Complications of Urinary Diversion
advertisement

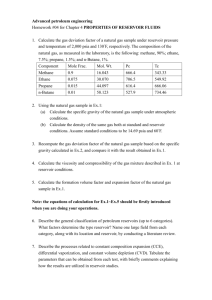
Complications of Urinary Diversion By Peter Tran, D.O. Garden City Hospital Resident Talk 12/17/2008 Overview Classification of urinary diversions Factors influencing complications Complications according to bowel segments Metabolic/physiologic complications Surgical complications: early and late Clasification of Diversions Orthotopic Heterotopic ◦ Continent cutaneous ◦ Non-continent cutaneous ◦ Diversion to GIT Examples of Orthotopic Neobladders Figure 82-2 Construction of the modified Camey II. A, The ileal loop is folded three times (Z shaped) and incised on the antimesenteric border. B, The reservoir is closed with a running suture to approximate the incised ileum. C, The urethroenteric anastomosis is performed. Examples of Orthotopic Neobladders Figure 82-3 Construction of the Hautmann ileal neobladder. A, A 70-cm portion of terminal ileum is selected. Note that the isolated segment of ileum is incised on the antimesenteric border. B, The ileum is arranged into an M or W configuration with the four limbs sutured to one another. C, After a buttonhole of ileum is removed on an antimesenteric portion of the ileum, the urethroenteric anastomosis is performed. The ureteral implants (Le Duc) are performed and stented, and the reservoir is then closed in a side-to-side manner. Examples of Orthotopic Neobladders Figure 82-4 Construction of the ileal neobladder (Studer pouch) with an isoperistaltic afferent ileal limb. A, A 60- to 65-cm distal ileal segment is isolated (approximately 25 cm proximal to the ileocecal valve) and folded into a U configuration. Note that the distal 40 cm of ileum constitutes the U shape and is opened on the antimesenteric border; the more proximal 20 to 25 cm of ileum remains intact (afferent limb). B, The posterior plate of the reservoir is formed by joining the medial borders of the limbs with a continuous running suture. The ureteroileal anastomoses are performed in a standard end-to-side technique to the proximal portion (afferent limb) of the ileum. Ureteral stents are used and brought out anteriorly through separate stab wounds. C, The reservoir is folded and oversewn (anterior wall). D, Before complete closure, a buttonhole opening is made in the most dependent (caudal) portion of the reservoir. E, The urethroenteric anastomosis is performed. F, A cystostomy tube is placed, and the reservoir is closed completely. Examples of Orthotopic Neobladders Figure 82-5 Construction of the Kock ileal reservoir. A, A total of 61 cm of terminal ileum is isolated. Two 22-cm segments are placed in a U configuration and opened adjacent to the mesentery. Note that the more proximal 17-cm segment of ileum will be used to make the afferent intussuscepted nipple valve. B, The posterior wall of the reservoir is then formed by joining the medial portions of the U with a continuous running suture. C, A 5- to 7-cm antireflux valve is made by intussusception of the afferent limb with the use of Allis forceps clamps. D, The afferent limb is fixed with two rows of staples placed within the leaves of the valve. E, The valve is fixed to the back wall from outside the reservoir. F, After completion of the afferent limb, the reservoir is completed by folding the ileum on itself and closing it (anterior wall). Note that the most dependent portion of the reservoir becomes the neourethra. The ureteroileal anastomosis is performed first, and the urethroenteric anastomosis is completed in a tension-free, mucosa-to-mucosa fashion. Examples of Orthotopic Neobladders Figure 82-8 Construction of the Mainz ileocolonic orthotopic reservoir. A, An isolated 10 to 15 cm of cecum in continuity with 20 to 30 cm of ileum is isolated. B, The entire bowel segment is opened along the antimesenteric border. Note that an appendectomy is performed. C, The posterior plate of the reservoir is constructed by joining the opposing three limbs together with a continuous running suture. D, An antireflux implantation of the ureters through a sub-mucosal tunnel is performed and stented. E, A buttonhole incision in the dependent portion of the cecum is made that provides for the urethroenteric anastomosis. Note that the ureterocolonic anastomoses are performed before closure of the reservoir. F, The reservoir is closed side to side with a cystostomy tube and the stents exiting. Examples of Orthotopic Neobladders Figure 82-9 Construction of Le Bag (ileocolonic) orthotopic reservoir. A, A total of 20 cm of ascending cecum and colon, with a corresponding length of adjacent terminal ileum, is isolated. The bowel is opened along the entire antimesenteric border, and the two incised segments are then sewn to one another. This forms the posterior plate of the reservoir. B, This reservoir is folded and rotated 180 degrees into the pelvis with the most proximal portion of the ileum (2 cm nondetubularized) anastomosed to the urethra. C, Modification is performed with complete detubularization of the bowel segment, which is then anastomosed to the urethra. Examples of Heterotopic Cutaneous Diversion Continent/catherizable Pouch ◦ Indiana Pouch Segment of ascending colon with terminal ileum and IC valve as continence mechanism. ◦ Penn Pouch Same as Indiana pouch except appendix used based on Mitrofanoff principle in which continence mechanism is the appendix. ◦ Gastric Pouch Segment of stomach and ileum recreated in to a reservoir Non-Continent ◦ Most popular - ileal loop Excretion of urine by means of evacuation ◦ Ureterosigmoidostomy ◦ Rectal bladder ◦ Sigmoid hemi-Kock Factors Influencing Complications Patient factors Bowel factors Patient Factors Performance status/co-morbidities Pt/caregiver compliance with CIC Mobility Previous XRT Renal function Liver function Body habitus BMI Bowel Factors/Technical Factors Type of intestinal segment used Length of intestinal segment Continent vs. incontinent Method/extend of detubularization Capacity Compliance Refluxing/non-refluxing uretero-enteric anastomosis Type of diversion chosen Gastric Complications Hypochloremic, hypokalemic metabolic alkalosis Hyper-gastrinemia Hematuria-dysuria syndrome Jejunum Complications Most severe metabolic complications Hyponatremia Hyperkalemic, hypochloremic metabolic acidosis Severe dehydration Ileal Complications Hyperchloremic, hypokalemic metabolic acidosis Vit B12 deficiency Colonic Complications Hyperchloremic, hypokalemic metabolic acidosis Metabolic/Physiologic Complications Renal deterioration Electrolyte disturbance Hypertension Altered sensorium Abnormal drug metabolism Osteomalacia Abnormal growth/development Vit deficiency Anemia Chronic diarrhea Hyper-gastrinemia Electrolyte Disturbance Colon/Ileum ◦ Hyperchloremic, hypokalemic metabolic acidosis Stomach ◦ Hypochloremic, hypokalemic metabolic alkalosis Jejunum ◦ Hyperchloremic, hyperkalemic, hyponatremic metabolic acidosis Hyperammonemia Hypomagnesemia Hypocalcemia Colon and Ileum Hyperchloremic, hypokalemic metabolic acidosis ◦ 15% of ileal conduits 10% severe enough to require Tx ◦ 20% of colon conduits 15% require Tx ◦ 50% ileal or colonic pouches 40% require Tx ◦ 80% of ureterosigmoidostomy Hyperchloremic, hypokalemic metabolic acidosis Symptoms ◦ ◦ ◦ ◦ ◦ Easy fatigability Anorexia/weight loss Polydipsia Lethargy Exacerbation of diarrhea in GI diversions Hyperchloremic, hypokalemic metabolic acidosis: MOA Net absorption of ammonium + chloride Increased secretion of HCO3 Impaired distal tubular secretion of hydrogen Physiologic Response ◦ Increased acid secretion by kidneys ◦ Bone demineralization to buffer acidosis Hyperchloremic, hypokalemic metabolic acidosis: Treatment Alkalinizing agent ◦ NaHCO3 ◦ K-Citrate ◦ Na-Citrate Blockers of Cl transport ◦ Chlorpromazine ◦ Nicotinic acid Gastric Complications Hypochloremic, hypokalemic metabolic alkalosis ◦ Rare unless comcomitant renal failure ◦ Severe dehydration, often triggered by vomiting or GI illness ◦ High serum gastrin levels Overdistension of gastric segment triggers gastrin release Gastric Complications Symptoms ◦ ◦ ◦ ◦ ◦ Lethargy Weakness Respiratory insufficiency Seizures Ventricular arrhythmia Gastric Complications: MOA H+, K+, and Cl- loss in gastric segment Net addition of HCO3 Serum gastrin levels correlate with systemic HCO3 concentration Gastric Complications: Tx Acute severe metabolic alkalosis ◦ ◦ ◦ ◦ ◦ ◦ Empty bladder NaCl volume replacement H2 blocker PPI Arginine HCl Surgical removal of gastric segment Gastric Complications: Tx Mild/prophylaxis ◦ Oral Na/K supplementation ◦ H2 blockers Hypokalemia - Incidence Colonic diversions ◦ 30% reduction in total body K Ileal diversions ◦ 0-15% reduction Hypokalemia: MOA Colonic/Ileal diversions ◦ Ileum may passively reabsorb some K blunting the loss ◦ Chronic metabolic acidosis ◦ Renal K wasting Hypokalemia Symptoms ◦ Typically no symptoms ◦ At most severe Muscle weakness Paralysis Hypokalemia: Tx Correct the acidosis ◦ Beware of acutely worsening K as in moves backto intracellular stores ◦ Oral K supplementation Altered Sensorium: MOA Hypomagnesemia Drug reabsorption Ammonia encephalopathy Altered Sensorium: Hypomagnesemia Renal loss Chronic diarrhea Decreased absorption Altered Sensorium: Hypomagnesemia Symptoms ◦ ◦ ◦ ◦ Cardiac arrhythmias Tremor Tetany Seizures Treament ◦ Mg replacement Ammoniogenic Encephalopathy Ammonium secreted by the kidney Ammonia is produced by urease splitting bacteria Reabsorbed and transferred to liver by portal circulation Nomally liver copes and coverts ammonia to urea Ammoniogenic Encephalopathy Risk Factors ◦ Typically in pre-existing or acquired liver disease ◦ Ureterosigmoidostomy>Colon or ileal conduits ◦ Triggers in setting of liver disease Constipation Increased protein load GI bleed UTI with ammonia producer Co-existing CNS depressant use Renal failure ◦ Normal liver ◦ Bacterial endotoxin – liver dysfunction with normal LFT Ammoniogenic Encephalopathy: Symptoms Apathy Restlessness Sleep disturbance Impaired intellectual abililites Asterixis and lethargy Stupor Coma Ammoniogenic Encephalopathy: Tx Decrease nitrogen load/remove precipitants ◦ Drain urine diversion ◦ Limit dietary protein intake ◦ Treat any systemic or UTI ◦ Lactulose Lowers gut pH so more NH4 than NH3 Promotes non-urease producing bacteria Decreases transit time of fecal matter Complexes the ammonia ◦ Neomycin/tetracycline Eliminate ammonia producing bacteria from the GIT ◦ Arginine glutamate Complexes ammonia Abnormal Drug Metabolism Drugs absorbs in GIT Drugs excreted unchanged in urine Reabsorbed in intestinal segment Abnormal Drug Metabolism List of drugs ◦ Dilantin ◦ Methotrexate/chemo ◦ Theophylline ◦ Abx (beta-lactams, nitrofurantoin, aminoglycosides) ChemoTx ◦ Ensure pt well hydrated ◦ Drain diversion with catheter ◦ Consider leukovorin administration with methotrexate Osteomalacia Potential long-term complication Affects children and adults Bone demineralization Mineralized component of bone is replace with osteoid Osteomalacia Risk Factors ◦ Bowel segment used Ureterosig most commonly Colon or ileal cystoplasties Colon or ileal conduits/neobladders ◦ Renal failure Chronic untreated metabolic acidosis Osteomalacia: MOA Bone buffering of chronic metabolic acidosis Vit D resistance – less Ca absorption by GIT Vit D deficiency – acidosis limits vit D production Sulphate in urine inhibits Ca and Mg re-absorption Resitance to PTH ◦ = Ca loss Osteomalacia Symptoms ◦ ◦ ◦ ◦ ◦ Diffuse skeletal pain Bone tenderness Fractures Gait disturbance Proximal muscle weakness Osteomalacia Prevention ◦ Particularly important in postmenopausal women and children ◦ Tx underlying metabolic acidosis Vit C Vit D Activated Vit D metabolite ◦ 1-alpha-hydroxycholecalciferol ◦ Ca supplementation Vitamin Deficiency ADEK – fat soluble lost in malabsorption of fat Vit B12 – absorbed in distal ileum Vitamin B12 Deficiency: Etiology Not synthesized by mammals – only dietary source B12 released from food by enzymes in stomach Bound to IF in duodenum Absorbed in terminal ileum Stored mainly in liver Total body stores of 2-5mg, loss of 0.1% daily Takes 2-4 years for defeciency to take effect 3-20% incidence after terminal ileum resection Vitamin B12 Deficiency: Symptoms Neurologic ◦ Peripheral neuropathy ◦ Degenerative changes/demyelination in spinal cord ◦ Voiding dysfunction ◦ Optic neuropathy Hematologic ◦ Megaloblastic anemia Inflammation of tongue/mouth Psychiatric disturbances Vitamin B12 Deficiency: Labs MCV > 120 Often neutropenia and thrombocytopenia Hypersegmented neutrophils Low serum B12 levels Vitamin B12 Deficiency: Bowel Segment Continent diversion increased risk ◦ Larger bowel segment used ◦ TI/IC junction resection ◦ Resection of > 50cm appears to be a major risk factor Vitamin B12 Deficiency: Tx Prevention ◦ Replace with 100ug cobalamin IM monthly starting 1 year after surgery if > 50cm ileum resected Treatment ◦ Neurologic symptoms may precede other ◦ Treat if the least bit concered ◦ Treat if lab values are abnormal but asymptomatic Surgical Complications Early ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Wound infection Intra-abdominal abscess Pyelonephritis Hemorrhage Urine leak/fistula Bowel leak/fistula Ileus Bowel obstruction Stomal bleeding/necrosis Surgical Complications Late ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Wound hernia or dehiscence Bowel obstruction Ureteral stricture UTI/pyelo Urinary stones Renal deterioration Stomal stenosis/parastomal hernia Hematuria dysuria syndrome Stomal Complications Early ◦ Bleeding ◦ Necrosis Late ◦ ◦ ◦ ◦ ◦ Dermatitis Retraction Prolapse Parastomal hernia Stenosis Stomal Bleeding Early ◦ Conservative Tx ◦ Most will stop with pressure/time Late ◦ ◦ ◦ ◦ Liver disease due to dilated veins Correct coagulopathy Ligation Porto-systemic shunting Parastomal Hernia Incidence ◦ 10% ileal conduit ◦ 20% colon conduit Risk Factors ◦ ◦ ◦ ◦ ◦ ◦ ◦ Wound infection Steriod use Malnutrition Obesity Chronic cough/COPD Advanced age Stomal not brought out through rectus muscle Stomal Stenosis Incidence ◦ 3-25% of ileal conduits ◦ 10-20% of colon conduits ◦ Catherizable stoma – 50% Brooke > Turnbull loop Stomal Stenosis Risk Factors ◦ Catherizable > end > loop ◦ Technical Protruding better and flushed for non-continent Insufficient fascial opening ◦ ◦ ◦ ◦ ◦ Muscle spasm Ischemia Infection Poor stomal hygiene Poor fitting appliance Stomal Stenosis Symptoms ◦ Suspect in Metabolic disturbance Infection/pyelo/sepsis Stones Renal decline Stomal Stenosis Work-up ◦ Conduit residual urine ◦ Loopogram Elongation Reflux with upper tract dilation Segment stenosis Tx ◦ Requires surgical repair Ureteroenteric Stricture Risk Factors ◦ Technical Tension Stripping ureteric blood supply Insufficient window through colon mesentery No mucosal to mucosal apposition ◦ Infection ◦ Stone passage ◦ Radiation ◦ IBD ◦ Previous urine leak Ureteroenteric Stricture Symptom ◦ Stones ◦ Back pain ◦ Infection/sepsis DDx ◦ Ureteral stone ◦ TCC recurrence Ureteroenteric Stricture Imaging US Loopogram CT/IVP Renogram Antegrade Nephrostogram ◦ Most useful ◦ Diagnostic/therapeutic ◦ Tract for antegrade procedure Ureteroenteric Stricture Tx ◦ Endoscopic Antegrade vs retrograde Balloon dilation Cold knife Laser incision ◦ Open Ureteroenteric Stricture Advantages of Endoscopic ◦ ◦ ◦ ◦ ◦ ◦ Reasonable 1st line Tx Less morbidity Less OR time Less blood loss Shorter hospital stay Pt. with metastatic disease Disadvantages ◦ High failure rate ◦ May complicate open repair Ureteroenteric Stricture Factors associated with failure of endoscopic repair ◦ Length > 1cm ◦ Stricture presenting < 6 months since surgery ◦ Left sided stricture Ureteroenteric Anastomosis Ureteroenteric Stricture Procedure Stricture Colon Leadbetter-Clarke 14% Strickler 14% Pagano 7% Small Bowel Bricker 7% Wallace 3% Nipple 8% Le Duc 18%