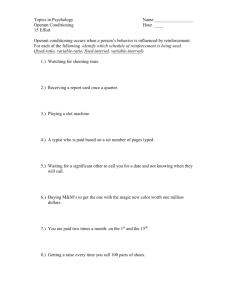
Functional Restoration, Operant and Classical Conditioning in
advertisement

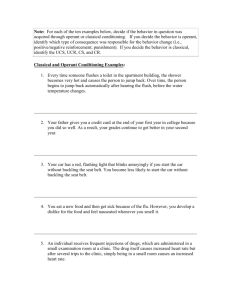
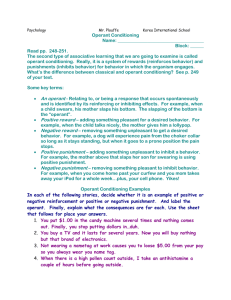
Ronald J. Kulich, Ph.D. Professor, Tufts University Lecturer, Harvard Medical School, Department of Anesthesia, Pain Medicine and Critical Care Massachusetts General Hospital History: Functional Restoration, Operant and Classical Conditioning in Clinical Pain Rehabilitation Reissued 2014 Classical Conditioning Bell Work Tasks Walking Boss Permanent Changes? CS UCR UCS Salivation Fear Autonomic Arousal Escape Food Pain Nausea Operant Conditioning Edward L. Thorndike (1874-1949) B.F. Skinner (1904-1990) Behavior +R Consequence Figure 1 Initial Development of Chronic Pain with Pain Contingent Activity Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Injury Kulich & Gottlieb, 1985 Stone & Kulich, 2015 Tx Time Tx Pain Activity Multiple treatments Figure 2 Development of Disability with Chronic Pain Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx pain-based activity reduced activity Time Tx Kulich & Gottlieb, 1985 Stone & Kulich, 2015 Pain Activity Multiple treatments Functional Restoration & Operant TX (Fordyce, 1967,1968; Mayer, 1987, 1988) Time limited Group based Highly selective Focus on function v. pain Targets RTW Focuses on perception of ability Uses quota-based exercise Outpatient Fordyce, 1976 Fordyce, 1976 Operant Pain Rehab History 70s “Operant” Fordyce 80s “Functional Restoration: Mayer Late 80s “Work Hardening” Mathieson 80s-90s Interdisciplinary Pain Management and Faux Functional Restoration Early 90s Inpatients Units Closed, then Outpatient Programs Closed 2012 Structured programs reemerge in Colorado, Holland Clinician Beliefs: Who makes patients disabled? Lotters et al 2011, Occup. Rehab regardless of the severity of the pain disorder, merely visiting a subspecialist was associated with a failure to fully return to work. Who makes patients disabled? Houben et al. European J. Pain (2005) Differentiated between physical therapists on their biomedical vs biopsychosocial orientations towards non-specific back pain. Therapists with biomedical orientation viewed daily activities as more harmful for the back of a LBP patient Consistent with van der Windt D, Hay E, Jellema P, et al. 2008 on PT training with chronic pain population Exercise, chronic pain and other variables There appears to be little or no relationship between improved physical functioning & performance and measures of mobility, trunk extension, trunk flexion strength, and other related variables. Psychologists fail as well Few current “behavioral” treatment models address objective function or employ operant principles Preliminary data from Jackson & colleagues show <5% of 76 “mindfulness” chronic pain studies employed objective measures of physical functioning A return to time limited, quota-based exercise? Exercise & Pain “…exercise should be a core treatment ... irrespective of age, comorbidity, pain severity and disability. Exercise should include: local muscle strengthening [and] general aerobic fitness.” (National Institute for Health and Care Excellence (NICE) 2014; Geneen L, Smith B, Clarke C, Martin D, Colvin LA, Moore RA, 2014; Wieland, 2013, Busch, 2013). Quota-Based Exercise vs Symptom Contingent “Pacing” Jan 17, 2015 “Compared graded exercise therapy (GET), in which patients gradually increase the length or intensity of a set of exercises; adaptive pacing therapy (APT), a strategy to set modest exercise goals but to stay within an maximum “envelope” of exertion defined by the illness; and cognitive behavioural therapy (CBT), which aims to identify and adjust the thought processes that lead to unhelpful behaviours.” Adapted pacing therapy added nothing to physical function scores White et al., 2011, The Lancet Screening: Who is Appropriate? No medical contraindications for a progressive, quota-based exercise Objective, realistic “micro” and “macro: functional goals No severe psychiatric disorder: Substance abuse, cognitive deficits Somatic focus, fear avoidance, and pain contingent activity is present Depression, anxiety, and “unhappy” with current status Acceptance of the concept that pain relief will not be targeted Acceptance of a diagnostic and pain amelioration endpoint Non-solicitous family or option of family intervention Absence of significant financial support for disability Co-treating clinician cooperation Opioids and other controlled substances ? The “Functional Restoration” Program Objective “Micro/Macro” Goals, excluding Pain Relief Identify Overt and Covert Pain Behaviors Identify “Well” behaviors Identify Reinforcers Address Barriers, e.g., Fear-avoidance, belief about opioids, solicitious family, sabotaging clinicians, “hurt versus harm” High frequency continues +R to intermitant +R Digital monitoring/self-monitoring, structured visits, social reinforcement Consistent Communication + Treatment Agreement Identifying Pain Behaviors Complains of pain Grimacing, limping Maladaptive thoughts, e.g., ruminations about injury, pathophysiology, “correct” posture Use of cane, braces, TENS units Pain contingent medication use Pain contingent physician visits Pain contingent passive treatments, e.g. massage, rest, ice, meditation Pain severity & symptom monitoring “Pacing” to eliminate “flares” Chronic Pain and Disability “Flags”adapted from Main et al 2008 ; Biological Personal and environmental Factors (Psychosocial) Red flags Stone & Kulich, 2016 Serious pathology Medical & Psychiatric co-morbidity Orange flags • Depression • PTSD • Somatoform Disorder/# sites Yellow flags Avoidant coping strategies Emotional distress Passive role Perceived low social support at wk Environmental (systemic) Blue flags Perceived unpleasant work Black flags Legislative criteria for Low job satisfaction Perception of excessive demands compensation Nature of workplace (eg. heavy work) Threats to financial security Pharmacotherapy & Operant Tx Can they mix? The pattern of medication use or other “pain relief” interventions are subject to the same operant principles Physicians reported increases and decreases in function to be the most important measure of success with chronic opioid therapy …while objective functional gains for COT remain elusive N = 82 PCPs, 65 Pain Specialists Nishimori, Kulich, Carwood, Okoye, Kalso, & Ballantyne (2006) Examples: Realistic Goals w/ Fixed Dates Increase function, e.g., walk 30 minute to grocery store by May 20, sit through movie with wife by May 30, lift 30 pound grandchild by May 15 Improve mood and sleep habits, e.g. 10 point change in CES-D, utilize 4 sleep hygiene skills Reduce medical visit frequency, e.g., PCP visit 1x per mo., ortho 1x per year Reduce/eliminate inappropriate medications, (specific medications and dates) Improve relaxation/mindfulness skills Return to volunteering by June 15 Is a Work Goal Realistic? Job & Supervisor Satisfac Job Satisfaction Predicts Injury (Bigos et al., 1991) 3000 Aircraft Employees over 4 years The Item: “I hardly enjoy tasks involved in my job.” “Yes” predicts 2.5 x more likely to incur a back injury Consistent with Frymoyer’s later data on reinjury after discectomy Operant/Functional Restoration Program Sample Treatment Plan and Agreement Congratulations on your enrolment in the Functional Restoration Program. The program is designed for individuals suffering from chronic pain who desire to return to normal levels of physical functioning in all area of life. Similar selective programs have shown great success with motivated individuals who often have tried a long history of other pain treatments, physical therapy and other rehabilitation efforts in the past. Rather than attempting to eliminate pain or providing additional diagnostic tests, the program is designed to assist you in improving overall function and developing the best quality of life despite pain. Our team works closely with you to achieve these goals. agreement cont’d The first step involves determining your specific goals that can be achieved over a 6-8 week period. (See Sample Goal List). After review with your clinician, these goals include: Goal Date 1 Walk to corner store (20 minutes) Exercycle (30 Minutes) May 1 2 Lift Grandchild (20 pounds) Free weights floor to weights (40 pounds) June 1 3 Improve sleep habits Improve Mood (CES-D) May 10 Out to movies with wife (3x) Volunteer work contact + Visit with Mass Rehab Commission Eliminate cane June 1 4 5 April 22 agreement cont’d Achieving Your Goals: We know that goals change. With respect to your exercises or other quality of life goals, we do occasionally adjust these goals in an individual bases, while goals are not changed or adjustment on more than one occasion in the program in order to better insure a clear pain of success. Goals and the components of your program are closely viewed by each clinician on several occasions throughout the day. Schedule: The program is scheduled 2 days per week for approximately 3-4 hours per day . You are expected to attend all sessions, regardless of pain. Given the program’s intensity and goals you have target, absence from two sessions results in discharge. agreement cont’d Other Treatments: One goal of the program is aimed toward minimizing unnecessary medical visits. During the period of the program, all participants are asked to end other pain and physical therapy related treatments. Medication: You are expected to continue on a stable of “fixed” dose of their medications during the program. The medication plan of care is outlined at the beginning of the program by your physician. These include: 1 2 3 4 Medication Dose Prescribed by clonazepam.5 oxycodone 5mg gabapentin 600 mg fluoxetine 20mg 2x per day 3x per day 3x per day 1x per day Jones-PCP BPCC BPCC Smith-Psychiatry agreement cont’d Pain Behavior commonly occurs with individuals who have persistent pain over many months or years. This can be observed by others around you. Other “covert” behaviors include thoughts about your pain that may get in your way of improved functioning. “Well behavior,” physical capacity and improved coping skills are intended to reduce pain behavior. Current pain behaviors discussed by you and your clinician include: Pain Behaviors 1 2 3 4 5 Use of the case Limping, grimacing Increasing oxycodone As-needed use of ice Use of back brace Solicitious Behavior Family members are often important supports for helping you return to functioning. In some cases, it’s helpful to have them observe your exercise effort and plan other family events together: “My family member interested in participating is….” _________________________ Figure 1 Initial Development of Chronic Pain with Pain Contingent Activity Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Injury Stone & Kulich, 2015 Tx Time Tx Pain Activity Multiple treatments Figure 2 Development of Disability with Chronic Pain and Introduction of Quota-based Activity Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx quota-based activity increase Tx reduced activity Time Stone & Kulich, 2015 Tx Pain Activity Quota-based activity Multiple treatments Figure 2 Development of Disability with Chronic Pain Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx Tx pain-based activity reduced activity Time Tx Stone & Kulich, 2015 Pain Activity Multiple treatments Figure 3 Development of Disability with Chronic Pain and Introduction of Quota-based Activity Tx Tx Tx quota-based activity increase reduced activity Time Kulich & Backstrom, in press Tx Pain Activity Quota-based activity Fixed treatments Electronic Activity Trackers Glorified pedometers “Use of pedometer is associated with significant increase in physical activity and decrease in body mass index and blood pressure.” 10-15% error, FitBit 10.1% error “the widespread integration of this technology into medical practice remains limited.”(Appleboom, 2014) • Bravata DM, Smith-Spangler C, Sundaram V, et al. Using Pedometers to Increase Physical Activity and Improve Health: A Systematic Review. JAMA. 2007;298(19):2296-2304. doi:10.1001/jama.298.19.2296. • Appelboom et al.: Smart wearable body sensors for patient self-assessment and monitoring. Archives of Public Health 2014 72:28 Kulich RJ, Berna C, Backstrom J, Mao J. APS 2015 Kulich RJ, Berna C, Backstrom J, Mao J. APS 2015 The early history of aggressive operant approaches Silas Weir Mitchell (1874) offered a treatise on “a lad of 16, who, while oppressed under certain family troubles, still contrived to lead his class… (Then) the headache came on…within a week so severe as to prevent all study….” …the pain was absent, or rare, as long as he rode on horseback, or idled at the seashore, but the slightest methodological use of his brain caused him hours of pain.” Describing a tenderness of the scalp and occipital area pain with increasingly diffuse pain, Mitchell also noted that the patient became progressively irritable and depressed as his pain persisted. He diagnosed that patient as having headache “from over use of brain.” (Mitchell, 1874). Mitchell suggested that the patient assume “a semibarbarous life,” shelving all academic interest, and returning to “camp life…as an incomparable means of cure.” He essentially instituted an intensive, quota-based exercise regimen. In commenting on causation for these stress induced physical maladies, the Boston Medical and Surgical Journal (1853) editorial noted that “many a bright young fellow is broken down by being overwrought.” by their studies. Follow-up Post Treatment Assessment FU Assessment FU Crisis Protocol for Relapse Work, Avocational, Independent Exercise Family +R well behavior FU Treatment Protocol Individual non-prn visits PCP + Managed Subspecialists The correct S. Groups, Relapse Groups