region complicate venipuncture? 1. The brachial artery normally bifurcates into the radial and ulnar arteries in the apex of the fossa, but this can occur as high as the axilla (remember Dr. Seibert saw this during a dissection). The brachial artery is used for taking blood pressure. 2. The medial cubital vein lies within the roof of the cubital fossa and will connect the cephalic and basilic veins of the upper limb. 3. In the image, you can see the “normal” course of the cephalic vein and the ulnar artery. Remember, a split of the brachial artery into the ulnar and radial arteries commonly occurs higher up. The cephalic vein and ulnar artery may be closer together on some patients than others. Puncturing the ulnar artery can lead to excessive bleeding and damage to the area. Forearm 1. Describe and discuss the muscles of the forearm in terms of compartments that share an innervation, function, and general attachment. Any exceptions to compartmental characteristics should be highlighted.. Forearm has anterior and posterior compartments -anterior compartment flexes the wrist and digits and pronate hand -most muscles share a proximal attachment at the medial epicondyle of the humerus and are innervated by the medial nerve. -exceptions to this attachment include the deep muscles of the forearm including the flexor digitorum profundus, flexor pollicis longus, and pronator quadratus. -expections to the innervation include the flexor digitorum profundus and the Flexor carpi ulnaris. The medial half of the flexor digitorum profundus is innervated by the ulnar nerve as is the entire flexor carpi ulnaris. -posterior compartment extend the wrist and digits and supinate the hand -most muscles share a proximal attachment at the lateral epicondyle of the humerus and are -innervated by the posterior interosseous nerve. -exceptions to the attachment include the abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and the extensor indicis which all are attached to the bones of the forearm. -exceptions to the innervations include the brachioradialis, extensor carpi radialis longus, the extensor carpi radialis brevus, and the alconeus. These are innervated by the radial nerve. -It is also important to not that the brachioradialis is in the posterior compartment of the arm but is a flexor muscle. -boundaries of the compartments -intermuscular septum -interosseous membrane -ulna deep fascia 2. Flexor compartment muscles see attached muscle document 3. Extensor compartment muscles see attached muscle document 4. Describe the structures forming the carpal tunnel and identify the structures that course through this tunnel -Formed by flexor retinaculum (anterior) and carpal bones (posterior) -the carpal bones include the pisiform and hamate medially, and the scaphoid and trapezium laterally. -Also transmits the Median Nerve and the Tendons of Flexor Pollicis Longus, Flexor Digitorum Profundus(four), and Flexor Digitorum Superficialis(four) -each of the tendons is surrounded by synovial sheath so that they have free movement in the tunnel -the median nerve is anterior to the tendons as you can see below the structure is not expandable and therefore inflammation internally causes carpal tunnel syndrome -the ulnar artery, ulnar nerve, and the tendon of the palmaris longus pass anterior to the tunnel 5. Describe the extensor retinaculum and the flexor retinaculum(transverse carpal ligament). What function do these structures serve? What is the consequence of edema in structures passing beneath the retinaculum. The flexor retinaculum is a thick connective tissue ligament that bridges the space between the medial and lateral sides of the arch and turns the carpal arch into the carpal tunnel. It holds the tendons to the bony plane at the wrist so they do no bow. The extensor retinaculum is connective tissue on the lateral, medial, and dorsal part of the wrist that breaks it into six compartments as seen above. The dorsal portion of the wrist contains tendons of the extensor digitorum and extensor indicis that share a sheath. The extensor carpi ulnaris and extensor digiti minimi tendons are on the medial side of the wrist in separate sheaths. The tendons of the abductor pollicis longus and the extensor pollicis brevis, the extensor carpi radialis longus and the extensor pollicis longus pass through the lateral portion of the dorsal wrist. When there is edema in either portion of the wrist, the tendons within the retinacula are pinched and cause weakness in movement of the wrist and hand as well as the above mentioned carpal tunnel syndrome caused by pressure on the median nerve. Both of these structures hold the tendons tight to the wrist bones to prevent bowing. 6. Describe the formation of the anatomical snuffbox. What tendons form its posterior and anterior limits, what artery passes through, what bone is in its floor, and what vein and nerve pass superficially? What is the clinical significance of pain upon palpation in this region? What is the clinical significance of pain in the anterior bordering tendons upon ulnar deviation? -a triangular depression formed on the posteriolateral side of the wrist and metacarpal I. The base of the triangle is at the wrist and the apex directed into the thumb. -it is formed by -tendons of the abductor pollicis longus and extensor pollicis brevis laterally -tendons of the extensor pollicis longus laterally -the trapezium and the scaphoid bones form the floor along with the distal ends of the extensor carpi radialis longus and extensor carpi radialis brevis -the radial artery passes obliquely through the snuffbox -terminal parts of the superficial branch of the radial nerve pass through subcutaneously as well as the origin of the cephalic vein from the dorsal venous arch of the hand -when there is ulnar deviation the scaphoid bone becomes palpable through the snuffbox. -pain can indicate fracture or more commonly pain associated with tenosynovitis of tendons. This is tested by the Finkelstein's test. 7. describe the course and branches of the arterial supply to the forearm. Where are they more susceptible to injury? Where would pulse be assessed? The largest arteries in the forearm are in the anterior compartment and pass distally to supply the hand and give rise to vessels that supply the posterior compartment. The brachial artery splits into two vessels in the forearm -radial artery -passes along the lateral aspect of the forearm just deep to the brachioradialis muscle, runs with the superficial branch of the radial nerve, and medial to the tendon of the brachioradialis muscle -covered only by deep and superficial fascia and skin on the distal forearm making it susceptible to injury -lies immediately lateral to the flexor carpi radialis tendon and is directly anterior to the pronator quadratus muscle. The pulse can easily be felt here on the lateral portion of the anterior wrist. -The artery passes around the lateral side of the wrist and supply blood to the thumb and lateral side of the index finger -branches of the radial artery -radial recurrent artery- anastomoses around the elbow and supplies muscles on the lateral forearm -palmar carpal- contributes to an anastomoses that supply carpal bones and joints -superficial palmar branch- pass superficial to or through the thenar muscles of the thumb which anastomoses with the superficial palmar arch connecting to the ulnar artery -ulnar artery -larger than the radial artery and passes down the medial aspect of the forearm deep to the pronator teres and travels through the forearm between the flexor carpi ulnaris and the flexor digitorum profundus. -not easily palpable as it remains tucked under the flexor carpi ulnaris tendon -in distal forearm is immediately medial to the ulnar nerve then passes into the hand lateral to the pisiform and superficial to the flexor retinaculum. -supplies medial 3 and a half fingers -branches of the ulnar artery -ulnar recurrent artery with anterior and posterior branches contribute to the anastomoses around the elbow -muscular arteries -common interosseous artery which divides into the anterior(supplies deep anterior compartment and radius and ulna) and posterior branches -two small carpal arteries which supply the wrist 8. Discuss the path and relationships of the median, radial, and ulnar nerves relative to muscles bones, and arteries. Where are they most susceptible to injury and what would signs/symptoms in the patient presenting with such an injury? -Anterior compartment contains the median and ulnar nerves as well as the superficial branch of the radial nerve -median nerve innervates muscles in the anterior compartment except for the flexor carpi ulnaris and the medial part of the flexor digitorum profundus -passes between the two heads of the pronator teres muscle and between the flexor digitorum superficialis muscle heads -just above the wrist it moves to the lateral side of the above mentioned muscle and becomes more superficial lying between the tendons of the palmaris longus and flexor carpi radialis. It then passes through the carpal tunnel -branches of median nerve -anterior interosseuous branch- largest branch and originates between the two heads of the pronator teres and travels down with the anterior interoseous artery -innervates muscles in deep layer and ends as articular branches to joints of the distal forearm and hand -palmar branch originates in distal forearm just proximal to the flexor retinaculum and innervates the skin over the central palm -ulnar nerve -most of its major branches occur in the hand -in the forearm it only innervates the flexor carpi ulnaris and the medial part of the flexor digitorum profundus -the ulnar nerve enters the anterior compartment of the forearm by passing posteriorly around the medial epicondyle of the humerus and between the humeral and ulnar heads of the flexor carpi ulnaris muscle. After passing down the medial side of the forearm in the plane between the flexor carpi ulnaris and the flexor digitorum profundus muscles, it lies under the lateral lip of the tendon of the flexor carpi ulnaris proximal to the wrist. -the ulnar artery is lateral to the ulnar nerve in the distal two-thirds of the forearm, and both the ulnar artery and nerve enter the hand by passing superficial to the flexor retinaculum and immediately lateral to the pisiform bone. -branches -muscular branches to the flexor carpi ulnaris and to the medial half of the flexor digitorum profundus that arise soon after the ulnar nerve enters the forearm; and - two small cutaneous branches-the palmar branch originates in the middle of the forearm and passes into the hand to supply skin on the medial side of the palm; the larger dorsal branch originates from the ulnar nerve in the distal forearm and passes posteriorly deep to the tendon of the flexor carpi ulnaris and innervates skin on the posteromedial side of the back of the hand and most skin on the posterior surfaces of the medial one and one-half digits. -radial nerve -The radial nerve bifurcates into deep and superficial branches under the margin of the brachioradialis muscle in the lateral border of the cubital fossa. -branches of the radial nerve -The deep branch is predominantly motor and passes between the two heads of the supinator muscle to access and supply muscles in the posterior compartment of the forearm. -The superficial branch of the radial nerve is sensory. It passes down the anterolateral aspect of the forearm deep to the brachioradialis muscle and in association with the radial artery. Approximately two-thirds of the way down the forearm, the superficial branch of the radial nerve passes laterally and posteriorly around the radial side of the forearm deep to the tendon of the brachioradialis. The nerve continues into the hand where it innervates skin on the posterolateral surface. Hand 1. Describe the contents of the hand from superficial to deep and medial to lateral (intrinsic and extrinsic muscles, bursae, vessels, and nerves) The hand is the region of the upper limb distal to the wrist joint. It is subdivided into three parts: The (1) wrist (carpus); (2) the metacarpus; and (3) the digits (five fingers including the thumb). The hand has an anterior surface (palm) and a dorsal surface (dorsum of hand). Bones There are three groups of bones in the hand: (1) the eight carpal bones are the bones of the wrist; (2) the five metacarpals (I to V); (3) the phalanges are the bones of the digits-the thumb has only two, the rest of the digits have three.. The metacarpal bone of the thumb functions independently and has increased flexibility at the carpometacarpal joint to provide opposition of the thumb to the fingers. Carpal bones Proximal row From lateral to medial, the proximal row of bones consists of: scaphoid, lunate, triquetrum, pisiform. Distal row From lateral to medial, the distal row of carpal bones consists of: trapezium, trapezoid, capitate, and hamate. Metacarpals Each of the five metacarpal bones is related to one digit: metacarpal I is related to the thumb; metacarpals II to V are related to the index, middle, ring, and little fingers, respectively Each metacarpal consists of a base, a shaft (body), and distally, a head. Phalanges The phalanges are the bones of the digits the thumb has 2 proximal and a distal phalanx; the rest of the digits have 3-a proximal, a middle, and a distal phalanx. Each phalanx has a base, a shaft (body), and distally, a head. Palmar aponeurosis The palmar aponeurosis is a condensation of deep fascia that covers the palm and is anchored to the skin. The apex of the triangle is continuous with the palmaris longus tendon, when present; otherwise, it is anchored to the flexor retinaculum. From this point, fibers radiate to extensions at the base of the digits that project into each of the index, middle, ring, and little fingers and, to a lesser extent, the thumb. Palmaris brevis The palmaris brevis, a small intrinsic muscle of the hand that overlies the hypothenar muscles, ulnar artery, and superficial branch of the ulnar nerve at the medial side of the palm. The palmaris brevis is innervated by the superficial branch of the ulnar nerve. Extensor hoods The tendons of the extensor digitorum and extensor pollicis longus muscles pass onto the dorsal aspect of the digits and expand over the proximal phalanges to form complex "extensor hoods" or "dorsal digital expansions". The tendons of the extensor digiti minimi, extensor indicis, and extensor pollicis brevis muscles join these hoods. In addition to other attachments, many of the intrinsic muscles of the hand insert into the free margin of the hood on each side. By inserting into the extensor hood, these intrinsic muscles are responsible for complex delicate movements of the digits that could not be accomplished with the long flexor and extensor tendons alone. The ability to flex the metacarpophalangeal joints, while at the same time extending the interphalangeal joints, is entirely due to the intrinsic muscles of the hand working through the extensor hoods. Carpal tunnel The carpal tunnel is formed anteriorly at the wrist by a deep arch formed by the carpal bones and the flexor retinaculum. The four tendons of the flexor digitorum profundus, the four tendons of the flexor digitorum superficialis, and the tendon of the flexor pollicis longus pass through the carpal tunnel, as does the median nerve. The median nerve is anterior to the tendons in the carpal tunnel. 2. Describe the functions of the intrinsic hand muscles as well as their attachments and innervations. Realize that all intrinsic hand muscles are innervated by T1 with some contribution from C8 – this will be critical to understanding the effects of a lower brachial plexus injury. see attached muscle document Muscles The intrinsic muscles of the hand are the palmaris brevis, interossei, adductor pollicis, thenar, hypothenar, and lumbrical muscles. Unlike the extrinsic muscles that originate in the forearm, insert in the hand, and function in forcefully gripping ("power grip") with the hand, the intrinsic muscles occur entirely in the hand and mainly execute precision movements ("precision grip") with the fingers and thumb. All of the intrinsic muscles of the hand are innervated by the deep branch of the ulnar nerve except for the three thenar and two lateral lumbrical muscles, which are innervated by the median nerve. The intrinsic muscles are predominantly innervated by spinal cord segment T1 with a contribution from C8. Interosseous Muscles The interossei are muscles between and attached to the metacarpals. They insert into the proximal phalanx of each digit and into the extensor hood and are divided into two groups, the dorsal interossei and the palmar interossei. All of the interossei are innervated by the deep branch of the ulnar nerve. Collectively, the interossei abduct and adduct the digits and contribute to the complex flexion and extension movements generated by the extensor hoods. Dorsal interossei Dorsal interossei are the most dorsally situated of all of the intrinsic muscles and can be palpated through the skin on the dorsal aspect of the hand There are four bipennate dorsal interosseous muscles between, and attached to, the shafts of adjacent metacarpal bones. Each muscle inserts both into the base of the proximal phalanx and into the extensor hood of its related digit. Palmar interossei The four palmar interossei are anterior to the dorsal interossei, and are unipennate muscles originating from the metacarpals of the digits. The palmar interossei adduct the thumb, index, ring, and little fingers with respect to a long axis through the middle finger. The movements occur at the metacarpophalangeal joints. Because the muscles insert into the extensor hoods, they also produce complex flexion and extension movements of the digits Adductor pollicis The adductor pollicis is a large triangular muscle anterior to the plane of the interossei that crosses the palm. It originates as two heads: (1) a transverse head from the anterior aspect of the shaft of metacarpal III; (2) an oblique head, from the capitate and adjacent bases of metacarpals II and III. The radial artery passes anteriorly and medially between the two heads of the muscle to enter the deep plane of the palm and form the deep palmar arch. The adductor pollicis is a powerful adductor of the thumb and opposes the thumb to the rest of the digits in gripping. Thenar muscles The three thenar muscles (the opponens pollicis, flexor pollicis brevis, and abductor pollicis brevis muscles) are associated with opposition of the thumb to the fingers and with delicate movements of the thumb and are responsible for the prominent swelling (thenar eminence) on the lateral side of the palm at the base of the thumb. The thenar muscles are innervated by the recurrent branch of the median nerve. Opponens pollicis The opponens pollicis muscle is the largest of the thenar muscles The opponens pollicis rotates and flexes metacarpal I on the trapezium, so bringing the pad of the thumb into a position facing the pads of the fingers. Abductor pollicis brevis The abductor pollicis brevis muscle overlies the opponens pollicis and is proximal to the flexor pollicis brevis muscle. The abductor pollicis brevis abducts the thumb, principally at the metacarpophalangeal joint. Its action is most apparent when the thumb is maximally abducted and the proximal phalanx is moved out of line with the long axis of the metacarpal bone. Flexor pollicis brevis The flexor pollicis brevis muscle is distal to the abductor pollicis brevis. The flexor pollicis brevis flexes the metacarpophalangeal joint of the thumb. Hypothenar muscles The hypothenar muscles (the opponens digiti minimi, abductor digiti minimi, and flexor digiti minimi brevis) contribute to the swelling (hypothenar eminence) on the medial side of the palm at the base of the little finger. The hypothenar muscles are similar to the thenar muscles in name and in organization. Unlike the thenar muscles, the hypothenar muscles are innervated by the deep branch of the ulnar nerve and not by the recurrent branch of the median nerve. Opponens digiti minimi The opponens digiti minimi muscle lies deep to the other two hypothenar muscles. Abductor digiti minimi The abductor digiti minimi muscle overlies the opponens digiti minimi.The abductor digiti minimi is the principal abductor of the little finger. Flexor digiti minimi brevis The flexor digiti minimi brevis muscle is lateral to the abductor digiti minimi. The flexor digiti minimi brevis flexes the metacarpophalangeal joint. Lumbrical muscles There are four lumbrical (worm-like) muscles, each of which is associated with one of the fingers. The lumbricals are unique because they link flexor tendons with extensor tendons. Through their insertion into the extensor hoods, they participate in flexing the metacarpophalangeal joints and extending the interphalangeal joints. The medial two lumbricals are innervated by the deep branch of the ulnar nerve; the lateral two lumbricals are innervated by digital branches of the median nerve. 3. Intrinsic hand muscles (ex. Mm. that have original & insertion in hand)” a. Specific knowledge of distal attachments is required as in text b. Specific knowledge of proximal attachments is NOT required see attached muscle document 4. Describe the formation of the superficial and deep arterial arches relative to their origin, major contributors, size, location in the palm and the branches provided in the palm and fingers. Where are they susceptible to injury & palpation? Arteries The blood supply to the hand is by the radial and ulnar arteries, which form two interconnected vascular arches (superficial and deep) in the palm. Vessels to the digits, muscles, and joints originate from the two arches and the parent arteries: the radial artery contributes substantially to the supply of the thumb and the lateral side of the index finger; the remaining digits and the medial side of the index finger are supplied mainly by the ulnar artery. Ulnar artery and superficial palmar arch The ulnar artery and ulnar nerve enter the hand on the medial side of the wrist. One branch of the ulnar artery in the hand is the deep palmar branch and anastomoses with the deep palmar arch derived from the radial artery. Branches from the superficial palmar arch include: a palmar digital artery to the medial side of the little finger; and three large, common palmar digital arteries, which ultimately provide the principal blood supply to the lateral side of the little finger, both sides of the ring and middle fingers, and the medial side of the index finger; they are joined by palmar metacarpal arteries from the deep palmar arch before bifurcating into the proper palmar digital arteries, which enter the fingers. Radial Artery The radial artery is on the lateral side of the wrist, passes over the floor of the anatomical snuffbox and into the deep plane of the palm. It also leads to the deep plane of the palm to form the deep palmar arch. The deep palmar arch passes medially through the palm between the metacarpal bones and the long flexor tendons of the digits. On the medial side of the palm, it communicates with the deep palmar branch of the ulnar artery Before penetrating the back of the hand, the radial artery gives rise to two vessels: a dorsal carpal branch, which passes medially as the dorsal carpal arch, across the wrist and gives rise to dorsal metacarpal arteries, which subsequently divide to become small dorsal digital arteries, which enter the fingers; Two vessels, the princeps pollicis artery and the radialis indicis artery, arise from the radial artery. The princeps pollicis artery is the major blood supply to the thumb, and the radialis indicis artery supplies the lateral side of the index finger. The deep palmar arch gives rise to: three palmar metacarpal arteries, which join the common palmar digital arteries from the superficial palmar arch; and three perforating branches, which pass posteriorly between the heads of origin of the dorsal interossei to anastomose with the dorsal metacarpal arteries from the dorsal carpal arch. 5. Describe the motor & sensory distribution of the nerves of the hand; be able to describe the dermatome for the nerve (ex. Median n) and specific cord levels of sensory supply (ex. C7 distribution). What function would be weak or lost in a patient presenting with injury to a specific muscle, group of muscles or nerves supplying hand muscles. Would there be any different findings if the nerve was injured at the wrist or the at the elbow? Nerves The hand is supplied by the ulnar, median, and radial nerves. All three nerves contribute to cutaneous or general sensory innervation. The ulnar nerve innervates all intrinsic muscles of the hand except for the three thenar muscles and the two lateral lumbricals, which are innervated by the median nerve. The radial nerve only innervates skin on the dorsolateral side of the hand. Ulnar nerve The ulnar nerve enters the hand lateral and posteromedially to the ulnar artery. Immediately distal to the pisiform, it divides into a deep branch, which is mainly motor and a superficial branch, which is mainly sensory. The deep branch of the ulnar nerve passes with the deep branch of the ulnar artery. As the deep branch of the ulnar nerve passes across the palm, it lies in a fibro-osseous tunnel (Guyon's canal) between the hook of the hamate and the flexor tendons. Occasionally, small outpouchings of synovial membrane (ganglia) from the joints of the carpus compress the nerve within this canal, producing sensory and motor symptoms. The superficial branch of the ulnar nerve innervates the palmaris brevis muscle and continues across the palm to supply skin on the palmar surface of the little finger and the medial half of the ring. Median nerve The median nerve is the most important sensory nerve in the hand because it innervates skin on the thumb, index and middle fingers, and lateral side of the ring finger. The median nerve also innervates the thenar muscles that are responsible for opposition of the thumb to the other digits. The median nerve enters the hand by passing through the carpal tunnel and divides into a recurrent branch and palmar digital branches. The recurrent branch of the median nerve innervates the three thenar muscles. The palmar digital nerves cross the palm deep to the palmar aponeurosis and the superficial palmar arch and enter the digits. They innervate skin on the palmar surfaces of the lateral three and one-half digits and cutaneous regions over the dorsal aspects of the distal phalanges (nail beds) of the same digits. In addition to skin, the digital nerves supply the lateral two lumbrical muscles. Radial Nerve The only part of the radial nerve that enters the hand is the superficial branch. It enters the hand by passing over the anatomical snuffbox on the dorsolateral side of the wrist. The superficial branch of the radial nerve innervates skin over the dorsolateral aspect of the palm and the dorsal aspects of the lateral three and one-half digits distally to approximately the terminal interphalangeal joints. 6. Describe the anatomical rationale underlying clinical correlations in the text and the clinical correlation section of notes. Be able to describe clinical scenarios including patient presentation, signs/symptoms, mechanism of injury, diagnosis, typical patient profile, and underlying anatomical rationale. Carpal tunnel syndrome Carpal tunnel syndrome is an entrapment syndrome caused by pressure on the median nerve within the carpal tunnel. The etiology of this condition may be a direct effect of increased pressure on the median nerve caused by overuse, swelling of the tendons and tendon sheaths (e.g., rheumatoid arthritis), and cysts arising from the carpal joints. Increased pressure in the carpal tunnel is thought to cause venous congestion that produces nerve edema and anoxic damage to the capillary endothelium of the median nerve itself. Patients typically report pain and pins and needles in the distribution of the median nerve. Weakness and loss of muscle bulk of the thenar muscles may also occur. Gently tapping over the median nerve (in the region of the flexor retinaculum) readily produces these symptoms (Tinel's sign). Initial treatment is aimed at reducing the inflammation and removing any repetitive insults that produce the symptoms. If this does not lead to improvement, nerve conduction studies will be necessary to confirm nerve entrapment, which may require surgical decompression of the flexor retinaculum. Ulnar nerve injury The ulnar nerve is most commonly injured at two sites: the elbow and the wrist. At the elbow, the nerve lies posterior to the medial epicondyle. At the wrist, the ulnar nerve passes superficial to the flexor retinaculum and lies lateral to the pisiform bone. Ulnar nerve lesions are characterized by "clawing" of the hand, in which the metacarpophalangeal joints of the fingers are hyperextended and the interphalangeal joints are flexed because the function of most of the intrinsic muscles of the hand is lost. Clawing is most pronounced in the medial fingers because the function of all intrinsic muscles of these digits is lost while in the lateral two digits, the lumbricals are innervated by the median nerve. Function of the adductor pollicis muscle is also lost. In lesions of the ulnar nerve at the elbow, function of the flexor carpi ulnaris muscle and flexor digitorum profundus to the medial two digits is lost as well. Clawing of the hand, particularly of the little and ring fingers, is worse with lesions of the ulnar nerve at the wrist than at the elbow because interruption of the nerve at the elbow paralyzes the ulnar half of the flexor digitorum profundus, which leads to lack of flexion at the distal interphalangeal joints in these fingers. Ulnar nerve lesions at the elbow and wrist result in impaired sensory innervation on the palmar aspect of the medial one and one-half digits. Radial nerve injury Around the elbow joint the radial nerve divides into its two terminal branches-the superficial branch and the deep branch nerve. The most common radial nerve injury is damage to the nerve in the radial groove of the humerus, which produces a global paralysis of the muscles of the posterior compartment resulting in wrist drop. Radial nerve damage can result from fracture of the shaft of the humerus as the radial nerve spirals around in the radial groove. The typical injury produces reduction of sensation in the cutaneous distribution, predominantly over the posterior aspect of the hand. Severing the posterior interosseous nerve (continuation of deep branch of radial nerve) may paralyze the muscles of the posterior compartment of the forearm, but the nerve supply is variable. Typically, the patient may not be able to extend the fingers. The distal branches of the superficial branch of the radial nerve can be readily palpated as "cords" passing over the tendon of the extensor pollicis longus in the anatomical snuffbox. Damage to these branches is of little consequence because they supply only a small area of skin. Joints of the Upper Limb 1. 2. 3. 4. Identify the type of joint. Identify types of movement allowed. Identify major supportive structures (i.e., ligaments and muscles) Describe internal joint architecture. Joint Type Movement Support Architecture Sternoclavicular (sc) Synovial, saddle-shaped, contains an articular disc Movement of the clavicle in the anteroposterior and vertical planes Ligaments (4): -anterior sternoclavicular ligament -between the proximal end of the clavicle and the clavicular notch of the manubrium -posterior sternoclavicular ligament -part of the 1st costal cartilage -interclavicular ligament -costoclavicular ligament Muscles: -all muscles that attach to the scapula Membrane: -synovial -fibrous Acromioclavicular (ac) Synovial Movement in the anteroposterior and vertical planes, some axial rotation Ligaments (2): -between the acromion and clavicle -acromioclavicular ligament -coracoclavicular ligament (trapezoid ligament and conoid ligament) Membranes: -synovial -fibrous Glenohumeral Synovial, ball and socket Multi-axial, flexion, extension, abduction, adduction, medial rotation, lateral rotation, circumduction Muscles (10): -supraspinatus -infraspinatus -teres minor -subscapularis -long head of the biceps brachii -deltoid -pectoralis major -coracobrachialis -latissimus dorsi -teres major Ligaments (4): -coracoacromial -coracohumeral -between the head of the humerus and the glenoid cavity of the scapula -transverse humeral -glenohumeral (superior, middle, inferior) Membranes: -synovial -fibrous Elbow Synovial -trochlea of humerus Muscles: to trochlear notch of ulna = hinge like -biceps brachii flexion and extension -brachialis -three separate joints, share a cavity -capitulum of humerus to head of radius = hinge like flexion and extension -synovial membrane is separated from the fibrous membrane of the joint capsule by fat pads (in the coronoid fossa, the olecranon fossa, and the medial fossa) -triceps brachii -brachilradialis -anconeus -supinator Ligaments: -annular -radial collateral -ulnar collateral Membranes: -includes the proximal radio-ulnar joint -fibrous membrane (superficial to the synovial membrane), attaches to the medial epicondyle and the margins of the olecranon, coronoid, and radial fossa of the humerus, coronoid process, olecranon of the ulna -synovial -fibrous Proximal radioulnar Synovial pivot Pronation and supination See above -head of radius to radial notch of the ulna, see above Distal radio-ulnar Synovial pivot Pronation and supination Ligaments: -between the head of the ulna and the ulnar notch of the radius -anular Muscles: -biceps brachii -supinator -fibrous articular disc between the joint and wrist -synovial and fibrous membranes -pronator teres -pronator quadratus Membranes: -interosseous -synovial -fibrous Radiocarpal (wrist) Synovial condylar Abduction, adduction, flexion, extension Ligaments: -palmar radiocarpal -palmar ulnocarpal -between the radius/the articular disk and the carpal bones (scaphoid, lunate, and triquetrum) -dorsal radiocarpal -radial collateral ligament of the wrist -ulnar collateral ligament of the wrist Intercarpal Synovial joints Limited movement but contributes to positioning of the had in abduction, adduction, flexion, and extension The gray's book says “numerous ligaments” but did not name them. I found some ligaments in Rohen's atlas but I decided not to include them in this chart. There looks like there are maybe 5-10. Between carpal bones that share a common articular cavity Carpometacarpal Synovial -greater range of motion between metacarpal 1 and trapezium, flexion, extension, abduction, adduction, rotation, and circumduction Again, there is only a small paragraph about this joint in the book and it does not name specific ligaments. If anyone would like to borrow my Rohen's atlas let me know. My understanding is that if it is not in gray's, we don't need to know it. Between metacarpals and carpals Ligaments: Between the distal heads of the metacarpals and the proximal phalanges of the digits -metacarpal 1 and carpal = saddle-shaped -metacarpal 2-5 and carpal = plane -limited sliding motion between metacarpals 2-5 and the carpal bones Metacarpal phalangeal Synovial condylar Flexion, extension, abduction, adduction, circumduction, limited rotation -palmar -collateral ligaments (medial and lateral) -deep transverse metacarpal ligaments Interphalangeal joint Synovial hinge Flexion and extension Ligaments: Between phalanges -collateral ligaments -palmar ligaments Clinical and Surface Anatomy 1. Identify the superficial landmarks associated with the upper limb (features of the skin, superficial and deep fascia, spaces, compartments, boney landmarks, muscles, ligaments, nerves, vasculature and joints). a. Shoulder - palpable spine, acromion, and coracoid process of the scapula. Can also palpate inferior angle and much of medial border. i. Can the palpate the supraspinatus and infraspinatus above and below the spine. ii. Trapezius (medial to U formed by clavicle and acromion) and deltoid (lateral to this U) form the contour of the shoulder. Axillary nerve runs deep to the deltoid around the surgical neck of the humerus. iii. Latissimus dorsi and teres major underly the axillary skin fold. b. Arm – olecranon (boney protuberance at the tip of the elbow), medial and lateral epicondyles. i. Triceps brachii is soft tissue mass posterior to humerus, inserts at olecranon. ii. Ulnar nerve passes posterior to medial epicondyle. iii. Brachioradialis is on the medial aspect of proximal forearm (flex elbow against pressure to view). Radial nerve comes from behind humerus to lie under the brachioradialis. The brachial artery is on the medial side of the arm in the cleft between the biceps brachii and triceps brachii muscles. The median nerve courses with the brachial artery, whereas the ulnar nerve deviates posteriorly from the vessel in distal regions. iv. Cubital fossa lie anterior to the elbow. Borders are lateral to medial epicondyle, brachioradialis and pronator teres muscles. Contains – biceps brachii tendon (lateral), brachial artery, median nerve (medial) (TAN). Can see cephalic, basillic and medial cubital veins in subq fascia. c. Distal forearm – i. Flexor carpi radialis (anterior) – lateral 1/3 of the anterior surface of forearm. Radial artery is immediately lateral and the site of radial pulse. ii. Flexor carpi ulnaris (anterior) – medial margin of forearm, inserts on pisiform. Can follow to palpate pisiform. Ulnar nerve and artery run under lateral lip of flexor carpi ulnaris. iii. Palmaris longus tendon (may be absent) (anterior) – down the center of the anterior surface of the forearm. Median nerve lies under palmaris longus tendon. Long tendon of the hand run deep to the median nerve and between the flexor carpi radialis and ulnaris. iv. Posterior – extensor digitorum tendons radiate to 2nd through 5th digits. Extensor carpi radialis longus and brevis muscles of lateral side of the wrist. Extensor carpi unlaris on medial side of wrist between end of ulna and the wrist. 1. Anatomical snuff box – borders = tendon of extensor pollicis longus (medial) and extensor pollicis brevis and abductor pollicis longus (lateral). Radial artery (radial pulse!), cephalic vein, and radial nerve run through here. d. Hand – thenar eminence, hypothenar eminence, dorsal venous network w/ basilica vein (medial) and cephalic vein (lateral), flexor retinaculum (btwn pisiform and tubercle of the scaphoid, and hypothenar 2. and thenar eminences), recurrent branch of median nerve (under flexor retinaculum to sit on top of thenar eminence), i. Superficial palmar arch - continuation of the ulnar artery, which lies lateral to the pisiform. Curves laterally across the palm anterior to the long flexor tendons in the hand, reaches as high as the proximal transverse skin crease of the palm and terminates laterally by joining branch of the radial artery that crosses the thenar eminence. ii. Deep palmar arch - originates on the lateral side of the palm deep to the long flexor tendons and between the proximal ends of metacarpals I and II, arches medially across the palm, terminates by joining the deep branch of the ulnar artery, which passes through the base of the hypothenar muscles and between the pisiform and hook of the hamate. The deep palmar arch is more proximal in the hand. e. Axillary inlet – anterior margin = clavicle to the coracoid process, inferior margin posterior = axillary skin fold overlying teres major and latissimus dorsi, inferior margin anterior = anterior axillary skin fold overlying pectoralis major, medial wall = serratus anterior, lateral border = humerus, floor of axilla = skin of the armpit. i. Long thoracic nerve passes vertically out of the axilla and down the lateral surface of serratus anterior just anterior to the posterior axillary skin fold. ii. The axillary artery, axillary vein and components of the brachial plexus pass through the axilla and into the arm by traveling lateral to the dome of skin that forms the floor. This neurovascular bundle can be palpated by placing a hand into this dome of skin and pressing laterally against the humerus. iii. Cephalic vein travels btwn deltoid and pectoralis major in clavipectoral triangle, joins the deeper axillary vein. f. Pulse points – axillary pulse, brachial pulse in midarm, brachial pulse in cubital fossa, radial pulse in distal forearm, ulnar pulse in distal forearm, radial pulse in anatomical snuff box. Apply anatomic knowledge and understanding to clinical scenarios presented in the chapter (see green boxes) and clinical correlations sections in notes. a. Fracture of the proximal humerus (p668) – fractures of the surgical neck are most common bc it is a weaker part of the bone. The associated axillary nerve and posterior (and I suppose anterior) circumflex humeral artery can be damaged (but this rarely happens). Test axillary nerve before relocation. b. Fractures of the clavicle and dislocations of theacromioclavicular and sternoclavicular joints (p573) – Clavicle fracture common due to size relative to potential forces, middle 1/3 fractures. Acromial end of clavicle tends to dislocate w/ trauma. Minor injury can tear fibrous joint capsule and ligaments of AC joint resulting in AC separation. More severe trauma and tear conoid and trapezoid ligaments (coracoclavicular ligament) resulting in elevation and upward sublaxation of the clavicle. Injury at SC joint usually anterior or posterior dislocation, posterior dislocation can impinge of great vessels. c. Dislocations of the glenohumeral joint (p674) – anterior (anteroinferior) dislocation is most frequent, and once it occurs and disrupts joint capsule it can occur with less force. Concerns – impinge on axillary nerve, stretch radial nerve. Posterior dislocation uncommon (electrocution, epileptic seizure). d. Rotator cuff disorders (p675) – Impingement and tendinopathy. Supraspinatus is most commonly involved as it passes beneath the acromion and acromioclavicular ligament (fixed dimention). Swelling of muscle, excessive fluid in the subacromial/subdeltoid bursae, or acromial bony spurs cause impingent during abduction. Blood supply to the supraspinatus tendon is poor, repeat trauma = degenerative changes and pain. Can result in partial- or full- thickness tears. Trouble with combing hair (abduction). Common is older patients. e. Inflammation of the subacromial (subdeltoid) bursae (p675) – inflammation (caused by supraspinaus tendinopathy or shoulder injury) makes movements of the glenohumeral joint painful. Inject corticosteroids and local anesthetic. f. Quadrangular space syndrome (p682) – hypertrophy of border muscles or fibrosis of the muscle edge can impinge on the axillary n. results – atrophy of teres minor muscle (typical, and affecting rotator cuff muscle function) and weakness of deltoid (atypical). Damage to the long thoracic nerve (p690) – descends on the lateral thoracic wall, on the external surface of serratus anterior, JUST DEEP TO SKIN AND SUBQ FASCIA, it’s vulnerable! Loss of muscle function allows medial border, esp inferior angle, of the scapula to elevate away from the thoracic wall. Normal elevation of the arm is no longer possible. When a patient pushes forward with the arm they will demonstrate “winging” of the scapula. h. Imaging the blood supply to the upper limb (p698) – use with trauma or insertion of AV fistula for dialysis. Ultrasound (3rd part of subclavian to deep and superficial palmar arteries). Angiography involves catheter insertion in femoral, working to the arm, inject radiopaque contrast. i. Trauma to the arteries of the upper limb (p699) – vulnerable in places where positin is fixed or subq. Fracture of 1st rib – compromise the distal portion of the subclavian a. or first part of axillary artery. Anastomoses are scapula and proximal humerus supply arm. Anterior dislocation of humeral head – compress axillary a. (artery is intimately related to brachial plexus!) j. Subclavian pinch off syndrome (p699) – central venous access routes include subclavian route actually enter 1st part of axillary v.) and jugular route. Subclavian route used for catheterization and placement of long term lines (hickman lines), short-term with multiple catheters, pacemaker wire insertion. How – identify clavicle, place needle in infraclavicular region at the midclavicular line or lateral to it, aim superomedially, aspirate blood. Complications – enter midclavicular or later to avoid other structure. Putting pacemaker wire through subclavius can cause kink and contraction of muscle could break the catherter or pacemaker wire. k. Injury to the brachial plexus (p709) – diagnosis requires meticulous clinical history taking and examination. Nerve conduction studies and electromyography are used to assess latency of muscle contraction when nerve is artificially stimulated. Usually blunt force trauma and devastating to function of the UL. Spinal cord injuries (spinal nerves), direct pulling injuries (roots of brachial plexus), trauma to the first rib (trunks), dislocation of glenohumeral joint (divisions and cords) can all affect brachial plexus. l. Breast cancer (p711) – axillary nodes drain lateral part of the breast. Removal of these nodes or radiotherapy of the axilla (kills small lymphatics as well) damages drainage of UL. Result = swelling, pitting edema (lymphedema) m. Rupture of biceps tendon (p716) – usually long head of biceps brachii. “Popeye sign” – prominent bulge of the muscle belly when flexing the elbow. Usually little effect on UL function. n. Blood pressure measurement (p720) – use sphygmometer and stethoscope. Compress the brachial a. pulse becomes audible just below systolic. Thumping becomes inaudible just belwo diastolic. Normal = 120/80mm Hg. o. Radial nerve injury in the arm (p724) – bounds with profunda brachii artery btwn medial and lateral head of triceps. Midshaft humerus fracture can permanently damage nerve. Symtoms – wrist drop, sensory changes over dorsum of hand. p. Median nerve injury in the arm (p724) – deep position, injury atypical. Most common issue is compression under flexor retinaculum (carpal tunnel syndrome). Rare issue – embryo remnant of corachobrachialis (ligament of struthers) can calcify and compress the median nerve. Symptoms – weakness in flexor muscles of the forearm and thenar muscles. q. Elbow joint injury (p727) – important to know age when interpreting radiographs bc of 2ndary ossification centers, capitulum-1 year; head (of radius)-5 years; medial epicondyle-5 years; trochlea-11 years; olecranon-12 years; lateral epicondyle-13 years. r. Supracondylar fracture of the humerus (p728) – in children, fracture proximal to the epicondyles. Distal piece and soft tissues pulled posteriorly by triceps, pulling on brachial artery (bowstrining). Anterior forearm become ischemic, sig reduced function of anterior compartment of the forearm. s. Trasection of the radial and ulnar arteries (p728) – adults… relatively subq. Typical cause – hand through plate glass window. Can ligate one or the other with little consequence. t. Pulled elbow (p728) – children under 5…pull a kid up a curb. Not-yet developed head of radius, laxity of anular ligament of radius. Painful but once relocated it subsides. Supinate and compress the elbow. g. u. v. w. x. y. z. aa. bb. cc. dd. ee. ff. gg. hh. Fracture of the head of the radius (p728) – typical cause – fall on outstretched hand. Loss of full extension. Surgical reconstruction and physiotherapy. “Fat pad” sign – when fracture the synovial cavity fills with fluid and elevates fat pads from in coronoid and olecranon fossa. Epicondylitis (p728) – golf and tennis. Overuse of flexor and extensor muscles of the forearm. Pain around epicondyles (golf – medial/ flexor tendons, tennis – lateral/ extensor origin), resolves with rest. Surgical division of extensor or flexor origins from bone can relieve pain. Elbow arthritis (p729) – osteoarthritis, common in dominant limb. Degenerative changes = boney spurs = loss of flexion/ extension. Ulnar nerve injury (p729) – posterior to medial epicondyle of the humerus in cubital tunnel, tunnel can undergo degenerative changes in older patients, compress nerve during flexion. Also direct trauma can cause impaired function. Construction of dialysis fistula (p731) – dialysis requires considerable flow rates, so requires vessels with high flow but veins in UL don’t have such high flow so the radial a. is joined to cephalic v. at the wrist or brachial a. to cephalic v. at elbow. Veins will increase in size in response to increased flow. Fractures of the radius and ulna (p734) – behave as one bone, serious injury usually affects both (fracture of both, fracture of one and dislocation of the other). See fracture, x-ray joints to check from dislocation. 3 classic injuries – i. monteggia’s fracture – fracture of prox 1/3 of ulna, anterior dislocation of radius at elbow. ii. galeazzi’s fracture – fracture of distal 1/3 of radius, partial dislocation of ulna at wrist iii. colle’s fracture – fracture and posterior displacement of distal radius fracture of the scaphois and avascular necrosis of the proximal scaphoid (p756) – most common carpal fracture – across the waist of the scaphoid. 10% of people – scaphoid sole blood supply from radial a. entering distal bone. In fracture proximal part loses blood supply and undergoes avascular necrosis. Carpal tunnel syndrome (p758) – entrapment of median nerve in carpal tunnel. Possible causes – overuse, swelling of tendons and sheaths, cysts in carpal joints. Increased pressure in carpal tunnel also causes venous congention resulting in edema and anoxic change. Symptoms – pain and pins and needles, weakness/ loss of function of thenar muscles. Test – tap medial nerve in tunnel produces symptoms tinel’s sign. Treatment – reduce inflammation, remove repetitive insults, surgical decompression. Snuffbox (p759) – in ulnar deviation the scaphoid is palpable, access fracture. Radial pulse felt here. Allen’s test (p770) – test adequate anatomosomes btwn radial and ulnar arteries. Compress radial and ulnar arteries in wrist, release pressure from one, observe filling pattern. Little connection in palmar arches demonstrates as red thumb and lateral index finger when radial artery is released. Venipuncture (p770) – ideal locations – cubital fossa and cephalic vein adjacent to snuffbox. Ulnar nerve injury (p772) – elbow posterior to medial epicondyle, wrist superficial to flexor retinaculum and lateral to pisiform. Symptoms – clawing of the hand (most pronounced in medial fingers), elbow injury results in loss of flexor carpi ulnaris and flexor digitorum profundus, impaired sensory innervation on palmar aspect of medial 1.5 digits. Distal branch of the ulnar nerve can help determine where the injury is, branches in distal forearm to innervate the medial side of dorsal hand. Radial nerve injury (p774) – most common injury site at radial groove of humerus (due to fracture) resulting in global paralysis of posterior compartment muscles = wrist drop, reduced sensation in post aspect of the hand. Splits into superficial and deep branches at elbow… i. Severing the posterior interosseous nerve (continuation of deep branch of radial nerve) may paralyze the muscles of the posterior compartment of the forearm, but the nerve supply is variable. Typically, the patient may not be able to extend the fingers. ii. The distal branches of the superficial branch of the radial nerve can be readily palpated as "cords" passing over the tendon of the extensor pollicis longus in the anatomical snuffbox. Damage to these branches is of little consequence because they supply only a small area of skin. Shoulder problem after falling on an outstretched hand (p786) – initially minor tenderness after fall, at presentation has pain and weakness in rt shoulder with muscle wasting of supraspinatus and infraspinatus (disuse), initiation of abduction is difficult, weak lateral rotation of humerus. The patient's apparent minor injury damaged the fibrocartilaginous glenoid labrum, which allowed a cyst to form and pass along the anterosuperior border of the scapula to enter the spinoglenoid notch. The cyst then extended upward, so compressing the suprascapular nerve. Surgical excision of the damaged glenoid labrum and removal improved the patient's symptoms. ii. Winged scapula (p786) – rt mastectomy, removal of axillary process and nodes for treatment of breast cancer. Nerve to serratus anterior (long thoracic nerve) was damaged causing loss of muscle mass and elevation of inferior angle away from costal surface. jj. Brachial plexus nerve block (p787) – 10ml local anesthetic into the axillary sheath. Palpate axillary artery with arm abducted and laterally rotated, locate the axillary sheath, inject anesthetic on both sides of axillary a. complications – direct needle spike of brachial plexus branches damaged axillary artery, arterial injection of the anesthetic. kk. Complication of a fractured 1st rib (p787) – car accident, unconscious, x-ray reveals fracture 1st rib. Check reflexes and axillary a., brachial a., radial a., and ulnar a. pulses. Requires considerable force to break the 1st rib. ll. Carpal tunnel syndrome? (p788) - tingling and numbness in 1st-3rd digits, anesthesia at base of thenar eminence, worse with arm extension. Median nerve compression but not carpal tunnel (cutaneous branch of median nerve supplying base of thenar eminence is proximal to carpal tunnel). Nerve studies indicated increased latency below the elbow. Issue was ligament of struthers (embryo remnant of corachobrachialis, extremely rare finding). mm. Immobilizing extensor digitorum (p789) - Placing the fist in a palm-down position on the table and pressing the middle phalanges onto the table effectively immobilizes the action of the extensor digitorum. Cannot lift middle finger in this position. Not true of the index and little fingers. nn. Torn supraspinatus tendon (p789) – rt shoulder pain, failure to initiate abduction, wasting of supraspinatus. Issue was tear in supraspinatus tendon (only supraspinatus affected here so tendon seems likely). Surgical repair needed. oo. How to examine the hand (p790) – examine the following i. Musculoskeletal system – looking for abnormailities, muscle wasting, palpate ind bones, joints (for restriction), muscle contraction ii. Circulation – radial and ulnar pulses and capillary return. iii. Nerves - A very simple examination would include tests for the median nerve by opposition of the thumb, for the ulnar nerve by abduction and adduction of the digits, and for the radial nerve by extension of the wrist and fingers and feeling on the back of the first web space. 1. Median - Median nerve damage results in wasting of the thenar eminence, absence of abduction of the thumb, and absence of opposition of the thumb. 2. Ulnar nerve - An ulnar nerve palsy results in wasting of the hypothenar eminence, absent flexion of the distal interphalangeal joints of the little and ring fingers, and absent abduction and adduction of the fingers. The thumb is unaffected. 3. Radial nerve - The radial nerve also produces extension of the wrist and extension of the metacarpophalangeal and interphalangeal joints and of the digits. pp. Shoulder joint problems (p791) – recurrent shoulder dislocation. MRI. Torn loose or born loose. Patient had a piece of bone that had fractured from posterior superior aspect of humeral head and separation of glenoid labrum (the bankart lesion). Underwent arthroscopic repair capsule tightened labrum and bony fragment sutured in place. i. Arthroscopy - Arthroscopy of the shoulder is an established method for assessing the shoulder joint. Portals of entry are anterior and posterior and small holes in the capsule are made percutaneously. The shoulder joint is filled with saline, which distends it, allowing the arthroscope to move around the joint and inspect the joint surfaces, including the labrum.