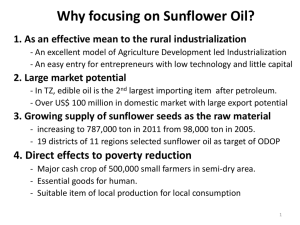
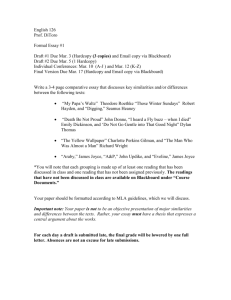
A tool for generating evidence to inform policies
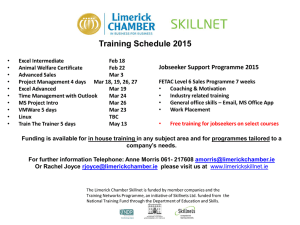
advertisement

Medicines safety in WHO: promoting best practices in Pharmacovigilance Dr Shanthi Pal Quality and Safety of Medicines WHO TBS_MAR_ 2011 1 What is pharmacovigilance The science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug-related problems. (The Importance of Pharmacovigilance, WHO 2002) A tool for generating evidence to inform policies 2 TBS_MAR_ 2011 2 Birth of modern pharmacovigilance Thalidomide – Phocomelia 1961 TBS_MAR_ 2011 3 16th World Health Assembly 1963 Assembly Resolution 16.36 - Clinical and Pharmacological Evaluation of Drugs INVITES Member States to arrange for a systematic collection of information on serious adverse drug reactions observed during the development of a drug and, in particular, after its release for general use. TBS_MAR_ 2011 4 WHO Programme for 140 International National Drug Monitoring Centres WHO Collaborating Centre, Uppsala WHO WHO Collaborating Centre, Ghana WHO Collaborating Centre, Morocco TBS_MAR_ 2011 5 Roles and Responsibilities WHO Policies and strategies for PV Guidelines, norms and standards Exchange of information Systems strengthening Training and capacity building Dialogue with donors & public health programmes TBS_MAR_ 2011 WHO Collaborating Centres Tools and technologies Research and Innovation Implementation / proof of concept Everyday technical support Training and capacity building Exchange of information 6 Policies (WHO) Implementation WHO WHO CCs ADR Data Country Analysis Signals Communication Based on spontaneous reporting Database TBS_MAR_ 2011 7 Advisory Committee on Safety of Medicinal Products (ACSoMP) The Advisory Committee on Safety of Medicinal Products shall provide advice on pharmacovigilance policy and issues related to the safety and effectiveness of medicinal products to the relevant Assistant Director-General in WHO and through him / her to the Collaborating Centre for International Drug Monitoring (the Uppsala Monitoring Centre), and to the Member States of WHO. TBS_MAR_ 2011 9 The WHO PV strategy What defines it TBS_MAR_ 2011 10 Putting the horse in front of the cart AFRICA If there are no systems, there will be no evidence TBS_MAR_ 2011 11 Morbidity profile (Clinical case mix) Distinct from developed countries Infectious diseases – 90% of global burden Determines the pharmaceutical characteristics Determines the Adverse event profile TBS_MAR_ 2011 12 Characteristics of the Pharmaceutical Setting Inefficient pharmaceutical procurement; inadequate storage facilities and distribution practices Few functional reputable or local pharmaceutical companies Lax border controls and customs entry points Weak regulatory systems TBS_MAR_ 2011 13 TBS_MAR_ 2011 14 TBS_MAR_ 2011 15 Diethylene glycol tragedy in Nigeria NAFDAC Nigeria Paracetamol 1989 > 100 deaths (children) Paracetamol + Chlorpheniramine 2009 (teething mixture – ‘My Pikin’) ~100 deaths (children) ~110 Acute renal failure PV scope needs to be expanded to address quality issues TBS_MAR_ 2011 16 Up to 50% of ADRs are preventable TBS_MAR_ 2011 17 Pharmacovigilance system that Records errors Analyses Learns Implements checks Prevents errors TBS_MAR_ 2011 18 Spontaneous reporting: Bedrock of PV these forty years. But: Lack of denominator data Public health programmes need to address key safety questions, quickly provide rates of AEs monitor AEs in special populations (children..) TBS_MAR_ 2011 19 Addressing the PV needs of public health programmes Dystonia with ACTs ? Result of malnutrition / repeated treatment with ACTs? Malaria HIV/AIDS Delete d4t?; NVP in women? Can we use TDF without renal monitoring? Risk of severe anaemia in children with AZT? Use NVP & rifampicin concomitantly in HIV/TB patients? TBS_MAR_ 2011 20 Methodological development Additional data sources Cohort Event Monitoring recording patients exposed (cohort, target 10 000) active and systematic follow-up for adverse events provides incidence rates and risk profile identification of sub-groups at risk piloted in Tanzania and Nigeria for malaria treatment supported by CemFlow ™ management tool TBS_MAR_ 2011 21 WHO has developed a protocol for cohort event monitoring (CEM) of antimalarials and ARVs is implementing CEM of antimalarials in Africa has developed 'Pregnancy register' protocol TBS_MAR_ 2011 22 Understanding what's available and what's needed in countries TBS_MAR_ 2011 23 Challenges to Pharmacovigilance TBS_MAR_ 2011 24 Type of assistance needed TBS_MAR_ 2011 25 PV consultants for AFRICA: PVSF WHO CC for advocacy and training in PV, Accra, Ghana TBS_MAR_ 2011 26 Technical Solutions for Africa VigiFlow: tool for national ICSR management and submission to WHO/UMC Provides country with a national database E2b compliant Incorporates MEDRA Free software update and maintenance by UMC Challenge: access to broadband internet Solution: Silverlite TBS_MAR_ 2011 27 Joint WHO/Global Fund pharmacovigilance strategy Establish basic functions and minimum requirements of national pharmacovigilance system Min PV req pharmacovigilance toolkit to support training and development www.pvafrica.org/toolkit Strong wording in Round 10 requesting countries to include PV TBS_MAR_ 2011 28 http://www.who.int/medicines/areas/quality_safety/ safety_efficacy/saf_pub/en/ TBS_MAR_ 2011 29 TBS_MAR_ 2011 30 What gets measured, gets done Success indicators Outcomes Impact TBS_MAR_ 2011 31 Additional stakeholders: the full picture Direct patient reporting WHO guidelines TBS_MAR_ 2011 32 Our strategy Understanding the local needs Making a 'deal' with public health programmes Bringing in additional stakeholders Expanding the scope of PV More patient centred TBS_MAR_ 2011 34 A systems approach We need to install systems and structures in place To promote PV as 'best practice' That aim to improve quality of care While addressing the safety, effectiveness and quality of medicines TBS_MAR_ 2011 35 Maintain as the cheapest, easiest, most sustainable method 3 tiers-approach for WHO 1. As before (Spontaneous reporting) Methods, additional use (errors, quality issues, resistance), more 2. More than before centres, patient focused Tools Handbooks New partners, Pilot 3. As never before Public Measure, Resources Indicators Fundraising (EuropeAid; BMGF; FP7) Networks of excellence (PVSF) TBS_MAR_ 2011 36 Thank you The impossible: we are on it For miracles: expect some delay Website www.who.int/medicines/areas/quality_safety/safety_efficacy/en TBS_MAR_ 2011 37