Diagnosis of Congenital Hemorrhagic Coagulopathies
advertisement

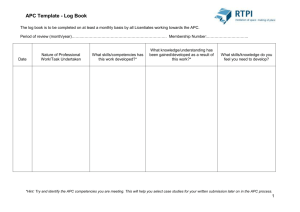
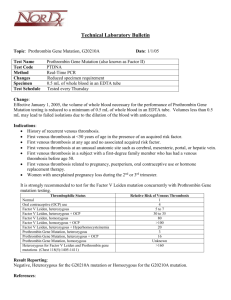
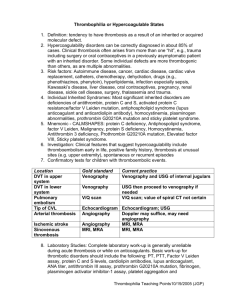
International Hemostasis VIP Meeting China, 2006 Armando Tripodi <armando.tripodi@unimi.it> Angelo Bianchi Bonomi Hemophilia and Thrombosis Center University of Milan Italy TRIPODI TRIPODI Settings where the Laboratory can help Clinicians • Diagnosis of congenital hemorrhagic coagulopathies (pre-surgical screening) • Thrombophilia testing and aPL/LA Syndrome • Diagnosis of acute venous thromboembolism • Heparin monitoring • Oral anticoagulant monitoring TRIPODI Settings where the laboratory can help clinicians Diagnosis of Congenital Hemorrhagic Coagulopathies (pre-surgical screening) TRIPODI Congenital Hemorrhagic Coagulopathies Aims of Laboratory Investigation • To establish the causes of bleeding in patients who have shown evidence of abnormal bleeding • To detect mild defects in asymptomatic patients TRIPODI Congenital Hemorrhagic Coagulopathies Most Important Screening Test Good Clinical History TRIPODI Congenital Hemorrhagic Coagulopathies Why should clinical history be collected • Poor sensitivity of screening tests to detect mild defects • The type of bleeding may provide valuable clue to its etiology TRIPODI Aims of the Clinical History To establish • • • • Type of bleeding Location, frequency, duration, severity Whether it is spontaneous or post-traumatic Whether other family members have the same symptoms • The age of appearence of the first symptoms • Whether other diseases are present • Whether the patients is taking drugs TRIPODI Main Bleeding Symptoms • Bleeding from mucous membranes is a typical feature of platelet disorders • Soft-tissue bleeding is a typical feature of coagulation disorders • Umbilical cord and delayed bleeding are typical feature of factor XIII deficiency • Simultaneous bleeding from multiple sites suggests an acute, acquired systemic coagulation or fibrinolytic disorders TRIPODI Laboratory Tests They should be • • • • Sensitive Limited in number Easy to do Their results clinically-relevant TRIPODI Diagnosis of Congenital Hemorrhagic Coagulopathies • First Step (Simple Screening Tests) - To detect most frequent and well established causes of bleeding • Second Step (Specific Tests) - To detect less common causes of bleeding due to abnormalities to which the screening tests are insensitive TRIPODI Diagnosis of Congenital Hemorrhagic Coagulopathies First Step • Primary Hemostasis - Platelet count - Bleeding Time (or alternative tests) • Coagulation - Prothrombin time (PT) - Activated partial thromboplastin time (APTT) TRIPODI Further Evaluation of Primary Hemostasis • Low Platelet Count - Investigation of thrombocytopenia • Prolonged Bleeding Time - Measurement of plasma Willebrand factor - Platelet aggregation studies TRIPODI Further Evaluation of Coagulation PT/APTT Prolongation Mixing Correction Factor assay TRIPODI No correction Screening for LA Inhibitor assay Diagnosis of Congenital Hemorrhagic Coagulopathies • First Step (Simple Screening Tests) - To detect most frequent and well established causes of bleeding • Second Step (Specific Tests) - To detect less common causes of bleeding due to abnormalities to which the screening tests are insensitive TRIPODI Diagnosis of Congenital Hemorrhagic Coagulopathies Second Step • Factor XIII deficiency • Fibrinolysis defects - tPA, PAI, α2PI • Von Willebrand factor deficiency • Dysfibrinogenemia TRIPODI Settings where the laboratory can help clinicians Thrombophilia Testing and aPL/LA Syndrome TRIPODI Thrombophilia • It may be defined as a condition characterized by an increased risk of thromboembolism at relatively young age • It may secondary to congenital, or acquired causes and some of them may be detected by laboratory investigation TRIPODI Laboratory Diagnosis of Thrombophilia Conditions to be investigated • Congenital - Antithrombin, protein C, protein S deficiencies - APC-resistance (factor V Leiden) - Hyperprothrombinemia (prothrombin mutation) - Dysfibrinogenemia • Acquired - Moderate hyperhomocysteinemia - Antiphospholipid antibody syndrome TRIPODI Naturally Occurring Anticoagulants HMKW PK XIIa XI XIa Antithrombin-Heparin IX IX VIIa-TF IXa VIIIa X X Xa Va II Fibrinolysis TRIPODI Fibrin IIa Fibrinogen Main Characteristics of Congenital Antithrombin Deficiency Inheritance Values in affected members Thrombotic symptoms Possible predisposing factors Autosomal dominant ~ 50% (functional assay) Deep vein thrombosis Pregnancy, surgery, oral contraceptives, etc. Prevalence in patients with venous thrombosis 2-4% Prevalence in the general population Rare TRIPODI Naturally Occurring Anticoagulants HMKW PK XIIa XI Antithrombin-Heparin XIa IX Protein C Protein S IXa VIIIa X IX VIIa-TF X Xa Va II Fibrinolysis TRIPODI Fibrin IIa Fibrinogen Main Characteristics of Congenital Protein C/Protein S Deficiency Inheritance Values in affected members Thrombotic symptoms Possible predisposing factors Prevalence in patients with venous thrombosis Prevalence in the general population TRIPODI Autosomal dominant Heterozygous: Homozygous: (functional assay) ~ 50% < 10% Deep vein thrombosis, superficial thrombophlebitis Pregnancy, surgery, oral contraceptives, etc. 4-8% Rare APC Resistance Control Patient TRIPODI Dahlbäck et al, 1993 Main Causes of APC Resistance • Congenital (85% of all cases) - Factor V Leiden mutation (the vast majority) - Factor V Cambridge mutation (very rare) • Acquired - Elevated coagulation factor levels - Pregnancy - Oral contraceptives intake - Lupus anticoagulants TRIPODI APC Resistance Types of measurement • Plasma analysis (APTT-based method) - Simple - Cheap - Sensitive to acquired APC resistance, not only to FV Leiden • Plasma analysis (APTT-based method with FV-def. plasma) - 100% specific for FV Leiden • DNA analysis - Does not detect acquired APC resistance TRIPODI APC Resistance APTT-based Method • It consists of two APTT - With APC - Without APC • Results Expression - APC ratio = APTT with APC APTT without APC • Interpretation - Lower than normal APC ratio suggests “APC resistance” TRIPODI Main Characteristics of Congenital APC Resistance (FV Leiden) Inheritance Values in affected members Thrombotic symptoms Possible predisposing factors Prevalence in patients with venous thrombosis Prevalence in the general population TRIPODI Autosomal dominant Heterozygous: low APC-ratio Homozygous: very low APC-ratio Deep vein thrombosis Pregnancy, surgery, oral contraceptives, etc. 20-60% 3-15% in Caucasians Prothrombin mutation • Genetic transition - G-to-A at position 20210 in the prothrombin gene (untranslated region) • Phenotypic expression - High levels of plasmatic prothrombin • Clinical expression - Increased risk of venous thromboembolism TRIPODI Main Characteristics of Congenital Hyperprothrombinemia (Prothrombin mutation 20210) Inheritance Values in affected members Thrombotic symptoms Possible predisposing factors Prevalence in patients with venous thrombosis Prevalence in the general population TRIPODI Autosomal dominant Heterozygous: 110-130% Homozygous: > 130% Deep vein thrombosis Pregnancy, surgery, oral contraceptives, etc. 6-18% 2-3% in Caucasians Main Characteristics of Congenital Dysfibrinogenemia Inheritance Main laboratory features Symptoms Prevalence in patients with venous thrombosis Prevalence in the general population TRIPODI Autosomal recessive Discrepancy between immunologic and functional fibrinogen, prolonged thrombin clotting time None, hemorrhage, venous and arterial thrombosis Rare Very rare Main Characteristics of Hyperhomocysteinemia Congenital Deficiency of CBS, MS, abnormal (absent or thermolabile variant) MTHFR. Acquired Vitamin deficiency (folate, B12), age, gender, chronic renal failure. Values in affected subjects Symptoms Prevalence in patients with venous thrombosis TRIPODI Moderate: Medium: Severe: 15-30 µM 30-100 µM > 100 µM Moderate: arterial, venous thrombosis Severe: homocystinuria syndrome 10-20% Main Characteristics of Antiphospholipid Antibody syndrome Clinical features Laboratory features Prevalence in patients with thrombosis TRIPODI Arterial and/or venous thrombosis, pregnancy loss repeated positive solid-phase antiphospholipid-(protein) antibodies (anticardiolipin, anti-b2GPI) and/or lupus anticoagulant tests Unknown Antiphospholipid Antibody Syndrome Laboratory diagnosis • LA and solid-phase antiphospholipid antibodies coexist in about 2/3 of the patients with the syndrome • Diagnosis must be based on both LA and solid-phase antiphospholipid antibodies detection TRIPODI Phospholipid-dependent tests for lupus anticoagulants • • - APTT and dilute PT Relatively insensitive KCT (or SCT) and dRVVT Sensitive Patients with higher dRVVT-ratio than KCTratio are more likely to develop thrombosis?? TRIPODI Antiphospholipid Antibody Syndrome Solid-phase antibodies • • • • • TRIPODI Anti-cardiolipin Anti-b2-Glycoprotein I Anti-phosphatidylserine Anti-prothrombin Anti-PS, anti-PC, anti-Annexin V Laboratory Diagnosis of Antiphospholipid Syndrome Recommendations • Search for LA - At least two phospholipid-dependent tests (screen and confirm) • Search for solid-phase antiphospholipid antibodies - Anti-cardiolipin - Anti-β2-GPI TRIPODI Laboratory Diagnosis of Thrombophilia Who should be tested • Patients with history of thrombosis • Family members • No general screening of the population for APC resistance • Is prophylactic APC resistance testing beneficial in association with risk situation? TRIPODI Laboratory Diagnosis of Thrombophilia When is it appropriate to test • After (and far from) a thrombotic episode • After discontinuation of oral anticoagulation • After delivery and puerperium TRIPODI Settings where the laboratory can help clinicians Diagnosis of Acute Venous Thromboembolism TRIPODI Diagnosis of Deep Vein Thrombosis • Clinical - Unrealiable • Plebography - Gold Standard • Compression ultrasonography (CUS) - Reliable (if thrombosis is proximal) • D-Dimer measurement - High negative predictive value when used in combination with clinical probability TRIPODI D-Dimer • D-dimer results from the plasmin-mediated degradation of cross-linked fibrin - It is an index of fibrin deposition - It is not specific for venous thromboembolism - It has a high negative predictive value for the diagnosis of venous thromboembolism, especially if used in combination with the clinical probability TRIPODI Diagnosis of Venous Thromboembolism (VTE) Combination of Clinical Probability and D-dimer Symptomatic VTE D- Dimer Clinical probability Negative D-Dimer and Low clinical probability Negative D-dimer and High clinical probability Positive D-Dimer Exclude VTE Further Investigation Further investigation TRIPODI D-Dimer to Establish the Optimal Duration of Oral Anticoagulant Treatment (OAT) G. Palareti et al, NEJM 2006 • Patients with a first episode of unprovoked VTE were on OAT for a minimum of 3 months • D-Dimer was measured after 1 month after cessation of OAT • Patients with normal D-Dimer did not continue OAT • Patients with elevated D-Dimer were randomized either to stop or resume OAT • All patients were followed up for an average of 1.15 years to assess for recurrent VTE TRIPODI D-Dimer to Establish the Optimal Duration of OAT Cumulative incidence of outcomes Palareti et al. NEJM 2006 0.20 Elevated D-Dimer No OAT 11.7% patient-years 0.15 0.10 Normal D-Dimer 4.2% patient-years 0.05 2.0% patient-years Elevated D-Dimer + OAT 0.00 0 TRIPODI 100 200 300 Days 400 500 600 Settings where the Laboratory can help Clinicians Heparin monitoring TRIPODI Type of Heparins • • - Unfractionated Heparin Treatment of acute venous thromboembolism Prophylaxis Low Molecular Weight Heparin Treatment of acute venous thromboembolism Prophylaxis TRIPODI Monitoring Unfractionated Heparin • Treatment of acute venous thromboembolism - APTT (therapeutic interval: from 1.5 to 2.5 the basal value) • Prophylaxis - In general no monitoring is required TRIPODI Monitoring Low Molecular Weight Heparin • Treatment of acute venous thromboembolism - In general no monitoring is required - When monitoring is required, the test of choice is the anti-factor Xa activity • Prophylaxis - No monitoring TRIPODI Acute Venous Thromboembolism Epidemiology • • - Incidence 1.6:1000 inhabitants per year Causes Acquired (surgery, cancer, pregnancy, oral contraceptives, etc.) - Congenital (Deficiency of Anticoagulant mechanisms) TRIPODI Acute Venous Thromboembolism Incidence Following: • Surgery - General - Orthopedic - Cancer • Medical diseases • Stroke (affected limb) • Trauma TRIPODI 25% 50-70% 50% 16% 60% >60% Deep Vein Thrombosis (DVT) Rates after Major Orthopedic Surgery in Asia (1) Piovella F et al, JTH 2005 • Aim - To assess the incidence of DVT in patients undergoing major orthopedic surgery of the lower limbs without prophylaxis • Design - Epidemiological study based on postoperative screening with centrally adjudicated bilateral venography TRIPODI Deep Vein Thrombosis (DVT) Rates after Major Orthopedic Surgery in Asia Piovella F et al, JTH 2005 • Participating Centers - 19 across Asia (China, Indonesia, South Korea, Malaysia, Philippines, Taiwan and Thailand) • Results - DVT was diagnosed in 41% (95% CI 35-47%) of the patients • Conclusions - The rate of DVT in the absence of prophylaxis in Asia is similar to that reported in Western countries TRIPODI Settings where the Laboratory can help Clinicians Oral anticoagulant monitoring TRIPODI Oral Anticoagulant Treatment • Optimal level of anticoagulation - To prevent thrombotic recurrences - Still adequate to ensure hemostasis • Laboratory control - To adjust dosage in individual patients TRIPODI Prothrombin Time (PT) Defined as - Clotting time of citrated plasma (or whole blood) upon addition of tissue extract (thromboplastin) and calcium ions Advantages - Simple and cheap - Sensitive to most of the clotting factors depressed by oral anticoagulation (VII, X, II) TRIPODI Prothrombin Time (PT) Main drawback in monitoring oral anticoagulants • Different responsiveness of commercial PT systems to the defect induced by oral anticoagulants • Different ways of expressing results TRIPODI Prothrombin Time (PT) Expression of Results • Coagulation time - Seconds • Percentage activity - Interpolated from a calibration curve • Ratio - Patient-to-normal coagulation time TRIPODI Prothrombin time (PT) Consequences of the Different Responsiveness of PT Systems • Different degree of anticoagulation in different hospital • Difficult establishment of “universal” therapeutic intervals TRIPODI Prothrombin Time (PT) Possible solutions to the different responsiveness of PT systems • To use the same PT system in all laboratories • To calibrate commercial PT systems against an International Standard TRIPODI Log-PT with IS manual technique Calibration of PT Systems ISIWorking system = Slope x ISIIS Log-PT with Working System TRIPODI Hierarchy of WHO Standards 67/40 BCT/253 OBT/79 RBT/90 rTF/95 RBT/05 TRIPODI RBT/79 How to Convert PT into INR PTRatio = PT patients Mean Normal PT ISI INR = (PTRatio) TRIPODI Degree of Anticoagulation and INR Inadequate Adequate Excessive 1 2 3 4 INR TRIPODI 5 6 Implementation of the INR System Responsibility (1) • Manufacturers of thromboplastins - They should provide the ISI for their systems • National control Laboratories - They should check the reliability of the ISI by occasional calibrations and organization of regular external quality control schemes TRIPODI Implementation of the INR System Responsibility (2) • Laboratory workers - They should favor implementation by expressing results for patients on oral anticoagulants as INR and informing clinicians on the INR system • Clinicians - They should use the INR for patients on oral anticoagulants TRIPODI Numbers of Patients on Oral Anticoagulant Treatment • About 1% of the general population in Western countries is on oral anticoagulant treatment - Prevention of venous thromboembolism - Prosthetic cardiac valves - Atrial fibrillation • The current rate of increase is about 10% per year TRIPODI Organization of Oral Anticoagulant Treatment • Established - Anticoagulation clinic - Specialists (cardiologists, hematologists, etc.) • Being Developed (fast growing) - Self-testing - Self-management TRIPODI Anticoagulation Clinics UK, Netherlands and Italy • - Main Task Patient education Laboratory monitoring Clinical monitoring Assistance on the occasion of adverse events - Assistance on the occasion of surgery or other potentially hemorrhagic events TRIPODI Anticoagulation Clinics UK, Netherlands and Italy • • - Personnel Physicians Nurses Medical technologists Equipment Coagulometers Computer software for automated drug prescription TRIPODI Anticoagulation Clinic registration prescription Computer-asssisted dosage Blood sampling TRIPODI Protrombin time (PT)