Chapter 34: Head and Spine Trauma
advertisement

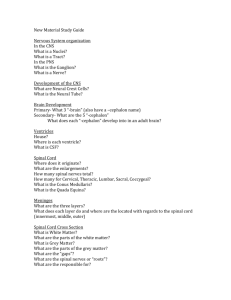
Chapter 34 Head and Spine Trauma National EMS Education Standard Competencies Trauma Integrates assessment findings with principles of epidemiology and pathophysiology to formulate a field impression to implement a comprehensive treatment/disposition plan. National EMS Education Standard Competencies Head, Facial, Neck, and Spine Trauma Recognition and management of • Life threats • Spine trauma National EMS Education Standard Competencies Pathophysiology, assessment, and management of • Penetrating neck trauma • Laryngotracheal injuries • Spine trauma − Dislocations/subluxations − Fractures − Sprains/strains National EMS Education Standard Competencies Pathophysiology, assessment, and management of (cont’d) •Facial fractures •Skull fractures •Foreign bodies in the eyes •Dental trauma National EMS Education Standard Competencies Pathophysiology, assessment, and management of (cont’d) •Unstable facial fractures •Orbital fractures •Perforated tympanic membrane •Mandibular fractures National EMS Education Standard Competencies Nervous System Trauma Pathophysiology, assessment, and management of • Traumatic brain injury • Spinal cord injury • Spinal shock National EMS Education Standard Competencies Pathophysiology, assessment, and management of (cont’d) •Cauda equina syndrome •Nerve root injury •Peripheral nerve injury Introduction • The central nervous system (CNS) consists of the brain and spinal cord. • Two primary divisions of insult: − Head injuries − Spinal cord injury The Scalp • The brain is housed within several layers: − Skin, with hair − Subcutaneous tissue − Galea aponeurotica − Loose connective tissue − Periosteum The Skull • Consists of 28 bones in three anatomic groups. − Auditory ossicles − Cranium − Face The Skull The Skull • Sutures: Special joints where the bones of skull are connected − Fontanelles are tissues that link the sutures. The Skull • Mastoid process: Cone-shaped section of bone at the base of each temporal bone The Skull • The floor of the cranial vault is divided into three compartments: − Anterior fossa − Middle fossa − Posterior fossa The Skull • Base of the skull − The occipital condyles are points of articulation between the skull and the vertebral column. The Brain The Brain • Cerebrum − Largest portion − Responsible for higher functions − Divided into hemispheres The Brain • Diencephalon − Includes the: • Thalamus • Subthalamus • Epithalamus • Hypothalamus The Brain • Cerebellum − Sometimes called “athlete’s brain” − Responsible for maintenance of posture, equilibrium, and coordination The Brain • Brainstem − Consists of midbrain, pons, and medulla − Connects spinal cord to rest of brain − Houses many structures critical to maintenance of vital functions • Reticular activating system (RAS) • Limbic system The Meninges • Protective layers that surround and enfold the entire CNS • Float in cerebrospinal fluid (CSF) The Spine • Consists of 33 irregular bones (vertebrae) • Components include: − Lamina − Pedicles − Spinous processes The Spine • Each vertebra is unique in appearance but shares basic characteristics. − Except the atlas and axis (C1 and C2) The Spine The Spine • Each vertebra is separated by intervertebral disks. − Stress on vertebral column can cause disks to herniate. • May result in nerve root injury The Spine • Spinal cord − Transmits nerve impulses between brain and body The Spine • Spinal nerves − 31 pairs − Named for region and level − Plexus: Cluster that function as a group The Spine • Sympathetic nervous system − Controlled by the hypothalamus − Controls sweating, pupil dilation, temperature regulation, and “flight or fight” responses − Loss of stimulation can disrupt homeostasis. The Spine • Parasympathetic nervous system − Carries signals to organs of the abdomen, heart, lungs, and skin above the waist − Slows heart rate when the sympathetic nerves are stimulated Scene Size-Up • Determine scene safety. • The following should prompt a search for signs of head and brain injuries: − − − − − Motor vehicle crashes Direct blows Falls from heights Assault Sports-related injuries Scene Size-Up • The following indicate the need for full spinal motion restriction: − High-velocity crash with severe vehicle damage − Unrestrained occupant of vehicle crash − Vehicular damage with compartmental intrusion − Fall from three times patient’s height − Penetrating trauma near spine Scene Size-Up • The following indicate the need for full spinal motion restriction (cont’d): − Ejection from moving vehicle − Motorcycle crash − − − − Diving injury Auto-pedestrian or auto-bicycle crash Death of occupant in same compartment Rollover crash (unrestrained) Primary Assessment • Form a general impression. − Note age and gender. − Observe position. − Determine whether condition is life threatening. − Manually stabilize the cervical spine. − Determine the level of consciousness. Primary Assessment • Airway and breathing − Ensure an open airway. − Maintain head and neck in neutral position, and clear the mouth. − Open the airway with the jaw-thrust maneuver if unresponsive or unable to maintain airway. Primary Assessment • Airway and breathing (cont’d) − If intubation is required: • Preoxygenate with 100% oxygen. • Administer lidocaine IV push. • Perform intubation with head in neutral in-line position. Primary Assessment • Airway and breathing (cont’d) − Evaluate breathing. − Monitor oxygen saturation, and maintain at 95% or higher. − Inadequate respirations require ventilation. Primary Assessment • Circulation − In absence of pulse, initiate CPR. − Control major bleeding with direct pressure. − Compare radial and carotid pulses. Primary Assessment • Circulation (cont’d) − Examine skin color, temperature, and moisture. − Volume resuscitation might be necessary. • Do not administer dextrose-containing solutions. • Restrict use for severe closed head injury. Primary Assessment • Transport decision − If patient is unstable, transport immediately. − Consider air transport if time will be prolonged. − Patients with severe brain injuries and increased ICP require neurosurgical intervention. History Taking • Patient’s reliability should be assessed. − Unreliable patients should have continuous spine protection until injury can be excluded. • Maintain a high index of suspicion. • Obtain SAMPLE history. Secondary Assessment • Obtain complete set of baseline vital signs. • Modify examination of any patient with suspected SCI based on: − Level of consciousness − Reliability as a historian − Mechanism of injury Secondary Assessment • Use DCAP-BTLS. • Evaluate distal PMS for all four extremities. • Expose the patient for your examination. − Cut away the patient’s clothes. − Observe the back and palpate the spine. Secondary Assessment • Placement on the backboard − Document before and after immobilizing. − Most patients can be log rolled. − Keep time on backboard to minimum. Secondary Assessment • Complete a full-body exam en route. − Head − Neck − Chest Abdomen − − − − Pelivs Extremities Back Buttocks Secondary Assessment • Level of consciousness − Obtain a complete GCS score. − Indicates extent of brain dysfunction Secondary Assessment • Pupillary assessment − Monitor size, equality, and reactivity of pupils. − When a light is shined into the eye, the pupil should briskly constrict. AAOS Secondary Assessment • Assessing ICP − Critical treatment decisions are based on key findings. − Secondary Assessment • Neurologic exam − Intended to establish a baseline for later comparison. − Determine the level of consciousness. Secondary Assessment • Neurologic exam − Myotomes: Regions where motor components of spinal nerves innervate tissues and muscles Secondary Assessment Secondary Assessment Secondary Assessment • Dermatomes: Regions where sensory components of spinal nerves innervate Reassessment • Monitor vital signs: − Every 5 minutes in unstable patient − Every 15 minutes in stable patient • Be alert for hypotension without other signs of shock. Reassessment • Check interventions. • Repeat the physical exam and reprioritize. • Document suspected spinal cord injury. Head Injuries • Traumatic insult to the head that can result in injury to soft tissue, bony structures, or the brain • Two general types: − Closed head injury − Open head injury Skull Fracture • Significance is related to: − Type of fracture − Amount of force − Area of head that sustained the blow • Potential complications: − Intracranial hemorrhage − Cerebral damage − Cranial nerve damage Skull Fracture • Linear skull fractures − Account for 80% of all skull fractures − No gross physical signs Skull Fracture • Depressed skull fractures − Result from highenergy direct trauma − Patients often present with neurologic signs. Skull Fracture • Basilar skull fractures − Usually occur following diffuse impact to head − Signs include: • CSF drainage • Raccoon eyes • Battle sign Skull Fracture • Open skull fractures − Result of severe force − Brain tissue might be exposed. − High mortality rate Traumatic Brain Injury • Classified into: − Primary brain injury • Injury to the brain and its associated structures − Secondary brain injury • After-effects of primary injury Traumatic Brain Injury • The most common cause is a motor vehicle crash. • Coupe-contrecoup − Front-and-rear type of injury Intracranial Pressure • An increase in ICP can be caused by: − Accumulation of blood within the skull − Swelling of the brain • Increase in ICP decreases cerebral perfusion pressure (CPP) and blood flow. − CPP = MAP - ICP Intracranial Pressure • Early warning signs of ICP: • Ominous signs: − Vomiting − Headache − Hypertension − Bradycardia − Cushing triad − Altered level of consciousness − Seizures − Nonreactive pupil − Coma − Posturing • Decorticate • Decerebrate Diffuse Brain Injuries • Cerebral concussion − Brain is jarred around in the skull. − Signs include: • Confusion, disorientation • Loss of consciousness • Retrograde amnesia • Autograde (posttraumatic) amnesia Diffuse Brain Injuries • Diffuse axonal injury (DAI) − Associated with or similar to a concussion − Involves stretching, shearing, tearing of nerve fibers and axonal damage − Classified as mild, moderate, or severe Focal Brain Injuries • Cerebral contusion − Brain tissue bruised and damaged in local area − Greater neurologic deficits − Swelling of the brain leads to increased ICP. Focal Brain Injuries • Intracranial hemorrhage − Epidural hematoma • Accumulation of blood between skull and dura mater • Result of blow to the head Focal Brain Injuries • Intracranial hemorrhage (cont’d) − Subdural hematoma • Accumulation of blood beneath dura mater outside the brain • Associated with venous bleeding • Acute or chronic Focal Brain Injuries • Intracranial hemorrhage (cont’d) − Intracerebral hematoma • Bleeding in brain tissue • Patient’s condition deteriorates quickly. Focal Brain Injuries • Intracranial hemorrhage (cont’d) − Subarachnoid hemorrhage • Bleeding into subarachnoid space • Patient presents with sudden, severe headache. Focal Brain Injuries • Intracranial hemorrhage (cont’d) − Subgaleal hemorrhage • Bleeding between periosteum and galea aponeurosis − Supragaleal hemorrhage • Firm, nodular mass Assessment and Management • Should be guided by factors such as: − Severity of injury − Patient’s level of consciousness Assessment and Management • Thermal management − Do not allow patient to develop hyperpyrexia. • Treatment of associated injuries − Apply loose, sterile dressings. − Objects impaled should be stabilized. Assessment and Management • Pharmacologic therapy − May be ordered if transport will be prolonged − Benzodiazepines should be used for seizures. − No neuroprotective agents are currently administered in a prehospital setting. Pathophysiology of Scalp Lacerations • Can vary between minor and serious • Can lead to significant blood loss − Do not become distracted by the injury. Assessment and Management of Scalp Lacerations • Consider the mechanism. − Inspect for missing tissue, impaled objects, or residual contaminants. − Evaluate for signs of continued bleeding. Assessment and Management of Scalp Lacerations • In isolated lacerations, stop the bleeding. • Do not explore the injury. − This may disrupt a clot formation and reinitiate bleeding. Pathophysiology, Assessment, and Management of Spine Injuries • Spinal cord injury (SCI) has limited treatment options. − Reducing incidence is best option for decreasing associated morbidity and mortality. Flexion Injuries • Result from forward movement of head • Typically result of rapid deceleration or direct blow to occiput Rotation with Flexion • The only area of the spine that allows for rotation is C1–C2. • Injuries are considered unstable. Vertical Compression • Transmitted through vertical bodies • Result from direct blow to crown or rapid deceleration from a fall Hyperextension • Results in fractures and ligamentous injury of variable stability Primary Spinal Cord Injury • Occurs at moment of impact • Spinal cord concussion − Temporary dysfunction lasts 24 to 48 hours. − May be due to a short-duration shock or pressure wave within the cord Primary Spinal Cord Injury • Spinal cord contusions − Caused by fracture, dislocation, or direct trauma • Cord laceration − Caused when a projectile or bone enters the spinal canal Secondary Spinal Cord Injury • Occurs when multiple factors permit a progression of the primary SCI • Classified as either complete or incomplete Secondary Spinal Cord Injury • Anterior cord syndrome − Displacement of bony fragments into anterior portion of the spinal cord − Findings include paralysis below level of insult • Central cord syndrome − Hyperextension injuries to the cervical area − Loss of function in upper extremities Secondary Spinal Cord Injury • Posterior cord syndrome − Associated with extension injuries − Presents as decreased sensation to: • Light • Touch • Proprioception • Vibration Secondary Spinal Cord Injury • Cauda equina syndrome − Compression of bundle of nerve roots − Can produce the following: • Low back pain • Myalgia, paresthesia, or myasthenia • Loss of sensation • Acute bladder/bowel dysfunction Secondary Spinal Cord Injury • Brown-Séquard syndrome − Functional hemisection of the cord; complete damage to spinal tracts on involved side • Spinal shock − Temporary local neurologic condition that occurs immediately after spinal trauma. Secondary Spinal Cord Injury • Neurologic shock − Results from temporary loss of autonomic function at the level of injury − Hemodynamic and systemic effects are seen. Assessment and Management • Current principles of spine trauma management include: − Recognition of potential or actual injury − Appropriate immobilization − Reduction or prevention of secondary injury Assessment and Management • Patient may not require immobilization if: − No neurologic deficit − Not under influence of alcohol, drugs, or medications − No distracting injuries − No motor or sensory deficit − No pain or tenderness Spinal Splinting Procedures for Supine Patients Spinal Splinting Procedures for Supine Patients • Do not force the head into a neutral, in-line position if the patient has: − Muscle spasms in the neck − Increased pain with movement − Numbness, tingling, or weakness − Compromised airway or ventilation Spinal Splinting Procedures for Seated Patients • A rigid cervical collar should be measured and placed appropriately. • A vest-type board should be used to transfer the patient onto a long backboard. Spinal Splinting Procedures for Seated Patients Spinal Splinting Procedures for Rapid Extrication • Use in the following situations: − Vehicle or scene is unsafe − Patient cannot be assessed before being removed from the car. − Patient needs immediate intervention. − Patient’s condition requires immediate transport. − Patient blocks access to another injured patient. Spinal Splinting Procedures for Rapid Extrication Spinal Splinting Procedures for Standing Patient Packaging and Removal of Injured Patients from the Water • Assume spinal injury for the following: − Diving injury − Boating injury − Watercraft injury − Falls from heights Packaging and Removal of Injured Patients from the Water Patients Wearing Helmets • Helmet removal is recommended in the following situations: − Helmet and chin strap fail to hold head securely. − Helmet and chin strap prevent airway control. − Helmet with a face mask cannot be removed. − Helmet prevents proper immobilization. Patients Wearing Helmets Pharmacotherapy of Spinal Cord Injury • Short-acting, reversible sedatives are commonly recommended for acute agitation. • Pain medication may be necessary. • Corticosteroids are sometimes used in the acute phase of SCI. Complications of Spinal Cord Injury • Potential for aspiration or respiratory arrest • Predisposal to atelectasis and pneumonia • Deep vein thrombosis and pulmonary embolism Complications of Spinal Cord Injury • Autonomic dysreflexia − Potentially life threatening − Most commonly occurs with injuries above T4–T6 − Patients present with a massive, uncompensated cardiovascular response. Complications of Spinal Cord Injury • Autonomic dysreflexia (cont’d) − Common precipitators include: • Skin lesions • Constrictive clothing • Sharp objects compressing the skin − Management is usually not a prehospital intervention. Nontraumatic Spinal Conditions • Back pain is one of the most common physical complaints. • Risks for developing low back pain include: − Occupations that require repetitive lifting − Exposure to vibrations − Comorbid diseases such as osteoporosis Nontraumatic Spinal Conditions • When evaluating: − Consider disease processes that can result in debilitating lesions. − Keep anatomy and neurophysiology in mind. − Pay attention to medications. Nontraumatic Spinal Conditions • Degenerative disk disease − Disk loses height and shock-absorbing effect. − Disk herniation may be caused. • Prehospital management is directed at decreasing pain or discomfort. Injury Prevention • Prevention includes safety measures that can decrease risk of injury. − Driving safely − Adhering to posted safety alerts Summary • The skull does not accommodate a swelling brain or accumulations of blood. • Be familiar with high-risk mechanisms of injury that can cause head injury, brain injury, and spinal cord injury. • Airway is a priority; maintain the head and neck in neutral alignment while you are suctioning and performing airway management. Summary • Control major bleeding without placing pressure on a potential underlying fracture. • Transport patients with severe injuries promptly to a trauma center. • Level of consciousness should continuously be assessed, including repeat assessments of the Glasgow Coma Scale score and pupillary assessment. Summary • Head injuries include skull fractures and traumatic brain injury. • Increased intracranial pressure can squeeze the brain against the interior of the skull and/or press it into sharp edges within the cranium. Summary • Cerebral perfusion pressure is the pressure of blood flowing through the brain; it is the difference between the mean arterial pressure and intracranial pressure. • If the cerebral perfusion pressure drops below 60 mm Hg in the adult, cerebral ischemia will likely occur. Summary • Begin treatment of a head-injured patient by stabilizing the cervical spine, opening the airway with the jaw-thrust maneuver, and assessing the ABCs. • All head-injured patients should receive 100% oxygen as soon as possible. • Avoid routine hyperventilation of a braininjured adult unless signs of cerebral herniation are present. Summary • Restrict IV fluids in a head-injured patient unless hypotension (systolic blood pressure of less than 90 mm Hg) is present. • Frequently monitor a head-injured patient’s level of consciousness, and document your findings. • Intubation of a brain-injured patient may require pharmacologic adjuncts. Summary • Seizures may occur in a brain-injured patient and can aggravate intracranial pressure and cause or worsen cerebral ischemia. • A brain-injured patient’s survival depends on recognition of the injury, prompt and aggressive prehospital care, and rapid transport to a trauma center that has neurosurgical capabilities. Summary • Do not become distracted by scalp lacerations. Once life threats are managed, evaluate the wound for continued bleeding. • In order to decipher the often subtle findings associated with a spinal cord injury, you need to understand the form and function of spinal anatomy. • Acute injuries of the spine are classified according to the associated mechanism, location, and stability of injury. Summary • Vertebral fractures can occur with or without associated spinal cord injury. • Stable fractures typically involve only a single column and pose a lower risk to the spinal cord. Summary • Primary spinal cord injury occurs at the moment of impact. Secondary spinal cord injury occurs when multiple factors permit a progression of the primary spinal cord injury. • Limiting the progression of secondary spinal cord injury is a major goal of prehospital management of spinal cord injury. Summary • Current principles of spine trauma management include recognition of potential or actual injury, appropriate immobilization, and reduction or prevention of the incidence of secondary injury. • Short-acting, reversible sedatives are recommended for the acute patient after a correctible cause of agitation has been excluded. Summary • The use of corticosteroids in the acute phase of spinal cord injury is controversial. • The complications of spinal cord injury are a consistent cause of the high morbidity and mortality associated with this type of injury. • Back pain is one of the most common physical complaints to present to emergency departments throughout the United States. Credits • Chapter opener: © Mark C. Ide • Backgrounds: Blue – Jones & Bartlett Learning. Courtesy of MIEMSS; Gold – Jones & Bartlett Learning. Courtesy of MIEMSS; Green – Jones & Bartlett Learning; Purple – Jones & Bartlett Learning. Courtesy of MIEMSS; Red – © Margo Harrison/ShutterStock, Inc. • Unless otherwise indicated, all photographs and illustrations are under copyright of Jones & Bartlett Learning, courtesy of Maryland Institute for Emergency Medical Services Systems, or have been provided by the American Academy of Orthopaedic Surgeons.