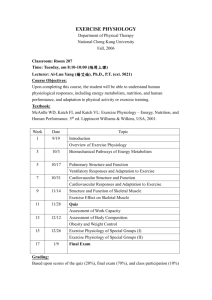
Lecture Note 2 - Cardiovascula
advertisement

Cardiovascular Physiology Definition of terms Cardiac cycle - Refers to the events of one complete heartbeat during which both atria and ventricles contract and then relax. Systole - The time period when the heart contracting. Diastole - The time period when the heart in the state of relaxation. Systolic Pressure - Peak pressure in the arteries when ventricles contract. Diastolic Pressure - Lowest pressure in the arteries when ventricles relax. End-systolic Volume – Volume of blood in the left ventricle at the end of contraction. End-diastolic Volume – Volume of blood in the left ventricle at the end of filling. Cardiovascular Physiology Cardiovascular Physiology Stroke Volume Volume of blood pumped by the heart in one contraction SV = EDV – ESV Where SV - stroke volume EDV - end-diastolic volume ESV - end-systolic volume Stroke volume usually consider only volume of blood pumped from the left side of the heart because that is the amount of blood sent to all the tissues of our body. Cardiovascular Physiology Stroke Volume can increase during exercise. Stroke volume depends on preload, afterload and contractility. Preload The pressure stretching the ventricular walls prior to contraction. Depends on ventricular filling and venous return i.e. return of blood back to the heart. Afterload Pressure the ventricle must generate to eject blood into aorta. Depends on arterial pressure Cardiovascular Physiology Contractility (Inotropy) Force that muscle can create at given length. Cardiovascular Physiology Cardiac Output Amount of blood in liter per minute pumped by the heart particularly the left ventricle. CO = SV x HR Where CO – cardiac output (L/min) SV – stroke volume (L) HR – heart beat rate (beat/min) Normal cardiac output is 5.0 L/min. Cardiovascular Physiology Ejection Fraction Fraction of blood ejected by ventricle relative to enddiastolic volume EF = (SV / EDV) x 100% Normal EF is usually greater than 60%. Cardiovascular Physiology Cardiac Cycle Events that occur in one heart beat. Cardiovascular Physiology Atrial Contraction Semilunar valves close, AV valves open. Pressure within the atrial chambers increases, which forces remaining blood in the chambers flow across the open atrioventricular (AV) valves. Isovolumetric Contraction All valves close. Pressure within ventricles increases. Ventricular Ejection Semilunar valves open, AV valves close. Intraventricular pressure higher than pressure in large arteries. Semilunar valves forced to open, blood rushes out from ventricle. Isovolumetric Relaxation All valves close. Intraventricular pressure falls causes all valves to close. Cardiovascular Physiology Ventricular Filling Semilunar valve close, AV valve open. Intraventricular pressure falls below arterial pressure. Blood flow through the atria into the ventricles. Intraventricular pressure continues to briefly fall because the ventricles are still undergoing relaxation. Once the ventricles are completely relaxed, their pressures will slowly rise as they fill with blood from the atria. Cardiovascular Physiology Pressure-Volume Relationship Cardiovascular Physiology The P-V plot shown here is for left ventricle (LV) a, b, c and d indicate phases in cardiac cycle - a : ventricular filling - b : isovolumteric contraction - c : ejection - d : isovolumetric relaxation Point 1 : end-diastolic pressure (EDP) and end-diastolic volume (EDV). Point 2 : LVP exceeds aortic diastolic pressure, the aortic valve opens, ejection phase begins. Point 3 : aortic valve closes, ventricle relaxes isovolumetrically. Point 4 : LVP falls below left atrial pressure mitral valve opens, ventricle begins to fill. Cardiovascular Physiology ESV – end-systolic volume. EDV – end-diastolic volume. ESPVR – end-systolic pressure-volume relationship EDPVR – end-diastolic pressure-volume relationship SV – stroke volume Stroke Work (SW) Work done by the ventricle to eject a volume of blood (i.e., stroke volume) into the aorta. Basically SW is the area inside the P-V plot. Another term is Cardiac Work which is simply product of SW and heart rate. Cardiac Work = Stroke Work x Heart Rate Cardiovascular Physiology Cardiovascular Physiology HEMODYNAMICS The study of blood flow and blood pressure. Hemodynamics is essential to understand cardiovascular dynamics system. Some basic relationships : F = ΔP/R Where F – blood flow (unit : ml/s) Δ P – pressure difference along vessel (unit : mmHg) R – resistance to flow (if it is not steady and change with time we call it impedance) (unit mmHg/ml/s) Cardiovascular Physiology To apply the concept in heart, suppose we know aortic and intraventricular pressure ventricular ejection. To find flow of blood : F = (PIv - Pao)/R Factors that influence resistance to flow : - length and diameter of vessel - viscosity of blood Cardiovascular Physiology VESSEL TYPE Aorta DIAMETER (mm) 25 FUNCTION Pulse dampening and distribution Large Arteries 1.0 - 4.0 Distribution of arterial blood Small Arteries 0.2 - 1.0 Distribution and resistance Arterioles 0.01 - 0.20 Capillaries 0.006 - 0.010 Venules Veins Vena Cava 0.01 - 0.20 0.2 - 5.0 35 Resistance (pressure & flow regulation) Exchange Exchange, collection, and capacitance Capacitance function (blood volume) Collection of venous blood Cardiovascular Physiology VASCULAR COMPLIANCE ability of a blood vessel wall to expand with changes in pressure. C = ΔV/ΔP C – vessel compliance ΔV – change in blood volume ΔP – change in pressure Reciprocal of compliance is elastance. What is the relationship between blood flow and volume? Frank-Starling Mechanism The change of heart’s force of contraction in response to change in venous return. During exercise, venous return i.e. blood that returns to the heart increased which then causes increase to stroke volume. Frank-Starling mechanism tells how change in venous return will alters the stroke volume. Increased venous return increases the ventricular filling (enddiastolic volume) and therefore preload, which is the initial stretching of the cardiac myocytes prior to contraction. Myocyte stretching causes an increase in force generation. This mechanism enables the heart to eject the additional venous return, thereby increasing stroke volume. Frank-Starling Mechanism Frank-Starling Mechanism