Creating Relationships and Opportunities: BSM Private Practices
advertisement

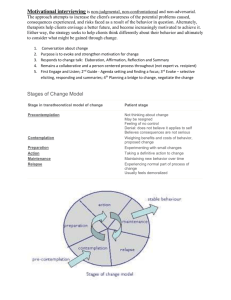
Psychological Implications of Diabetes & Chronic Disease Anne Bartolucci, Ph.D., C.B.S.M. Atlanta Insomnia & Behavioral Health Services, P.C. Disclosures: • No commercial bias or influence • Sources: ▫ ▫ ▫ ▫ Textbooks Articles from peer-reviewed journals Dr. Google (N.I.H. & reputable sources) My own clinical practice • Only one diabetic family member: My Diabetic Family Member: Objectives: • Identify and be able to problem-solve barriers to self-management of diabetes in children and adults both immediately after diagnosis and long-term. • Increase awareness of clinical and subclinical psychological disorders that can arise from diabetes and other chronic conditions. • Introduce time-limited techniques to identify psychological problems and increase compliance with treatment. Biopsychosocial Model • Engel (1977) • Multifactorial • Patient context: “conditions of life and living” ▫ History/Early experiences ▫ Biomedical markers vs. symptom onset & adoption of sick role ▫ Social & cultural context • Trust in physician & medical system ▫ When to seek care ▫ Compliance Biopsychosocial Model • Biological ▫ Physiological ▫ Symptoms • Psychosocial ▫ Cognitive ▫ Social support ▫ Identity as patient • Medico-Legal ▫ Insurance ▫ Coordination of care (e.g., PCP & specialists) Objective: • Identify and be able to problem-solve barriers to self-management of diabetes in children and adults both immediately after diagnosis and long-term. Barriers • Illness affects many areas of a patient’s life • Psychological: ▫ ▫ ▫ ▫ Knowledge Perception bias/accuracy Stress Self-efficacy Barriers: • Psychological (cont’d): ▫ Grief/Adjustment Time Stages: Denial Anger/Shame Bargaining Sadness Acceptance ▫ Actions lack immediate reinforcement Barriers: • Social: ▫ ▫ ▫ ▫ Family environment (children & adolescents) Context of social support Negative social influences Self-care autonomy / Desire for independence Barriers: Problem-Solving • Knowledge: ▫ Patient-centered ▫ Revisit • Training ▫ Hypoglycemia prevention ▫ Self-monitoring • Stress management • Family intervention • Social/Coping skills training Barriers: Problem-Solving • Social: ▫ ▫ ▫ ▫ Include family members in treatment planning Use as coparticipants or coaches Communication Training of school personnel (e.g., teachers, school nurse) Objective: • Increase awareness of clinical and subclinical psychological disorders that can arise from diabetes and other chronic conditions. Psychological Disorders • Depression: ▫ At least three times more prevalent in diabetics than general population ▫ Bilateral influence ▫ Associated with other psychosocial stressors ▫ Challenges: nonspecific effects of illness vs. depression related to diabetes? Psychological Disorders • Eating Disorders ▫ ▫ ▫ ▫ Poorly studied, prevalence unknown Young women Diabetes occurs first Signs: Severe emaciation Poor glycemic control without reason Psychological Disorders • Generalized Anxiety Disorder • Specific Phobia • In children: ▫ Aggression ▫ Learning disabilities • Subclinical ▫ Poor coping with stress ▫ Sleep problems Objectives: • Introduce time-limited techniques to identify psychological problems and increase compliance with treatment. Assessment: Depression • Formal/Structured: ▫ Beck Depression Inventory ▫ SIGECAPS: Sadness Loss of interest Feelings of guilt or being punished Low energy Concentration problems Appetite changes Psychomotor agitation/retardation (observed) Sleep problems Suicidal or homicidal ideation, intent, plan Assessment: Stress • Multifactorial: ▫ Situational stressors ▫ Interpretations/reactions Cognitive Emotional Behavioral ▫ Coping skills ▫ Resources ▫ Self-efficacy Transtheoretical Model • Stages of Change: Where is the patient? ▫ ▫ ▫ ▫ ▫ ▫ Precontemplation Contemplation Preparation Action Maintenance Termination Transtheoretical Model • Processes of change: ▫ ▫ ▫ ▫ ▫ ▫ ▫ ▫ ▫ ▫ Consciousness raising Dramatic relief Self-reevaluation Environmental re-evaluation Self-liberation Social liberation Counterconditioning Stimulus control Contingency management Helping relationships Transtheoretical Model • Most patients will be in contemplation and precontemplation • To move forward… ▫ Precontemplation: increase pros ▫ Contemplation: decrease cons • Pros need to increase twice as much as cons decrease Transtheoretical Model • To move from precontemplation to contemplation, need to engage in: ▫ Consciousness raising ▫ Dramatic relief ▫ Environmental reevaluation • To move forward from contemplation, need: ▫ Self reevaluation • In preparation, person is engaging in: ▫ Self-liberation Compliance: Making Allies • Don’t “should” on your patients! ▫ What can/will they do? ▫ Some compliance is better than none • How do we make this work for you? • What gets in the way of adherence? ▫ Instead of “why aren’t you…?” ▫ Takes defensiveness away • Specific action plan • Revisit what will get in the way? • Building on small & large victories Motivational Interviewing • Identify problem • Resolve ambivalence • Listen for “change talk:” ▫ ▫ ▫ ▫ Problem recognition Expression of concern Intention to change Optimism about change Motivational Interviewing • “Roll with resistance.” ▫ ▫ ▫ ▫ ▫ ▫ ▫ Simple reflection Amplified reflection Double-sided reflection Shifting focus Agreement with a twist Emphasizing personal choice Reframing Maintaining Change: • Lapses vs. Relapses vs. Collapses ▫ Lapse = temporary slip-up ▫ Relapses = larger slip-up ▫ Collapse = back to square one and a half • What can we learn from this? ▫ Tracing sequence of events back to emotional, situational, & behavioral antecedents • What can you do differently next time? Conclusions: • Diabetes is a disorder that affects many aspects of a patient’s life and therefore requires a multifactorial treatment strategy. • The Biopsychosocial Model can help with patient case conceptualization, identification of barriers to compliance, and potential motivators to move through the Stages of Change. • Motivational Interviewing techniques can aid clinicians with moving through resistance to compliance both early in the process and later when the patients slip up. Contact • anne@sleepyintheatl.com • www.sleepyintheatl.com • Office address: ▫ 315 West Ponce de Leon Avenue Suite 1051 Decatur, GA 30030 404-378-0441