contact dermatitis
advertisement

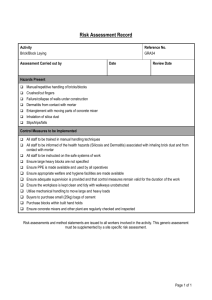
World Allergy Organization December, 2011 Cancun, Mesxico New Horizons Session on Skin Diseases Contact Dermatitis Luz Fonacier MD, FACAAI, FAAAAI Section Head of Allergy Program Director, Allergy and Immunology Winthrop University Hospital Professor of Clinical Medicine SUNY at Stony Brook Long Island, New York Disclosure Research and Educational Grants: • AAAAI ART Grant • Genentech • Dyax • Lev Speaker’s Bureau • Baxter Long Island, New York Objectives WAO Upon completion of this workshop, participants should be able to: 1. Recognize important contact allergens 2. Be familiar with the clinical correlation of the results of the patch test Long Island, New York Dermatitis Contact Allergens of the Year 2011: Dimethyl Fumarate Bruze M, Zimerson E. Dermatitis 2011,Vol 22,No 1 2010: Neomycin Sasseville D. Dermatitis 2010, Vol. 21, No 1 2009: Mixed Dialkyl Thioureas Anderson B, Dermatitis 2009, Vol. 20, No. 1 2008: Nickel 2008 Komik R. Zug K Dermatitis 2008 Vol. 19, No. 1 2007: Fragrance Storrs F. Dermatitis 2007 Vol.28, No. 1 2006: P-Phenylenediamine DeLeo V. Dermatitis 2006 Vol. 17, No. 2 2005: Corticosteroids Isaksson BM. Dermatitis 2005 Vo. 16, No. 1 2004: Cocoamidopropyl Betaine Fowler J. Dermatitis 2004 Vol 15, No.1 2003: Bacitracin Sood A, Taylor J. Dermatitis 2003 Vol 14, No. 1 2002: Thimerosal Belsito D. Dermatitis 2002 Vol.13, No.1 2001: Gold Fowler J Dermatitis 2001 Vol.12, No.1 2000: Disperse Blue Dyes Storrs F Dermatitis 2000 Vol. 11, No. 1 Long Island, New York Dimethyl Fumarate Contact Allergen of 2011 Furniture-Related Dermatitis • Common sites were trunk, limbs, buttocks, face • Blistering, lichenoid, contact urticaria Shoe Related Dermatitis Textile Related Dermatitis Photo from: Bruze M, Zimerson E. Dermatitis 2011,Vol 22,No 1 Long Island, New York Neomycin Contact Allergen of 2010 Fifth most common allergen in NA (ACDS database) Higher rate of sensitization due to availability of antibiotic in OTC: ‘‘triple antibiotic’’ High risk groups: stasis dermatitis, leg ulcers, anogenital dermatitis & otitis externa Long Island, New York Patch Test with Neomycin In T.R.U.E. Test: 20% in petrolatum • False (-) may occur in 10% of cases * • If strongly suspected, ROAT with commercial preparation or PT with 20% aqueous solution Intradermal tests: 1% solution of neomycin Patch-test slow to appear, peaking at day 4 or even at day 7** Similar to gold, (+) reactions may persist for days to weeks *Epstein E. Contact dermatitis to neomycin with false negative patch tests: allergy established by intradermal and usage tests. Contact Dermatitis 1980;6:236–7 **Bjarnason B, Flosado´ ttir E. Patch testing with neomycin sulfate. Contact Dermatitis 2000;43:295–302 Long Island, New York Neomycin Cross Reactivity 90% for paromomycin & butirosin 70% for framycetin 60% for tobramycin & kanamycin 50% for gentamicin 4% for streptomycin Concomitant sensitizations: neomycin and bacitracin Long Island, New York Neomycin in vaccines Vaccines contain 25 mg of neomycin Reactions are minimal, local or transient The Committee on Infectious Diseases of the American Academy of Pediatrics no longer considers contact hypersensitivity to neomycin a contraindication to vaccination Kwittken PL, Rosen S, Sweinberg SK. MMR vaccine and neomycin allergy. Am J Dis Child 1993;147:128–9 Long Island, New York Mixed Dialkyl Thioureas Contact Allergen of 2009 Mixture of diethylthiourea (DETU) & dibutylthiourea (DBTU) Applications and Uses • Adhesive manufacturing • Anticorrosive agents • Paint & glue removers • Pesticides & fungicides • Photocopy paper (diazo copy paper) • Photography, as an antioxidant • Rubber accelerator (especially neoprene) • Synthetic resins • Textile and dye industry 1.1% + PT reaction rate and of highest relevance rate in NACD Anderson B. Mixed Dialkyl Thioureas. Dermatitis 20:1 pp 3-5. 2009 Long Island, New York Nickel: Contact Allergen of 2008 10% of population are nickel allergic Increasing incidence of allergic sensitization to nickel in North America • New sources of nickel ACD: cell phones New insight was offered into the possible genetics of nickel contact allergy Long Island, New York Dietary Nickel Evidence support the contribution of dietary nickel to dermatitis such as vesicular hand eczema Meta-analysis of systemic contact dermatitis following oral exposure to nickel estimated that: • 1% of nickel allergic patients would have systemic reaction to nickel content of a normal diet • 10% would react to 0.55 - 0.89 mg of nickel * Kornik R & Zug K. Dermatitis2008;19(1):3-8 * Jensen CS, Menné T, Johansen JD. Systemic contact dermatitis after oral exposure to nickel: a review with a modified metaanalysis Contact Dermatitis 2006;54:79–86 Long Island, New York Nickel Pyramid >50 mcg Soybean, Boiled ~ 1 cup: 895mcg Cocoa, 1 tbsp: 147 mcg Cashew, ~ 18 nuts:143 mcg Figs ~5: 85 mcg Lentils ½ cup cooked: 61 mcg Raspberry: 56 mcg 20-50 mcg Vegetables, canned½ cup: 40 mcg Lobster 3 oz: 30 mcg Peas Frozen, ½ cup: 27 mcg Asparagus, 6 spears: 25 mcg Oat Flakes 2/3 cup: 25 mcg Pistaccios, 47 nuts: 23 mcg Strawberries, 7 med: 9 mcg Bread wheat, 1 slice: 5 mcg Poultry, 3.5 oz: 5 mcg Carrots, 8 sticks: 5 mcg Apple, 1 med: 5 mcg Cheese 1.5 oz:3 mcg Yogurt, 1 cup:3 mcg Mineral water, 8 fl oz: 3 mcg Mushroom raw, ½ cup: 2 mcg Corn Flakes, 1 cup: 2mcg <20mcg Nickel in Biomedical Devices Reports of dermatitis to biomedical devices lead to: • Consultation requests from orthopedic surgeons & orthodontists regarding safety of permanent or semipermanent metal medical devices in suspected nickel-sensitized patients • High variability of care in terms of testing & recommendations • Increased health care costs • Medicolegal concerns contribute to testing consultations • In some instances of joint replacement, selection of a more expensive & less durable option As nickel allergy incidence increases, this problem also presumably will increase Kornik R and Zug K. Dermatitis2008;19(1):3-8 Long Island, New York METAL IMPLANT “ALLERGY” Often suspected but rarely documented Nickel: 10% of population are nickel allergic • 25% of nickel sensitive patients are also cobalt sensitive 5% of orthopedic implant patients & up to 21% of patients with preoperative metal sensitivity may develop cutaneous allergic reactions upon reexposure to the same metal* Clinical manifestations • Cutaneous – localized – generalized: mostly eczematous (urticaria & vasculitis reported) • Implant Failure Basko-Plluska JL, Thyssen, JP & Schalock PC. Cutaneous &Systemic Hypersensitivity Reactions to Metallic Implants. Dermatitis, 2011. 22;2: 65–79 *Niki Y, Matsumoto H, Otani T, et al. Screening for symptomatic metal sensitivity: a prospective study of 92 patients undergoing total knee arthroplasty. Biomaterials 2006;26:1019–26. Long Island, New York Metals and Alloys Used in Implants Basko-Plluska JL, Thyssen, JP & Schalock PC. Cutaneous &Systemic Hypersensitivity Reactions to Metallic Implants. Dermatitis, 2011. 22;2: 65–79 Long Island, New York Knee replacements Incidence of sensitivity for all types of orthopedic implants is probably < 0.1% • includes static orthopedic implants (higher probability of sensitization than dynamic prostheses) Rare partly because modern knee prostheses are metal-on-plastic, as opposed to metal-on-metal Other components that very rarely cause sensitization • bone cement (methyl methacrylate) • polyethylene (plastic spacer) Merritt K, Rodrigo JJ. Immune response to synthetic materials. Clin Orthop Relat Res 1996;(326):71–9 Long Island, New York Prospective Longitudinal Studies and Reviews Study Total Pts Conclusions Carlsson & Mo¨ller 1989 18 Metal allergic pts with confirmed allergy to one of the metals in their device prior to stainless steel orthopedic implants had no issues (6-yr ff-up) Merritt & Rodrigo1996 22 1% develop cutaneous vs 20–25% develop implant-induced metal sensitivity without any allergic skin manifestations Niki et al, 2006 92 26% of screened pts had (+) lymphocyte stimulation tests to at least one metal (Ni, Co, Cr, Fe). In metal (+) prior to implant, 21% (5/24) developed cutaneous dermatitis at the site of implant;(some widespread dermatitis) 5% of the total study developed cutaneous allergic reactions. Thyssen et al, 2009 356 Risk of surgical revision was not increased in patients with metal allergies Risk of metal allergy was not increased in patients who were operated on, in comparison with controls. Eben et al, 2010 92 66/92 had sx (pain, reduced motion, swelling) Rates of allergy: nickel: 24.2%; cobalt:6.1%; chromium: 3.0% Symptomatic (31.8%) had allergic reaction to bone cement components (gentamicin 23.8%, benzoyl peroxide 10.6%, hydroquinone 4.5%) Sensitization rates in symptom-free patients: 3.8% for nickel, cobalt, chromium; 15.4% for gentamicin Carlsson A, Mo¨ller H. Implantation of orthopaedic devices in patients with metal allergy. Acta Derm Venereol 1989;69:62–6 Merritt K, Rodrigo JJ. Immune response to synthetic materials.Sensitization of patients receiving orthopaedic implants. Clin Orthop 1996;326:71–9.. Niki Y, Matsumoto H, Otani T, et al. Screening for symptomatic metal sensitivity: a prospective study of 92 patients undergoing total knee arthroplasty. Biomaterials 2006;26:1019–26. Thyssen JP, Jakobsen SS, Engkilde K, et al. The association between metal allergy, total hip arthroplasty, and revision. Acta Orthop 2009;80:646–52. Eben R, Dietrich KA, Nerz C, et al. Contact allergy to metals and bone cement components in patients with intolerance of arthroplasty. Dtsch Med Wochenschr 2010;135:1418–22. Long Island, New York Allergic contact dermatitis from bone cement components • Reported in 24.8% of patients (n = 239)* • Orthopedic bone cements composition: • methyl methacrylate (MMA) • N,N-dimethylp- toluidine (DPT) • may be a significant cause of aseptic loosening **7 /15 patients with aseptic loosening of a total hip replacement were DPT allergic • benzoyl peroxide*** • antibiotics (gentamicin, tobramycin, clindamycin, erythromycin)*** *Thomas P, Schuh A, Eben R, et al. Allergy to bone cement components. Orthopa¨de 2008;37:117–20. **Haddad FS, Cobb AG, Bentley G, et al. Hypersensitivity in aseptic loosening of total hip replacements. The role of constituents of bone cement. J Bone Joint Surg Br 1996;78:546–9. *** Kuehn KD, Ege W, Gopp U. Acrylic bone cements: composition and properties. Orthop Clin North Am 2005;36:17–28. Long Island, New York Implant Failure 16 patients with failed metal-on-metal arthroplastic implants; 81% had metal sensitivity (PT &/or lymphocyte transformation test)* Accumulated reports in total hip arthroplasty : • prevalence of metal allergy – ~ 25% in patients with a well-functioning hip arthroplastic implant – ~ 60% among patients with a failed or poorly functioning implant** * Thomas P, Braathen LR, Dorig M, et al. Increased metal allergy in patients with failed metal-on-metal hip arthroplasty and periimplant T-lymphocytic inflammation. Allergy 2009;64:1157–65. ** Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am 2001;83:428–36. Basko-Plluska JL, Thyssen, JP & Schalock PC. Cutaneous &Systemic Hypersensitivity Reactions to Metallic Implants. Dermatitis, 2011. 22;2: 65–79 Long Island, New York Endovascular stenting procedures & in-stent restenosis * Retrospective study of coronary in-stent restenosis 6 mos post stainless steel stent placement & PT 2 months after angioplasty • 11 (+) PT in 10/ 131 (8%) – 7 to nickel & 4 to molybdenum • Clinical history not predictive of a (+) or (-) patch-test result • All 10 with (+) PT to metal had in-stent restenosis (higher frequency of restenosis than in patients with no metal allergy) Conclusion: …suggest that allergy to metals, nickel in particular, plays a relevant role in inflammatory fibroproliferatory restenosis ** Prospective study of 174 stented patients • 109 for initial placement & 65 for in-stent restenosis) • Patients with recurrence of in-stent restenosis had significantly higher (+) PT to metals (nickel & manganese) • No correlation with restenosis after initial stent placement *Köster R, Vieluf D, Kiehn M, et al. Nickel and molybdenum contact allergies in patients with coronary in-stent restenosis Lancet 2000;356:1895–7 **Iijima R, Ikari Y, Amiya E, et al. The impact of metallic allergy on stent implantation: metal allergy & recurrence of in-stent restenosis Int J Cardiol 2005;104:319–25 Long Island, New York Diagnostic Criteria for Metal-Induced Cutaneous Allergic Reactions 1. Chronic eczema beginning weeks or months after the implant 2. Eczema most severe around the implant site 3. Absence of other contact allergens or systemic cause 4. Patch tests positive or strongly positive for one of the metals in the alloy 5. Complete & rapid recovery after total removal of foreign metal implant Merle C, Vigan M, Devred D, et al. Generalized eczema from Vitallium osteosynthesis material. Contact Dermatitis 1992;27:257–8. Long Island, New York METAL IMPLANT “ALLERGY” Conclusions Most reactions to endovascular, cardiovascular, orthopedic, dental metal implants are based on anecdotal case reports or on data from relatively small cohorts • The temporal & physical evidence before and after removal of implants leaves little doubt that a considerable number of patients develop metal sensitivity & cutaneous allergic dermatitis in association with metallic orthopedic implants Conflicting Data: Prospective longitudinal studies are strongly needed • Recent case study showed that ~ 5% developed eczematous reactions directly associated with metallic implants* • Preexisting metal sensitivity with implant containing the offending metal had a higher rate of cutaneous dermatitis • proven cases incriminate nickel, cobalt, chromium, copper Basko-Plluska JL, Thyssen, JP & Schalock PC. Cutaneous &Systemic Hypersensitivity Reactions to Metallic Implants. Dermatitis, 2011. 22;2: 65–79 *Niki Y, Matsumoto H, Otani T, et al. Screening for symptomatic metal sensitivity: a prospective study of 92 patients undergoing total knee arthroplasty. Biomaterials 2006;26:1019–26. **Merritt K, Rodrigo JJ. Immune response to synthetic materials. Sensitization of patients receiving orthopaedic implants. Clin Orthop 1996;326:71–9. Long Island, New York METAL IMPLANT “ALLERGY” Conclusion Need for patch testing is controversial, poorly reliable in predicting or confirming implant reaction • Preimplantation PT: may be considered if suspected of having a strong metal allergy • Post cutaneous eruption (months to years after implant): PT can be done with an appropriate series of metals A negative PT is reassuring for absence of delayed hypersensitivity reaction A positive PT does not prove relevance If relevant allergens are identified and corticosteroid therapy is insufficient to clear the eruption, removal of the implant may be considered Basko-Plluska JL, Thyssen, JP & Schalock PC. Cutaneous &Systemic Hypersensitivity Reactions to Metallic Implants. Dermatitis, 2011. 22;2: 65–79 Long Island, New York Regulating Nickel 1992: Danish Ministry of Environment regulated nickel exposure to products in prolonged contact with the skin • Danish schoolgirls with ears pierced after 1992 regulations had significantly less nickel sensitization compared to those pierced prior to the regulations (5.7% vs 19%) 1994: European Union • limited nickel release threshold from objects in prolonged contact with skin to 0.05 mg/cm2/ week • nickel content of post assemblies (material inserted into pierced parts of the body) to a migration limit of 0.2 mg/cm2/week Laws regulating nickel products, appears to be decreasing sensitization in the younger population Kornik R and Zug K. Dermatitis2008;19(1):3-8 Jensen CS, Lisby S, Baadsgaard O, et al. Decrease in nickel sensitization in a Danish schoolgirl population with ears pierced after implementation of a nickel-exposure regulation Br J Dermatol 2002;146:636–42 Long Island, New York Cosmetics Facial cosmetic dermatitis • Bilateral • Patchy Eyelid Neck • “run-off” pattern • Cosmtics applied to face, scalp or hair often initially affect the neck • Most afftected site of ACVD from nail varnish is the neck Lips Consort/Connubial Dermatitis: primarily fragrance Fragrance Contact Allergen of 2007 > 2800 fragrance ingredients in database of Research Institute for Fragrance Materials, Inc • ~100 are known allergens Complex substances containing hundreds of different chemicals Most common cause of ACD from cosmetic • Patch test 4th in frequency (10.4%) • 1.7-4.1% of general population have + PT to fragrance mix Johansen JD. Fragrance contact allergy: a clinical review. Am J Clin Dermatol 2003;4:789-98 Pratt MD et a;. North American Contact Dermatitis Group Patch-test Results 2001-2002 study period. Dermatitis 2004;15:176-83 *Buckley DA et al. The frequency of fragrance allergy in a patch-test polulation over a 17 year period. Br J Dermatol 2000;142:203-4 Long Island, New York Fragrance Mix Patch test Test Fragrance Mix I Balsam of Peru Myroxylon pereirae NACD 2009-2010 Fragrance Mix II Cinnamic alcohol 1% Cinnamic acid Coumarin 2.5% Cinnamic aldehyde 1% Benzoyl Cinnamate Hydroxyisohexyl 3cyclohexene carboxaldehyde (Lyral) 2.5% a-Amyl cinnamaldehyde (amyl cinnamal) 1% Benzoyl Benzoate Citronellol 0.5% Hydroxycitronellal 1% Benzoic acid Farnesol 2.5% Geraniol 1% Vanillin Citral 1.0% Isoeugenol 1% Nerodilol a Hexyl cinnamic aldehyde 5.0% Eugenol 1% Oak moss 1% Tricky Aspects of Fragrance Allergy New fragrance chemicals are constantly introduced Regulation of fragrance ingredients in cosmetics exempts fragrance formulas as “trade secrets” Some manufacturers do not consider essential oils to be fragrance • Tree tea oil (Melaleuca alternifolia) • Ylang-ylang oil (Cananga odorata) • Jasmine flower oil (Jasminum officinale) • Peppermint oil (Mentha piperita) • Lavander oil (Lavandula angustifolia) • Citrus oil (limonene) “Covert fragrances”- used for purposes other that for aroma (ie preservatives) can be added to “fragrance free” products • Bensaldehyde • Benzyl alcohol • Bisabolol • Citrus oil • Unspecified essential oils Castanedo-Tardan M & Zug K. Patterns of Cosmetic Contact Allergy. Dermatol Clin 2009 27: 265-280 Long Island, New York Balsam of Peru Myroxylon pereirae One of 5 most prevalent allergens in TT Found in toothpaste, mouthwash scents, flavors of food & drinks Cross react with colophony, wood and coal tar, turpentine, resorcinol monobenzoate Systemic CD to certain fruits in patients sensitive to fragrance Long Island, New York Fragrance Leave on fragrances: induce dermatitis at normally utilized concentrations Wash on/wash off products: ? Relevance of brief exposure • Concentration of fragrance left on fabric by laundering was very low & threshold were below induction levels -Contact Dermatitis. 2003 Jun;48(6):310-6. -Contact Dermatitis. 2003 Jun;48(6):324-30. -Contact Dermatitis 2002 Dec;47(6):345-52 -Am J Contact Dermat 1996 Jun;7(2):77-83 Fragrance Systemic Contact Dermatitis Foods to Avoid in Balsam-Restricted Diet • Citrus fruits: oranges, lemons, grapefruit, tangerines, marmalade, juices • Flavoring agents: pastries, bakery goods, candy, chewing gum • Spices: cinnamon, cloves, vanilla, curry, allspice, anise, ginger • Spicy condiments: ketchup, chili sauce, barbecue sauce, chutney, pickles, pizza • Perfumed or flavored tea & tobacco • Chocolate • Certain cough medicines & lozenges • Ice cream • Cola, spiced soft drinks such as Dr Pepper • Tomatoes & tomato-containing products ~ half of patients with positive PT to MP who followed BOP reduction diet had significant improvement of their dermatitis Salam TN, Fowler JF Jr. Balsam-related systemic contact dermatitis J Am Acad Dermatol. 2001 Sep;45(3):377-81 Long Island, New York Summary on Fragrance Allergy Fragrance mix I allergens found in 15- 100% of cosmetic products (especially deodorants) • 2nd - 5th most common (+) PT in series around the world • Testing FM I–allergic patients with ingredients of the mix is successful only about 50% of the time Testing to FM I and BOP picks up 60-70% of fragrance allergic individuals* Many persons have (+) PT to fragrance, but few have clinical allergies to fragrances (allergic contact dermatitis) Storrs F J. Fragrance. Dermatitis Volume 18, Issue 01, March 2007, Pages 3-7 *Larsen W et al. Fragrance contact dermatiis: a worldwide multicenter investigation (part III)> Contact Dermatitis 2002;46:141-4 Long Island, New York P-phenylenediamine (PPD) Contact Allergen of 2006 Permanent Hair Dye • Theoretically, does not cause reaction if fully oxidized • In reality, it is likely that PPD is never completely oxidized • Other reactions: IgE mediated anaphylaxis & lymphomatoid reactions Risk Factors & Ethnic Differences Aging Population • 40% of women in America & Europe color their hair (70% are over 35 y.o.) Black men have higher incidence –use darker shades of dye with higher concentration of PPD Occupational: Currently the most common cause of contact dermatitis in hairdressers Hesse et al. Contact Dermatitis to hair dyes in a Danish Adult population: an interview based study. Br J of Dermatol 2005; 153:132-5 Dickel H et al. Comparison of patch test with standard series among white and black racial groups. Am J Contact Dermat 2001;12:77-82 Long Island, New York New Route of Exposure Body tattooing has increased among the youth of many cultures Use of black henna tattoo (higher PPD than in hair color) Sensitization to PPD from tattoos is likely lifelong • likely see individuals who react to their attempts at hair coloring as they age (reported in 5.3% who never used hair dye) Hesse et al. Contact Dermatitis to hair dyes in a Danish Adult population: an interview based study. Br J of Dermatol 2005; 153:132-5 Dickel H et al. Comparison of patch test with standard series among white and black racial groups. Am J Contact Dermat 2001;12:77-82 De Leo V. p-Phenylenediamine Dermatitis Volume 17, Issue 02, June 2006, Pages 53-55 Long Island, New York Chemicals that may cross react with PPD • • • • • • • • • Product Class Sunscreens Antiinfectives Diuretics Anesthetics Textile dyes Antidiabetic COX-2 inhibitors Rubber Accelerators Black Rubber mix Chemicals PABA & padimate O Sulfonamides & p-aminosalicylic acid Thiazides Benzocaine and related “caines” Azo dyes Sulfonylureas Celecoxib N-isopropyl-N’-phenyl-p-phenylenediamine De Leo V. p-Phephenylenediamine. Dermatitis 2006. 17;2: 53-55 Corticosteroids Contact Allergen of 2005 Increase detection probably due to • Greater awareness • Expanding market for CS • Improved testing procedure Suspect • In stasis ulcers & chronic eczema • When dermatitis fails to respond to CS • When dermatitis worsens with treatment SKIN TESTING TO TOPICAL CORTICOSTEROID * Tixocortol Pivalate (1%) - Class A * Budesonide (0.1%) - Class B&D Hydrocortisone (1%) Hydrocortisone-17-butyrate (0.1%) Betamethasone-17-valerate (0.12%) Clobetasol-17-propionate (0.25%) Prednisolone (1%) * Triamcinolone (0.1%) Patient’s commercial steroid Repeat open application test * Found in current TRUE Test Identifies > 91% of CS allergy Bjarnason et al. Assessment of budesonide patch tests. Contact Dermatitis 1999, 41:211-217 Bofa et al. Screening for corticosteroid contact hypersensitivity. Contact Dermatitis 1995,33: 149-151 Long Island, New York STRUCTURAL GROUPS OF CORTICOSTEROIDS Cross reactivity based on 2 immune recognition sitesC 6/9 & C16/17 substitutions Class A (Hydrocortisone & Tixocortol pivalate: has C17 or C21 short chain ester) Hydrocortisone, -acetate, Tixocortol, Prednisone, Prednisolone, -acetate, Cloprednol, Cortisone, -acetate, Fludrocortisone, Methylprednisolone-acetate Class B (Acetonides: has C16 C17 cis-ketal or –diol additions) Triamcinolone acetonide, -alcohol, Budesonide, Desonide, Fluocinonide, Fluocinolone acetonide, Amcinonide, Halcinonide Class C (non-esterified Betamethasone; C16 methyl group) Betamethasone sodium phosphate, Dexamethasone, Dexamethasone sodium phosphate, Fluocortolone Class D1 (C16 methyl group & halogenated B ring) Clobetasone 17-butyrate, -17-propionate Betamethasone-valerate, dipropionate, Aclometasone dipropionate, Fluocortone caproate, -pivalate, mometasone furoate Class D2 (labile esters w/o C16 methyl nor B ring halogen substitution) Hydrocortisone 17-butyrate ,-17-valerate,-17-aceponate,-17-buteprate, methylprednisolone aceponate Wilkinson SM Corticosteroid cross reactions: an alternative view. Contact dermatitis 2000;42:59-63 Long Island, New York Cocoamidopropyl betaine Contract Allergen of 2004 Second most common allergen in shampoo Amphoteric surfactant often found in shampoos, bath products, eye & facial cleaners Less irritating than are older polar surfactants such as sodium lauryl sulfate but more capable of allergic sensitization. Positive reactions to this allergen are often clinically relevant Shampoos Typically composed of 10-30 ingredients eyelid dermatitis, facial dermatitis, neck dermatitis, scalp dermatitis, dermatitis of the upper back, or dermatitis in more than one of these areas, often leading to difficulty in clinical diagnosis. Of 9 products with no fragrance, 4 had fragrance related potential allergens; 3 of these 4 had botanical ingredients, & 1 had benzyl alcohol Thus, only 5 products in database were truly fragrance free & definitely safe for patients with fragrance allergy. Matthew Zirwas and Jessica Moe Shampoos. Dermatitis, Vol 20, No 2 (March/April), 2009: pp 106–110 Long Island, New York Cocoamidopropyl betaine Typically presents as eyelid, facial, scalp, and/or neck dermatitis • frequent exposure to personal cleansing products • enhanced ability of “sensitive skin” in these areas to develop ACD 3.3% of 975 patients had a + reaction to CAPB (NACDG 2001) Found in >600 personal care products (FDA data voluntarily reported by industry) Commercial bulk production of CAPB may result in contamination of the final product with two chemicals used in the synthesis of CAPB, namely, amidoamine (AA) and dimethylaminopropylamine (DMAPA) Fowler JF. Cocamidopropyl Betaine. Dermatitis 2004;15:3-4 Cosmetic Preservatives • • • • • • Formaldehyde Formaldehyde* Quarternium 15* Diazolidinyl urea* (Germall II) Imidazolidinyl urea* (Germall) Bromonitropropane (Bronopol) DMDM Hydantoin (Glydant) (8.4) (9.3) (3.2) (3.0) • • • • • Non Formaldehyde Methyldibromoglutaronitrile (Euxyl K400) MCI/MI Parabens* Chloroxylenol Iodopropynylbutylcarbamate (5.8) (2.3) (0.5) (0.8) (0.4) (3.3) (2.6) Paraben, quarternium-15 & formaldehyde preservatives are frequently combined & cosensitize *** (% Prevalence PT reaction based on NACDG or TT) *Antigen present in the T.R.U.E. Test ***Albert MR et al. Concomitant positive reactions to allergens in the patch testing standard from 1988-1997. Am J Contact Dermat 1999. 10:219-223 Long Island, New York Formaldehyde Most common potential source of exposure Cosmetics • rarely listed on ingredient label, direct use forbidden in some countries • Contain formaldehyde releasers Permanent press textiles • Increase strength, prevent shrinking, resist wrinkling (permanent press) of cellulose and rayon fibers *Agner et al.Formaldehyde allergy: a follow up study. Am J Contact Dermatitis 1999;10:12-17 Long Island, New York Formaldehyde & Formaldehyde Releasing Preservatives Difficult to avoid because formaldehyde is present in cleaning products, biocides Cross reactivity varies • A high cross-reactivity rate between formaldehyde, Bioban (mixture of 4-(2-nitrobutyl)-morpholine and 4,49-(2-ethyl-2nitrotrimethylene) Dimorpholine), and other formaldehydereleasing agents • Only half of patients with formaldehyde/ FRP allergies reacted to 1-2 allergens and only 1% reacted to all 6** *Anderson B et al Patch-Test Reactions to Formaldehydes, Bioban, and Other Formaldehyde ReleasersDermatitis, Vol 18, No 2 (June), 2007: pp 92–95. **Herbert C, Reitschel RL. Formaldehyde and formaldehyde releasers: how much avoidance of cross reacting agents is required? Contact Dermatiits 2004;50:371-3 Formaldehyde in Textile Resin Reactions: irritant & ACD, exacerbation of AD, urticaria, phototoxic eruptions* • more subacute and chronic dermatitis Testing with formaldehyde alone identifies only ~70% of patients who are allergic to the formaldehyde resins • PT with resins as well Slow resolution of dermatitis even with careful avoidance • As much as 50% still had constant dermatitis * *Hatch KL, Maibach HI. Textile chemical finish dermatitis. Contact Dermatitis 1986;14:1–13. Allergic Contact Dermatitis from Formaldehyde Textile Resins Fowler JF Jr, Skinner SM, Belsito DV. Allergic contact dermatitisfrom formaldehyde resins in permanent press clothing: an underdiagnosed cause of generalized dermatitis. J Am Acad Dermatol .1992;27:962–8. Hilary C. Reich and Erin M. Warshaw Allergic Contact Dermatitis from Formaldehyde Textile Resins . Dermatitis, Vol 21, No 2 (March/April), 2010: pp 65–76 Long Island, New York Key Diagnostic Criteria for Allergic Contact Dermatitis from Formaldehyde Textile Resins 1. Characteristic location of eruption corresponding with contact with clothing 2. Positive PT to formaldehyde 3. Positive PT to suspected fabric 4. Demonstration of free formaldehyde in the suspected fabric 5. Negative reaction to other potential clothing allergens (eg, rubber, nickel, dyes) Reich H & Warshaw E. Allergic Contact Dermatitis from Formaldehyde Textile Resins . Dermatitis. 2010. 21;2:65–76 Long Island, New York Treatment for Textile Finish/ Formaldehyde Resin Allergic Contact Dermatitis Use 100% silk, polyester, acrylic, nylon • Linen & denim are acceptable if soft & wrinkle easily Avoid ‘‘easy care,’’ ‘‘permanent press,’’ or ‘‘wrinkle free’’ Some experts also recommend avoidance of formaldehydereleasing preservatives in personal products* AVOID FORMALDEHYDE RESINS AT ALL TIMES. Even exposure once a month (‘‘Dress clothes’’ only worn on weekends) is enough to maintain your dermatitis Reich H & Warshaw E. Allergic Contact Dermatitis from Formaldehyde Textile Resins . Dermatitis. 2010. 21;2:65–76 *Scheman A, Jacob S, Zirwas M, et al. Contact allergy: alternatives for the 2007 North American Contact Dermatitis Group (NACDG) standard screening tray. Dis Mon 2008;54:7–156. Long Island, New York Quarternium 15 Most common cosmetic preservative allergen Most sensitization is caused by formaldehye releaser Most Quarternium allergic patients are also allergic to formaldehyde Castanedo-Tardan M & Zug K. Patterns of Cosmetic Contact Allergy. Dermatol Clin 2009 27: 265-280 Long Island, New York Paraben Most commonly used ingredient in cosmetic next to water (87-93%) Average total paraben exposure per person in the US is ~ 76 mg/day • Cosmetics & personal products: 50 mg per day – Current concentrations of paraben are generally < 0.3% • Drugs: 25 mg per day • Food: 1 mg per day – paraben in foods is usually less than 1% Parabens are weak sensitizers in cosmetics Paraben-sensitive individuals often tolerate paraben-containing cosmetics on normal intact skin but not damaged skin “Paraben paradox”: only sites of healed dermatitis flare when sensitizer is applied Allison CL, Warshaw EM. Parabens: A Review of Epidemiology, Structure, Allergenicity, and Hormonal Properties. Dermatitis 2005; 16:57-66 Castanedo-Tardan M & Zug K. Patterns of Cosmetic Contact Allergy. Dermatol Clin 2009 27: 265-280 Dermatitis of the Eyelid Eyelids particularly sensitive • thickness (0.55 mm) compared to other facial areas (~2 mm ) • substances applied to scalp or face easily come into contact with the eyelids • substances on fingers can also be a source of palpebral eczematous dermatitis • airborne pollen and dust usually cause such powerful palpebral reactions that any absence of eyelid involvement automatically excludes a diagnosis based on airborne pollen and dust * Ayala F et al. Eyelid Dermatitis: An Evaluation of 447 Patients. Dermatitis 2003;14:069-074 * Sher M. Contact dermatitis of the eyelids. S Afr Med J 1979;55:511–513. (PubMed) Long Island, New York Dermatitis of the Eyelid Allergic contact dermatitis: 55-63.5% 13.4% Fragrance / Balsam of Peru 8.2% 6.0% Gold sodium thiosulfate Nickel sulfate Irritant contact dermatitis: Atopic dermatitis: Seborrheic dermatitis: 15% < 10% 4% Ayala F et al. Eyelid Dermatitis: An Evaluation of 447 Patients. Dermatitis 2003;14:069-074 Reitschel RL et al. Common contact allergens associated with Eyelid dermatitis: data from the NACDG 2003-2004 study period. Dermatitis 2007; 18:78-81 Long Island, New York Dermatitis of the Eyelid Eyelid dermatitis as only site 13.4% Perfume 7.1% Fragrance Mix 6.3% Balsam of Peru 8.2% Gold sodium thiosulfate (most common allergen in pure Mixed facial & eyelid dermatitis* Nickel Kathon Fragrance eyelid dermatitis. 6.0% 3.3% 3.0% 2.2% 1.9% Nickel sulfate Neomycin Methyldibromoglutaronitrile, Quarternium 15 Methylchloroisothiaxolinone Cobalt Cl, DMDM hydantoin, Amidoamine, Cocamidopropyl amine, Thiuram mix, 1.5% Bacitracin, Cinnamic aldehyde, Tosylamide formaldehyde resin, Propylene glycol, Tixocortol pivalate Of 268 cases, 33 showed relevant reactions to an allergen not in the 65 NACDG standard screening allergens *Valsecchi et al. Eyelid Dermatitis: an evaluation of 150 patients. Contact Dermatitis.1992;27:143-7 Reitschel RL et al. Common contact allergens associated with Eyelid dermatitis: data from the NACDG 2003-2004 study period. Dermatitis 2007; 18:78-81 Gold Contact Allergen of 2001 9.5% of 4,101 patch-test were (+) to gold Most common sites: • Hands 29.6% • Face 19.3% – Common in head & neck with seborrheic distribution • Eyelids 7.5% Most common uses: • Wear it: Fashion appeal • Drink it: Anti-inflammatory medication • Smile with it: Dental appliance • Eat it: Dessert contain 5 g of 24-carat gold) Fonacier L, Dreskin S, Leung DL. “Allergic Skin Diseases”. 2010 Primer on Allergic and Immunologic Diseases , 6th Edition. The Journal of Allergy and Clinical Immunology. Volume 125, Issue 2, Supplement 2 (February 2010) S 138-149 Ehrlich A, Belsito DV. Allergic contact dermatitis to Gold. Cutis 2000;65:323-6 Fowler et al. Gold allergy in North America. Am J Contact dermat 2001;12:3-5 McKenna KE et al. Contact allergy to gold sodium thiosulfate. Contact Dermatitis 1995;32:143-6 Long Island, New York Gold Oral symptoms: + Patch test may be clinically relevant in patients with gold dental appliance • Increased rate if dental gold has been present for >10 yrs • Late reacting allergen: >50% + gold test was delayed (1 week) Facial dermatitis: subset of patients clear with gold avoidance • women with titanium dioxide in cosmetics that adsorbs gold released from hand jewelry or eyeglass frames Eyelid dermatitis: 7 of 15 gold allergic patients cleared by not wearing gold jewelry Ehrlich A, Belsito DV. Allergic contact dermatitis to Gold. Cutis 2000;65:323-6 Fowler et al. Gold allergy in North America. Am J Contact Dermat 2001;12:3-5 Koch P & Balmer F. Oral lesions and symptoms related to metals in dental restorations. A clinical, allergological and histological study. J Am Acad Dermatol 1999;41;422-430 Nedorost S, Wagman, A. Positive Patch-Test Reactions to Gold: Patients' Perception of Relevance and the Role of Titanium Dioxide in Cosmetics. Dermatitis 2005;16:67-70 Long Island, New York Gold Trial of gold avoidance may be warranted if with + PT to gold • Avoidance period required for benefit is long and may only be partial • Avoidance of gold earrings did not benefit patients with earlobe dermatitis ie no correlation between gold earring use and earlobe dermatitis • Subset of gold-allergic patients with facial dermatitis who wore powder, eye shadow, or foundation on affected areas did clear with total avoidance of gold jewelry on the hands and wrists Ehrlich A, Belsito DV. Allergic contact dermatitis to Gold. Cutis 2000;65:323-6 Fowler et al. Gold allergy in North America. Am J Contact Dermat 2001;12:3-5 Koch P & Balmer F. Oral lesions and symptoms related to metals in dental restorations. A clinical, allergological and histological study. J Am Acad Dermatol 1999;41;422-430 Nedorost S, Wagman, A. Positive Patch-Test Reactions to Gold: Patients' Perception of Relevance and the Role of Titanium Dioxide in Cosmetics. Dermatitis 2005;16:67-70 Long Island, New York Dermatitis with Scattered Generalized Distribution Difficult diagnostic and therapeutic challenge: lacks the characteristic distribution that gives a clue to the etiology NACDG data: ~ 15% of the patients patch tested only had scattered generalized dermatitis • 49% had a positive patch test deemed at least possibly relevant to their dermatitis • The prevalence was higher in patients with a history of atopic dermatitis • Two most common allergens: – Nickel – Balsam of Peru Zug KA, Rietschel RL, Warshaw EM, et al. The value of patch testing patients with a scattered generalized distribution of dermatitis: Retrospective cross-sectional analyses of North American Contact Dermatitis Group data, 2001 to 2004. J Am Acad Dermatol 2008;59:426-431 Long Island, New York TREATMENT OF CONTACT DERMATITIS Identify and avoid contact with allergens and irritants • Give exposure list (synonyms & sources) Alternatives & substitutions if possible – Cover nickel plated objects – Wash formaldehyde containing garments – Gloves & barriers Supportive care: antihistamines Topical corticosteroids Oral corticosteroids Other modalities: UV light TREATMENT OF CONTACT DERMATITIS Prior to PT, may provide patient with “Lo.C.A.L. (Low contact allergen) Skin Diet (Zug KA); eliminates most common allergens Products devoid of • Fragrance • Formaldehyde Releasing Preservatives • MCI/MI • MDG/PE • Lanolin • CAPB • Benzophenone-3 Long Island, New York TREATMENT OF CONTACT DERMATITIS Acute Contact Dermatitis (wet, oozing lesions) • Aluminum sulfate & calcium acetate (Domeboro) in clean absorbent cloth 20-30 min as compress 2-3 x a day • or Oatmeal baths (Aveeno) in extensive areas • Oral corticosteroid if severe • Fluourinated steroids for 1-2 weeks Chronic contact dermatitis • Emollients to decrease itching • Low to medium strength topical cs • Antihistamines to decrease itching • UV light • Cyclosporine • Topical calcineurin inhibitors Long Island, New York