Working Smarter
advertisement

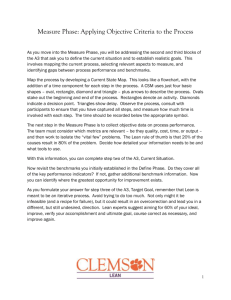
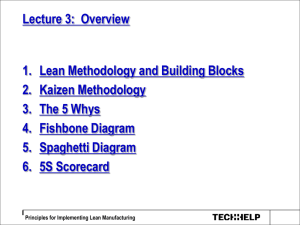
Working Smarter, Not Harder Brett Williamson, LSW, MBA Program Director Objectives 1. 2. 3. 4. Participants will have a basic understanding A3 problem solving process and its application to healthcare services and their own workplace. Participants will learn about specific techniques to perform root cause analysis. Participants will be able to identify processes within their programs where the application of lean methodologies may reduce waste. Participants will be able to apply organization change strategies to promote lean implementation. Why is going Lean so important? ■ Rising Healthcare Costs. ■ Organizational expenses rising 3-5% annually. ■ Behavioral Healthcare Reimbursement not keeping up with expenses. ■ Meeting certain regulations can be labor intensive and lack an adequate reimbursement structure. ■ Organizations are being forced to do more with less. ■ Pay-for-performance standards will force organizations to reduce errors. Lean = Elimination of Waste (muda) ■ 8 categories of waste 1. 2. 3. 4. 5. 6. 7. 8. Overproduction Excessive Inventory Defects Non-value added processing Waiting Underutilized people Excess Motion Transportation There is nothing so useless as doing efficiently that which should not be done at all. ~Peter F. Drucker Nothing stops an organization faster than people who believe that the way you worked yesterday is the best way to work tomorrow. ~Jon Madonna “ Lean solutions involve looking at processes, breaking them down into parts, and eliminating waste.” Establishing lean processes through the elimination of waste improves efficiency, productivity, employees satisfaction and patient satisfaction. -Carol Berczuk, The Lean Hospital, 2008 Change is the Key Every organization has an institutional culture. That same culture can lead to complacency. An attitude of “we have always done it this way” is sure to lead to problems. Organizations must develop a Culture of Leadership where leadership is defined as the ability to cope with change. Leaders are visionaries with a poorly developed sense of fear and no concept of the odds against them. ~Robert Jarvik Our only security is our ability to change. ~John Lilly Traditional vs. Lean Culture 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Traditional Functional silos Managers Direct Benchmark to justify Blame people Rewards: individual Supplier is the enemy Guard information Volume lowers cost Internal Focus Expert Driven 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Lean Interdisciplinary Teams Managers teach/enable Seek ultimate performance, absence of waste Root Cause Analysis Reward: Group sharing Supplier is the ally Share Information Removing waste lowers cost Customer focus Process Driven Institute of Healthcare Improvement, Going Lean in Health Care. Innovation Series 2005 If you want to truly understand something, try to change it. ~Kurt Lewin Organizational Change ■ Kotter’s 8-Step Change Model 1. Create Urgency A. Identify potential threats, develop scenarios showing what could happen in the future. B. Examine opportunities for potential exploitation. Neither a wise man nor a brave man lies down on the tracks of history to wait for the train of the future to run over him. ~Dwight D. Eisenhower 8 Step Change Model 2. Form a Powerful Coalition A. Convince people that change is necessary. B. Bring together influential people. C. The team needs to continue to build urgency and momentum around the need to change. 8 Step Change Model 3. Create a Vision for Change A. Identify the values central to the change. B. Develop a clear and concise summary that describes how you see the future. C. Create a strategy to execute the vision. A leader has the vision and conviction that a dream can be achieved. He inspires the power and energy to get it done.” — Ralph Lauren 8 Step Change Model 4. Communicate the Vision A. Talk about the vision at every opportunity. B. Remember what you do is much more important than what you say. C. Lead by example The difference between the right word and the almost right word is the difference between lightning and the lightning bug. ~Mark Twain The less people know, the more they yell. ~Seth Godin 8 Step Change Model 5. Remove Obstacles A. Identify change leaders in you organization. B. Make sure your organizational structure is in line with your vision. C. Recognize and Reward individual for leading the change. D. Act quickly to remove barriers. 8 Step Change Model 6. Create Short-Term Wins A. Create short-term targets, success motivates. B. Again, reward individual and/or groups for meeting the targets. 8 Step Change Model 7. Build on the Change 1. Analyze each success to determine reasons for success and areas for improvement. 2. Set goals that build on the momentum. 8 Step Change Model 8. Anchor the Changes in Corporate Culture A. Build the culture of change into the hiring process. B. Recognize key leaders of change. Resistance to Change ■ ■ Any Organizational Change will encounter some resistance. Kotter and Schlesinger (2008) stress the importance of recognizing the 4 common reasons people resist change. Kotter and Schlesinger, Choosing Strategeies for Change When you are through changing, you are through. ~Bruce Barton Failure is not fatal, but failure to change might be. ~ John Wooden 4 Reasons for Resisting Change 1. 2. Parochial Self-interest: people resist change because they think they will lose something of value. They will focus on their own best interest not the best interest of the total organization. Misunderstanding and Lack of Trust: when individuals do not understand the implications of the change, they may perceive that they have more to lose than they will gain. Kotter and Schlesinger, Choosing Strategeies for Change 4 Reasons for Resisting Change 3. 4. Different Assessments: people may assess the situation differently than those leading the change and see more costs than benefits for both themselves and the company. Low Tolerance For Change: people fear that they will not be able to develop new skills and behaviors that will be required as a result of the change. Kotter and Schlesinger, Choosing Strategeies for Change Change is hard because people overestimate the value of what they have—and underestimate the value of what they may gain by giving that up. ~James Belasco and Ralph Stayer Flight of the Buffalo (1994) Lean Management Defined ■ ■ Lean management utilizes the systematic elimination of waste from all aspects of an organization's operations. Lean simply means using less to do more. Lean Management Embraces 5 principles ■ ■ ■ ■ ■ Value-What is the customer willing to pay for? Value Stream-Steps to deliver the value Flow-Organizing the Value Stream to be continuous Pull-Responding to customer demand Perfection-Relentless, continuous improvement(Kaizen) Value Added vs. Non Value Added ■ Value Added Activity – Any activity that impacts output or outcome for the customer ■ Non Value Added Activity – Any activity that DOES NOT impact output or outcome for the customer Toyota Production System (TPS) Historical Perspective ■ Between 1948 and 1975, Taiichi Ohno Shigeo Shingo and Eiji Toyoda, develop what is now referred to as the Toyota Production System (TPS). ■ It combines attitudes, themes and specific problem solving techniques into an integrated socio-technical system for manufacturing. ■ More recently, healthcare organizations have adopted and adapted the TPS to help negotiate the ever changing healthcare environment. Toyota’s 14 Principles 1. 2. 3. Management decisions should be made with long-term vision, in lieu of short term financial goals Create continuous process flow to help bring problems to the surface. Use Pull systems to avoid overproduction. Toyota’s 14 Principles 4. Level out the workload 5. 6. 7. 8. Build a culture to stop and fix problems to get it right the first time Standardize processes and tasks Use visual control Use reliable technology Toyota’s 14 Principles 9. 10. 11. Grow leaders to help perpetuate the culture and teach it to others Develop exceptional people Extend your network of partners challenging them to improve Toyota’s 14 Principles 12. 13. 14. Go see for yourself to help thoroughly understand the situation Make decisions slowly by consensus, considering all options, implement decisions rapidly Become a learning organization through reflection and continuous improvement Toyota Principle # 10 Go to the Gemba ■ Gemba - Japanese for the actual place. In management terms this can mean going to where value is created. Going to see the actual place: the source of the problem. The goal is to gain understanding by observing the actual circumstances in which a product/service is used/provided then determine where and when improvements and innovation are possible. This is the cornerstone of the A3 Process. Facts from paper are not the same as facts from people. The reliability of the people giving you the facts is as important as the facts themselves. ~Harold S. Geneen TPS and the A3 ■ ■ A3 thinking is a problem solving tool that was developed and used extensively at Toyota which utilizes Deming's PDCA (Plan-Do-Check-Act) improvement cycle. The following slides will further explain the process The Power of the A3 ■ ■ ■ ■ ■ ■ ■ ■ The A3 offers a simple and consistent way to achieve and document root cause analysis Accountability occurs naturally Testing establishes a safe, experimental attitude and environment Management and staff learn to see problems the same way A3 problem solving occurs as part of everyday work The A3 process documents costs and benefits The A3 template helps us solve problems and document new processes The A3 process is satisfying to everyone, particularly frontline workers A deep understanding of the current conditions is essential to avoid ‘jumping to conclusions. Cindy Jimmerson, Lean Healthcare West in Missoula, Montana Erroneous assumptions can be disastrous. ~Peter Drucker Good management is the art of making problems so interesting and their solutions so constructive that everyone wants to get to work and deal with them. ~Paul Hawken, Natural Capitalism Plan-Do-Check-Act ■ ■ The PDCA cycle is the basis for A3 thinking. The importance of planning is stressed. Toyota’s Principle 12—clearly encourages careful planning, consensus building and rapid implementation. Plan-Do-Check-Act ■ Plan: Define the system, assess the current situation, analyze causes and develop experiments/improvement theories. ■ Do: Run the experiments/improvement theories. ■ Check/Study: Evaluate the results to determine if the experiment worked. ■ Act: Standardize you new process or begin the cycle again depending on the results. The A3 ■ ■ ■ ■ ■ The next slide is an example of an outline that would be utilized to develop an A3. As the form would indicate, the majority of the time is spent in the planning phases which include: Background, Current conditions, Goals/Targets, and Analysis. The Do phase is represented by the Proposed Countermeasures. The Check phase is incorporated into the Plan/Results. The Act phase occurs during follow up. TITLE: ANALYSIS: BACKGROUND Answers the question, “Why are you talking about it?” CURRENT CONDITIONS Choose the simplest problem-analysis tool that clearly shows the cause-and-effect relationship: 5 whys, fishbone, charts, continuous improvement tools, visual aids. Answers the question: “What is the root cause(s) of the problem?” What’s the pain/symptom? Just the facts. Summary, visual, map, pareto diagram, tally sheet, histogram, scatter diagram, control chart, graph Answers the questions, “Where do things stand today?” Countermeasures, Options and Evaluation Answers the questions: “What is your proposal to reach the future state, the target condition? How will your recommended counter-measures affect the root cause(s) to achieve the target? Plan: GOALS/TARGETS: specific, measurable, brief, one or two bullets Answers the question: “What specific outcomes are required” Answers the question: “What activities will be required for implementation and who will be responsible for what and when? What are the indicators/measures of performance or progress?” Just One Technique The 5 Whys ■ ■ A problem solving technique that looks at the end result of a process to reflect on what caused it. By asking the question "Why" the symptoms can be separated from the causes of a problem. This is important because symptoms may often mask the root causes of problems A relentless barrage of "why’s" is the best way to prepare your mind to pierce the clouded veil of thinking caused by the status quo. Use it often. ~Shigeo Shingo Advantages of the 5 Whys ■ ■ ■ ■ ■ ■ Simplicity Effectiveness Comprehensiveness Flexibility Engaging Inexpensive The 5 Why Process 1. Write down the specific problem. Writing the issue helps you formalize the problem and describe it completely. It also helps a team focus on the same problem. 2. Ask Why the problem happens and write the answer down below the problem. 3. If the answer you just provided doesn't identify the root cause of the problem that you wrote down in step 1, ask Why again and write that answer down. 4. Loop back to step 3 until the team is in agreement that the problem's root cause is identified. Again, this may take fewer or more times than five Whys. 5 Why Worksheet www.qualitytrainingportal.com/.../5whys.gif www.qualitytrainingportal.com/.../5whys.gif If you don't ask the right questions, you don't get the right answers. A question asked in the right way often points to its own answer. Asking questions is the ABC of diagnosis. Only the inquiring mind solves problems. ~Edward Hodnett TPS Principle # 6 Standard Work ■ ■ ■ ■ ■ Documentation of the least wasteful way of completing an activity/function. Best Practices are incorporated into standard work. Standard work is the basis for all continuous improvement activities. Eliminate Work-arounds One way to help organize work and work areas is time utilize the 6s process. Engagement Study Muhlenberg Behavioral Health ■ Background – July 2008 thru October 2008 • Poor compliance with initial appointments • 228 scheduled initial appointments • Show rate 79%--48 unused appointments • Yearly projection of unused appointments=144 • Patient complaints regarding lack of access Current Conditions ■ ■ No engagement of client with outpatient program Patients’ expectations and perceptions unclear Goals/Targets ■ Increase show rate by 5-10% Analysis ■ Root cause-poor connection with OP provider-lack of engagement Countermeasures/Plan ■ ■ Contact patient 2-3 days prior to appointment Utilize script to engage patient in the treatment process ■ Explain nature of the visit and expectations ■ Answer any questions OUTCOMES No Contact (n = 12) Left a Voicemail (n = 234) No-show 18% No-show 50% Kept 50% Cancelled 6% Kept 76% Cancelled 0% Left Message w/ Other (n = 77) Spoke w/ Patient No-show 4% No-show 6% Cancelled 2% Cancelled 6% Kept 88% Kept 94% (n = 219) OUTCOMES First Appts: Nov 08–Aug 09 (n = 542) Overall Compliance improves from 79% to 85% No-show 11% Cancelled 4% Kept 85% Future Plans (initially developed after analysis of the data) ■ ■ ■ ■ ■ Develop complementary “script” for referring providers Get “best” contact # from patient – ask the patient, esp if cell phone desired Develop enhanced program brochure for hand-out at D/C, with name & # to call at any time before first appt Roll out to other outpatient programs Implement post discharge calls 2-3 post discharge to “check in”. What steps did we take? ■ ■ ■ ■ ■ ■ Got “best” contact # from patient – ask the patient, especially if cell phone desired Developed enhanced program brochure for hand-out at D/C, with name & # to call at any time before first appt Rolled out to other outpatient programs Encouraged internal providers (higher levels of care, e.g. partial and inpatient). Call for outpatient appointment at admission. Called patient post discharge from higher levels of care. Screened internal referrals more effectively. Follow up data ■ The following charts represent the finding of a study at Muhlenberg Behavioral Health – Conducted FY 10—July 1, 2009 thru June 30, 2010. NO CONTACT (n=28) LEFT VOICEMAIL (n=350) No-show, 4, 14.29% No-show, 43, 12.29% Cancelled, 14, 4.00% Cancelled, 1, 3.57% Kept, 23, 82.14% Kept, 293, 83.71% Kept Cancelled No-show MESSAGE WITH OTHER (n=84) No-show, 3, Cancelled, 3.57% 7, 8.33% Kept, 74, 88.10% SPOKE WITH PATIENT (318) No-show, 8, Cancelled, 2.52% 10, 3.15% Kept, 299, 94.32% All Referrals FY 10 Cancelled, 38, 4.83% No-show, 60, 7.62% Kept Cancelled No-show Kept, 689, 87.55% What next? ■ Out of our initial study, it was determined that we needed to focus on our internal referrals since the noshow/cancellation rate for those individuals was higher than the general population. Background Poor compliance with initial appointments. Lowest compliance was actually discharges from higher levels of care. Compliance is key to: Reducing readmissions Improving quality of care Ensuring patient safety Current Conditions Poor compliance and extended wait times create the following issues: ■ ■ ■ ■ ■ Delivery: wait times 2-3x acceptable standard Delivery: 25-50% no-show rate for initial appointments Quality: Impedes continuity of care and patient safety Cost: Impacts revenue & growth Quantity: Creates rework-Scheduling & rescheduling, etc. Goals/Targets ■ ■ ■ ■ ■ Improve waiting time to 7-14 days post discharge Improve initial appointment compliance to at least 85% Improve patient satisfaction Improve referral source satisfaction Reduce readmissions Analysis ■ ■ ■ ■ ■ Patient safety and continuity of care negatively impacted by long wait time Waiting time for appointments exceeds acceptable standards by 2-3 times 25-50% no-show rate for initial appointments ER visits prompted by long waiting period Difficulty connecting with OP programs Proposed Countermeasures ■ ■ ■ ■ ■ ■ ■ Engagement Process Clarify inclusion-exclusion criteria Standardize referral process Develop insurance matrix for Higher Levels of Care (HLC) HLC connect with OP provider at admission Obtain best contact number for patient Post discharge calls Proposed Countermeasures Chart nd la rra fe :re s -re m sra ey og rv pr su P n O io s at ct m R fa ra is /U og at s pr es rs P oc be er pr ork lO em e al M rg sew for d ha a an s m sc y c or nt es f di t b ke n d tie oc r r c io Pa e p nda nta nta at i k o m a c ta ic or st C f n e in L n s i op arg etro r H s/ ge el h s fo el ar es ev isc x d es i oc isch D r r D oc l pr at da d of Pr M a an C r l r ay L st ce rra s fe D H c. m an re fe op et or f ra ur Re tor le n i le ns og tio ev d I n r u r D o ed P p crip op da m h s el tan O to sc ll ev de OP e S s a s D m er m op aba id ra nd ro el v g a t f o o ev C da lls pr pr L D et H c a r e: op e in rg el nt s en Ta ev tim me /C twe D e ve rD ge b er fo ga k es en ure e lin eria R in t ch tion cri el rm as rfo rou ica on B b n si Pe op mu clu el m ex ev co n/ D e io ov us pr incl op el Im ev D M W W M S S W W W W S W M S W W M S M S S W M S S Improve member satisfaction** W M W M S M S M M M S Improve patient satisfaction* M 20 days <14 days S M W M M S M S S S S <15% 28% Performance Outcomes Reduce the number of no-shows from LVHN higher levels of care Reduce waiting time for initial appointments to acceptable industry standards In Development S= Strong Relationship Completed and implemented M= Moderate Relationship Being explored W= Weak Relationship Plan ■ Meet with inpatient and partial social workers regarding the following: – Begin discharge process on day of admission-allowing lead time for the outpatient programs. – Review inclusion-exclusion criteria – Assess their concerns regarding the referral process Plan continued ■ ■ ■ ■ ■ ■ Implement post discharge calls Dedicated line for internal referrals Standardize referral process Distribute flyers to programs to give to the patients upon discharge Reminder calls Monitor wait time via intake database Wait time FY10 % Internal Intakes Meeting Criteria <15 days Post Discharge from a Higher Level of Care 150.00% 100.00% 100.00% 93.75% 86.36% 83.33% 72.22% 80.00% 66.67% 73.85% 75.00% 70.59% 66.67% 55.56% 52.63% 50.00% 0.00% Jul Aug Sep Oct Nov Dec Jan Feb Mar Month % Meeting Criteria < 15 days Goal Apr May Jun YTD % of Kept Appointments 120.00% 94.12% 100.00% 80.00% 70.00% 77.78% 57.89% 56.25% 60.00% 68.18% 90.00% 87.50% 83.33% 77.78% 100.00% 72.54% 48.15% 40.00% 20.00% 0.00% Jul Aug Sep Oct Nov Dec % Kept Appts (discharges from higher levels of care) Jan Feb Mar Apr May Jun % Kept Appts (discharges from higher levels of care) Goal YTD RESULTS ■ ■ ■ Decreased average wait time from 25 days to 11. Increase show rate from 62% (112 referrals, 69 kept appts.) to 88% (82 referrals, 72 kept appts.) Increase % of patients scheduled within 15 days of discharge form 71% to 82%. Evaluation ■ ■ ■ ■ Discontinue post discharge calls, unable to reach patients, not net effect. Continue engagement calls. Enforce inclusion-exclusion criteria. Monitor wait time and intervene as necessary. Another Case for A3 thinking ■ Background – Increase in accounts receivables and increased referrals to collection. One Definition ■ Buffing the Chart – Verifying benefits – Checking authorizations – Checking visit limits – Checking for claims issues – If issues were encountered, the situation would be dealt with at that time. Current Conditions ■ ■ ■ ■ ■ Total time spent in the process of preparing charts to posting charges was consuming on average 6-7 hours/day of staff time. Continued errors and an excessive amount of rework. Mistakes along the process were increasing the amount of follow up required by the Billing Coordinator. Patient’s being sent to collections. Increase in A/R. Increased billing errors. Goals and Targets ■ ■ ■ ■ ■ Decrease the amount of time spent preparing charts. Decrease A/R. Decrease accounts in collection. Decrease write offs and lost revenue amounts. Decrease posting time. Analysis What is the root cause? 1. 2. 3. 4. 5. Utilized the 5 Whys Why is it taking more time to complete the posting cycle? Why is the work not evenly distributed? Why are staff not performing the tasks at the time events are occurring? Why are staff not entrusted to perform the tasks? Why are staff not cross-trained to perform multiple tasks? Countermeasures and Options ■ ■ ■ Cross train staff to perform all aspects of the posting cycle. Standardize the benefit verification form and process by utilizing the technology available in our billing system. Establish a workflow process that distributed the workload and minimized rework and errors. Plan ■ Standardize a template for benefit verification. The template would be used for all accounts and would be stored electronically. ■ Staff would be trained in posting charges at the time they are received. ■ Establish a step by step process that utilizes staff potential and decreases opportunities for mistakes. Outcomes ■ Standardized template for benefit verification information created and implemented. ■ Reduced A/R. ■ Reduced amount of time for posting process for Billing Coordinator from 3-4 hours to 1 ½ hours with no increase in time spent by other support staff. ■ Reduced time to post charges. One last follow-up ■ ■ Due to the reduction in posting time, our billing coordinator was able to devote more time to past balances. Over the first five months of the project we have collected over $16K in past balances. We should work on the process, not the outcome of the processes. ~Edwards Deming Questions??? References Berczuk, C. (2008). The Lean Hospitial. The Hospitalist, 29-31. Kotter, J. (2001). What Leaders Really Do. Harvard Business Review, 79 (11), 85-96. Retrieved from the Health Business Fulltext Elite Database. Kotter, J. (2007). Leading Change. Harvard Business Review, 85(1), 96-103. Retrieved from the Health Business Fulltext Elite Database. Kotter, J. and Schlesinger, L. (2008). Choosing Strategies for Change. Harvard Business Review, 86(7/8), 130-139. Retrieved from the Health Business Fulltext Elite Database. Hadfield, Debra and Holmes, Shelagh. The Lean Healthcare Pocket Guide XL. MCS Media, Inc. 2008. Graban, Mark. Lean hospitals CRC Press, 2009 Institute of Healthcare Improvement. (2005) Going Lean in Health Care. Innovation Series 2005, 7, p.8 Marchwinski, Chet, Shook, John and, Schroeder, Alexis. Lean Lexicon. The Lean Enterprise Institute, Cambridge, MA, USA. Fourth Edition, March 2008. Serrat, O. (2009). The Five Whys Technique. Knowledge Solutions. Retrieved from http://www.adb.org/Documents/Information/Knowledge-Solutions/The-Five-WhysTechnique.pdf. Shook, John. Managing to Learn: Using the A3 Management Process to Solve Problems, Gain Agreement, Mentor and Lead, Harvard Business School Press, 2002.