Bipolar disorder * prevalence
advertisement

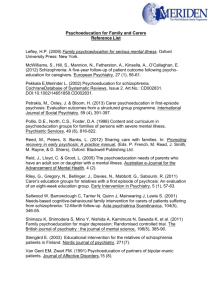
Psychoeducation and other psychological approaches for Bipolar Disorders Dr. Francesc Colom PsyD, MSc, PhD Bipolar Disorders Program IDIBAPS- CIBERSAM -Hospital Clínic Barcelona, University of Barcelona Centro de Investigación Biomédica En Red de Salud Mental Syndromal and Functional Recovery Should Be the Goal of Integrative Treatment Effect Sizes of Psychosocial Treatments Psychotherapy Outcome/Endpoint Effect Size NNT∞ Psychoeducation (Perry et al, 1999)1 Manic relapse .30 4 Psychoeducation (Perry et al, 1999)1 Depressive relapse .16 - Psychoeducation (Colom et al, 2003)2 Relapse during treatment phase .22 5 Psychoeducation (Colom et al, 2003)2 Relapse during 2-year follow-up phase .32 4 Case management (Simon et al, 2005)3 Number of weeks without manic symptoms .14 - Cognitive therapy (Lam et al 2003)4 Relapse/recurrence over 1 year .32 4 Cognitive therapy (Scott et al, 2001)5 Relapse/recurrence over 18 months .45 3 Family-focused therapy (Miklowitz et al, 2003)6 Relapse/recurrence over 2 years .17 6 Interpersonal and social rhythm therapy (Frank et al, 2005)7 Relapse/recurrence over 2 years .57* 4* *For those with < 4 comorbid diagnoses ∞ NNT = number needed to treat 1Perry A, et al. BMJ 1999;318:149-153. F et al. Arch Gen Psychiatry 2003;60:402-407. 3Simon GE, et al. Psychol Med 2005;35:13-24. 4Lam DH, et al. Arch Gen Psychiatry 2003;60:145-152. 2Colom 5Scott J, et al. Psychol Med 2001;31:459-467. DJ, et al. Arch Gen Psychiatry 2003;60:904-912. 7Frank E, et al. Arch Gen Psychiatry 2005;62:996-1004. 6Miklowitz Outcome According to Time Since Last Episode Phase of Disorder Effect Lower Upper P Value EUTHYMIA (Individual) .583 .407 .836 .002 EUTHYMIA (Group) .639 .436 .936 .018 EPISODE IN LAST YEAR .654 .388 1.101 .081 EPISODE IN LAST MONTH .839 .617 1.140 .255 .601 5.098 .292 1.75 ACUTE EPISODE Fixed Combined (5) .703 .582 .851 .000 Random Combined (5) .711 .569 .890 .003 0.1 Scott J, Vieta E & Colom F (2007) 1 10 Psychoeducation for BD… Is NOT: – Just information – Just good medical practice – Just crisis management – “Convincing” the patient – Giving a booklet or a website address to your patients – Self help BUT: – Training – Providing patient’ empowering tools – Enhancing coping strategies – Encouraging informed proactiveness – Agreeing on reasonable targets – Promoting self-care The Modern Patient-Physician Relationship Is Becoming Horizontal Evolving Patient-Physician Relationship Paternalism Partnership One-on-one strategies Team approaches Knowledge gap Educational empowerment “Doctors orders” Mutual decision-making Intervention Prevention Magee M, D’Antonio M. The Best Medicine. New York: Spencer Books; 2001. Magee M. Relationship Based Health Care in the United States, United Kingdom, Canada, Germany, South Africa, and Japan. Presented at the World Medical Association Annual Meeting. Helsinki, September 11, 2003. The proper setting The utopic setting for succeeding in the implementation of psychoeducation Open-door policy. – Less prescheduled appointments but total flexibility for unscheduled visits or in-call availability. – Psychoeducation encourages the patient to have a proactive attitude in dealing with his disorder and so the therapist should have the same proactive and flexible attitude. (Colom, British Journal of Psychiatry, 2011) Why group setting? Allows modeling Allows training Supportive Against stigma Enhances insight Increasessocial network Cheaper Composing a psychoeducation group Beetween 8 and 12 outpatients. Better to start with 16. Balance gender. Balance bipolar subtype. No more than two ages subgroups. Therapist & co-therapists. Suitable schedule. 90 minutes per session. Written material. Who should deliver psychoeducation? Therapist Charachteristics Training: 12 hours ... and 3 years Previous clinical experience with bipolar patients Rather an expert on a disorder than on a technique Previous experience with patients groups Interpersonal skills Common sense Sense of humour Adherence enhancement Early warning signs identification Illness awareness Psychoeducation Substance misuse avoidance Habits regularity Psychoeducation Illness awareness Hospitalization, treatment with antipsychotics M Cocaine Split with Sandra Holidays in Morocco I meet Sandra. I go out every night H Chronicity and recurrence Euthymia Subthreshold cycling d Treatments Consequences Antidepressants Depression. Lost job. D Lithium Triggering factors 17 18 19 20 21 22 23 Psychoeducation Adherence enhancement “In developed countries, adherence among patients suffering chronic diseases averages only 50 percent.” – World Health Organization 2003 Adherence to Long-Term Therapies: Evidence for Action Adherence to Long-Term Therapies: Evidence for action. World Health Organization 2003. Available at: http://www.who.int/chronic_conditions/adherencereport/en/. American Medical Association. The Patient’s Role in Improving Adherence. Available at: http://www.ama-assn.org/ama/pub/article/12202-8427.html. Magee M. Attacking Chronic Diseases in Developing Countries. . Available at: http://www.healthpolitics.com/program_info.asp?p=prog_55. Treatment Adherence in Euthymic Bipolar Patients 13% N=200 27% 60% Good Compliance Medium Compliance Colom F, et al. J Clin Psychiatry 2000;61(8):549-555. Poor Compliance BEAM survey: reasons why patients are concerned about taking medication (% patients) Feel ashamed Feel dependent It is slavery I am a little afraid It is unhealthy Fear of long-term side effects Medication not really needed Side effects My physical condition Treatment is useless Got pregnant 0 5 Patients (%) 10 15 20 25 Morselli et al 2002 Combination Therapy Average Number of Medications in 258 Bipolar Outpatients Followed Up Prospectively for 1 Year 60 20.9% Number of Patients 50 17.1% 18.2% 40 12.0% 12.0% 30 20 6.6% 6.6% 10 0 3.1% 0.8% 0 1 2 3 4 5 6 7 Total Number of Medications Post RM, et al. J Clin Psychiatry. 2003;64(6):680-690. 8 1.9% 9 0.8% 10 Compliance “The extent to which a patient follows medical instructions” Adherence “The extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes – corresponds with agreed recommendations from a health care provider” Haynes RB. Determinants of compliance: the disease and the mechanics of treatment. Baltimore: Johns Hopkins University Press; 1979. Adherence to Long-Term Therapies: Evidence for action. World Health Organization 2003. Lithium Levels During Psychoeducation 0,9 0,8 0,7 0,6 0,5 0,4 0,3 0,2 0,1 0 -6 months N=49 Baseline * p<0,05 * p<0,01 N=120 Colom F, et al. Bipolar Disord, 2005. N=44 * * * 6 months 12 months 18 months 24 months Psychoeducation Control Group Psychoeducation Early warning signs identification Efficacy of Teaching Bipolar Patients Early Detection of Prodromal Signs 1.0 Exp-M Cumulative survival Control-M Exp-D 0.8 Control-D 0.6 0.4 0 20 40 Weeks Exp-M=experimental group, manic; Exp-D=experimental group, depressive. Perry A et al. BMJ. 1999;318:149-153. 60 80 Ernie: •Likes jokes •Talkative •Hyperactive •Sleeping problems Ernie Depressive prodromes: •Likes quiet environment •Enjoys reading for hours •Doesn’t like jokes or surprises •Needs a lot of sleep Bert: •Likes quiet environment •Enjoys reading for hours •Doesn’t like Bertjokes or Hypomanic surprises prodromes: •Needs a lot of •Likes jokes sleep •Talkative •Hyperactive •Sleeping problems Looking for Early Warning Signs in BD A prodrom should be –A behaviour –Operative –Different from the usual behavioral span –Well-known –Subtle Is it a valid early warning sign?? « I sleep less » « I sleep less than 6 hours » Is it a valid early warning sign?? « I increase my smoking » « I smoke more than 15 cigarrettes » Is it a valid early warning sign?? « I feel sexually aroused » « I click on porn websites » Is it a valid early warning sign?? « Increased self- esteem » or « I am joyfull and happier » « I do more than 10 phone calls a day » « Pre-emergency plan » After ticking three or more boxes, the patient contacts his moodwatch and they decide together if the therapist should or should not be contacted. It is helpful to have a pre-agreement stating that, if the moodwatch is sure that an episode is starting, he has the right to contact the therapist. Emergency plan The patient should contact the therapeutic team as soon as possible The patient should start with the « agreed behaviors » as soon as possible We may have pre-arranged « rescue medications » for some patients Psychoeducation Habits regularity Habits regularity in bipolar disorder (Shen et al., 2008) Habits Sleeping habits Sleeping hygiene Physical exercise General health Work & Stress Family Issues Problem solving Psychoeducation Substance misuse avoidance Substance use Avoid “policeman” attitudes Stress importance on avoidance of “softer” drugs – Alcohol – Caffeine – Cannabis Cigarretes withdrawal management Psychological interventions for bipolar disorder: are all the same? Francesc Colom, MSc, PsyD, PhD Bipolar Disorders Program IDIBAPS-CIBERSAM Catalonia 1° AXIS: POLARITY (THE PENDULUM) Predominant Polarity Operational description of a clinical impression 2/3 of past episodes of a given polarity Validated with more than 1000 patients1, 2, 3 Included in ISBD Nomenclature Taskforce recommendations4 ...But neglected by DSM-5 despite all its clinical and therapeutic implications 1. Colom et al., 2006; 2. Rosa et al., 2008; 3. Yang et al., 2013; 4.Tohen et al., 2009 Predominant Polarity ≥2/3 of a patient's past episodes fulfilling DSM-IV criteria for Depression or Mania/ Hypomania MPP DPP UPP Colom et al., JAD, 2006 Predominant Polarity 40 44 56 With PP 2/3 Without PP of total episodes of the same pole 60 Depressive PP (Hypo)manic PP (Colom et al., 2006) Two possible ways of classifying bipolar treatments... Prevention of Depression (buyt not mania) Balanced stabilizer Prevention of Mania (but not depression) Polarity Index A measure of the relative prophylactic efficacy of drugs used in bipolar disorder maintenance treatment NNT depression Polarity Index= NNT mania PI = 1 Predominantly Antidepressive PI Predominantly Antimanic PI Popovic et al., 2012 Polarity Index of medicaments used in maintenance treatment of BD PI = 1 QUE 1.14 Predominantly Antidepressive PI LAM 0.40 VPA 0.49 OXC 0.62 LI 1.39 OLZ2 ZIP ARI RLAI .98 3.91 4.38 12.09 Predominantly Antimanic PI Popovic et al., European Neuropsychopharmacology, 2012 NNT Mania NNT Depression NNT Any episode Polarity Index Psychoeducation¹ 7.5 5.5 4.6 0.73 CBT2 9.6 3.2 4.8 0.33 CBT3 5.7 3.6 4.9 0.63 CBT4 19 5.4 4.8 0.89 Popovic et al., 2013; 1Colom 2003; 2Lam 2003; 3Lam 2005; 4Meyer, 2011 NNT Mania NNT Depression NNT Any episode Polarity Index Enhanced relapse prevention4 40 40 20 1 Family-focused therapy5 4 5.6 5.3 1.40 Brief technique-driven interventions6 3.9 13.1 11.3 3.36 Caregiver group psychoeducation7 5.0 8.9 4.2 1.78 Popovic et al., 2013; 4Lobban 2010; 5Miklowitz 2003; 6Perry 1999; 7Reinares Polarity Index for Adjunctive Psychotherapies in maintenance treatment of BD PI = 1 Enhanced relapse prevention4 Familyfocused therapy5 Caregiver group psychoeduc.7 Brief techniquedriven interv.6 CBT8 CBT2 CBT3 Psychoeducation¹ Popovic et al., 2013 2º AXIS: SEVERITY (THE PIT) Proposed Staging Model for Bipolar Disorder Kapczinski et al, submitted Two possible ways of classifying bipolar treatments... Stage 4: Paliative care: Diminish impact and alleviate some symptoms Stage 3: Remediation & rehabilitation: Reduce burden, improve functioning Stage 2: Maintenance treatments: Reduce # episodes & # days spent ill Stage 0/1: Preventive treatments: Specific for offspring or for cyclothymia Late Medium Early D-prevention M-prevention At risk Efficacy of Teaching Bipolar Patients Early Detection of Prodromal Signs 1.0 Exp-M Cumulative survival Control-M Exp-D 0.8 Control-D 0.6 0.4 0 20 40 Weeks Exp-M=experimental group, manic; Exp-D=experimental group, depressive. Perry A et al. BMJ. 1999;318:149-153. 60 80 Cluster RCT: PATIENTS & THERAPISTS RECRUITED FROM CMHTs (ERP=12 teams; TAU=11 teams) ERP TAU Adjusted hazard ratio 0.79 (95% CI 0.45–1.38) Lobban, F. et al. The British Journal of Psychiatry 2010;196:59-63 Late EW (Ind) Medium Early D-prevention M-prevention At risk Family-focused psychoeducation (Miklowitz et al., Arch Gen Psychiatry 2003) FFT Delays Rehospitalization Longer Than Individual Treatment Cumulative Survival Rate UCLA FFT Study (N=53) 1,0 0,8 0,6 39 Weeks 0,4 0,2 Individually-focused treatment Family-focused treatment 0,0 0 26 52 78 104 Weeks X2 (1) = 3.87, P <.05 Rea, Tompson, Miklowitz et al. J Consult Clin Psychol. 2003 ; 71: 482-492. 130 156 182 Patients’ Recurrences During 15-month Follow-up after Family Psychoeducation % 80 N=113 *p=0.011 70 66 60 50 *p=0.017 42 40 p=0.211 41,1 37,5 29,8 30 17,5 20 p=0.468 10 3,6 0 0 Mood episode Reinares M et al. Bipolar Disord. 2008. Mania/hipomania Depression Control (n=56) Intervention (n=57) Mixed Impact of staging on family psychoeducation Stage I N= 113 Advanced Stages Reinares et al, 2010 Late EW (Ind) FFT Medium Early D-prevention M-prevention At risk CBT in Bipolar Disorders: 1-year follow-up Survival Function at mean of covariates 1.2 1.0 .8 Cum Survival .6 ALLOC .4 therapy .2 control -10 0 10 20 30 40 50 60 Time of first bipolar episode (weeks) (Lam et al., Arch Gen Psychiatry 2003) CBT in bipolar disorder: 2-year follow-up (Lam et al., Am J Psychiatry, 2005) CBT Not Effective in Acutely Ill Patients With Multiple Episodes Recurrences (%) 100 TAU n=126 80 CBT n=127 60 40 20 0 Time (wk) At risk (n) 0 253 8 204 16 168 24 146 32 131 40 117 48 102 56 94 64 84 72 Actuarial cumulative recurrence curves (Kaplan-Meier): intention-to-treat analysis of any recurrence. CBT=cognitive-behavioral therapy; TAU=treatment as usual. Scott J et al. Br J Psychiatry. 2006;188:313-320. Reality is a mess… but not that much Of the 253 patients, 89% (225) were either in episode at baseline or had 2 or more of: – Past history of >12 episodes – Co-morbid axis I/II – Current or past history of substance abuse/dependence – History of attempted suicide (severe) – Forensic history Only 10% of patients in real-life clinical settings present this way (Scott and Colom., 2008) Cumulative proportion without episode A randomized controlled trial of cognitive behavioural group therapy for bipolar disorder 1.0 TAU CBGT 0.8 • 50 euthymic BP I or II • TAU vs. TAU + CBGT 0.6 • ITT: no differences re time to relapse (total, manic, or depressive) 0.4 0.2 0.0 0 20 40 60 80 Weeks CBGT, cognitive behavioural group therapy TAU, treatment as usual Gomes Psychother Psychosom. 2011;80:144. Early input is better % recurrence by treatment group and number of previous episodes CBT, cognitive behavioural therapy TAU, treatment as usual N=253 Scott Br J Psychiatry. 2006;188:313. Late FFT Medium EW (Ind) Group F-Psyched Early D-prevention M-prevention At risk Mean Number of Episodes (5-year Follow-up) 9 Psychoeducation group 8 Control group 7 6 5 * 4 3 * 2 * * * 1 0 Total episodes *P<.05 psychoeducation vs control. Colom F et al. Br J Psychiatry. 2009. Mania Hypomania Mixed Depression Time Spent Ill (5-year Follow-up) 700 P<.001 Psychoeducation group (N=50) 600 Control group (N=49) Days 500 P<.001 400 300 200 P<.05 P<.005 P<.005 100 0 Total Colom F et al. Br J Psychiatry. 2009. Mania Hypomania Mixed Depression IS STRUCTURED GROUP PSYCHOEDUCATION FOR BIPOLAR PATIENTS EFFECTIVE IN ORDINARY MENTAL HEALTH SERVICES? A CONTROLLED TRIAL IN ITALY 102 Bipolar outpatients type I & II Psychoed. group 1 year follow-up (n=57) Controls p-value (n=45) N° of hospitalisations Mean (ds) 0.11 (0.36) 0.47 (0.69) .001 1.75 (7.0) 10.16 (16.8) .001 N° of days of hospitalisation Mean (ds) Exclusion criteria •Axis I comorbidity •Mental retardation (QI <70) •Organic brain damage or deafness SURVIVAL CURVES FOR HOSPITALISATION N° of people hospitalised Psychoed. Group (5 out of 57) Controls (16 out of 45) Candini et al., 2013 Mean time spent in an episode (5-year follow-up) PATIENTS WITH >15 EPISODES AT STUDY ENTRY N.S. N.S. N.S. N.S. N.S. Colom et al., Acta Neuropsychiatrica, 2010 Impact of staging on family psychoeducation Stage I N= 113 Advanced Stages Reinares et al, 2010 Early input is better % recurrence by treatment group and number of previous episodes CBT, cognitive behavioural therapy TAU, treatment as usual N=253 Scott Br J Psychiatry. 2006;188:313. Late FFT CBT Group Psyched Medium EW (Ind) Group F-Psyched Early D-prevention M-prevention At risk Unsolved areas Functional impairment (Ultra)High-risk individuals Therapy availability/implementation problems “Veteran” patients / paliative psychotherapy Dual pathology Physical health Unsolved areas Functional impairment (Ultra)High-risk individuals Therapy availability/implementation problems “Veteran” patients / paliative psychotherapy Dual pathology Physical health Why psychological treatments may not work on patients with >11 previous episodes? Psychotherapy requires some good functioning on attention, learning, executive functioning and memory, and all these could be seriously damaged in veteran patients Lifestyle difficult to change Kindling/sensitization OR… It may be imposiible to see differences from non-treated patients because they have already learnt… (Kapczinsky et al., Expert Rev Neurother, 2009) Functioning Assessment Short Test (FAST) Functional Impairment across Mood States * D>M>E >C * 50 40 * 30 * 20 10 0 Depression (Hypo)mania Euthymia Healthy Controls (Rosa et al., 2010) Functional Impairment in Remitted Bipolar Patients 20 d=1.26, p<0.001 18 16 FAST scores 14 d=1.18, p<0.001 12 10 8 d=0.65, p<0.001 6 d=0.91, p<0.001 d=0.88, p<0.001 4 d=0.33 d=0.35, p<0.004 2 0 total autonomy occupational cognition financial issues Interpersonal leisure time (Rosa et al., 2008) Psychoeducation and functional remediation Within-group effect sizes in functional improvement, by domain of the Functioning Assessment Short Test 0.8 34 0.7 32 0.6 30 Effect size Functioning Assessment Short Test† Changes in functional impairment scores before and after intervention in patients with bipolar disorder 28 26 24 Functional remediation (n=77) Psychoeducation (n=82) 22 Treatment as usual (n=80) 20 0 Time (weeks) ** 0.5 Torrent C, et al. Am J Psychiatry 2013 * 0.4 0.3 0.2 21 0.1 0.0 *p<0.05, **p<0.005 compared with treatment as usual †Higher scores indicate greater impairment * Leisure Interpersonal* Financial Cognitive Occupational* Autonomy Functional remediation Psychoeducation Treatment as usual Functional remediation in BP-II patients (Solé et al., Eur Neuropsy 2015) Functional Remed. Late FFT CBT Group Psyched Medium EW (Ind) Group F-Psyched Early D-prevention M-prevention At risk Unsolved areas Functional impairment (Ultra)High-risk individuals Therapy availability/implementation problems “Veteran” patients / paliative psychotherapy Dual pathology Physical health Family-Focused Therapy for individuals at bipolar risk (Miklowitz et al., 2013) Functional Remed. Late FFT CBT Ad hoc CBT/Psyched Group Psyched Medium EW (Ind) Group F-Psyched FFT-HR Early D-prevention M-prevention At risk Unsolved areas Functional impairment (Ultra)High-risk individuals Therapy availability/implementation problems “Veteran” patients / paliative psychotherapy Dual pathology Physical health :): The SIMPLe Project Main aims Develop a Smartphone application which could: •Empower the self-management of the disorder and improve the outcome through a personalized psychoeducation program. While at the same time: •Becoming a user-friendly device, suitable for daily use. •Non-stigmatizing, discrete and non-invasive. •Sensitive enough to detect mood changes and emergency situations. •Providing tailored psychoeducational contents and encourage behavior change. •Guarantee safety and confidentiality. •Provide useful data for clinical and research purposes. * Clinical trial.gov Identifier: NCT02258711 :): SIMPLe: General app function framework Unsolved areas Functional impairment (Ultra)High-risk individuals Therapy availability/implementation problems “Veteran” patients / paliative psychotherapy Dual pathology Physical health :): The SIMPLe Project What’s next? SIMPLeBand Passive information inclusion Smartphone data log Weareables Rematch (Relapse prEvention through Mobile providers cAll deTailed records (CDRs) Project (Colom, 2012) Newer potential targets for BD psychotherapy Emotional hyperreactivity Social cognition Non-verbal strategies BCT rather than CBT … Few episodes (0-6): Prevention Psychoeducation CBT Pharmacotherapy Most patients: Pharmacotherapy Psychoeducation (adherence empowerment) >12 episodes or Stage >3: Paliative pharmacology Functional remediation Biophysical treatment Centro de Investigación Biomédica En Red de Salud Mental