Mobile Telemedicine Systems System.Pdf
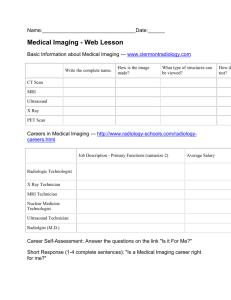
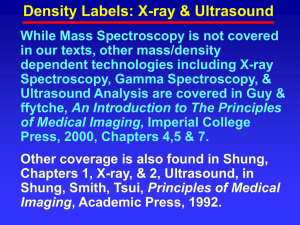
advertisement

Dr. David Hareva Medical Informatics ITT Telkom, 24 September 2011 What is Telemedicine & Teleradiology? Teleradiology Medicine Clinical Genomics Medical Informatics Biomedical Informatics Telemedicine Telemedicine informatics Genomics Communications Bioinformatics Telematics Informatics Definition of Telemedicine Telemedicine may be defined as the use of electronic information and telecommunications technologies to support long-distance clinical healthcare, patient and professional health-related education, public health and health administration. Nihal FG and Elif DU. Theory and Applications of Telemedicine. Journal of Medical Systems, Vol. 26, No. 3, June 2002 Specialties in telemedicine Specialties that use telemedicine often use a 'tele-' prefix; Fix line, wireless, microwave, Tele Tele-radiology satellite, mobile network. Security Communication Tele-cardiology + Modalities of Medical Imaging Tele-psychiatry (X-Ray, Ultrasound, CT, MRI, etc) and Radiology Data acquisition. Tele-pharmacy + etc DICOM and PACS Informatics Image Processing/Analysis Image compressing What is Teleradiology? Teleradiology is the transmission of radiologic images from a site of image acquisition to a remote location for interpretation. Today, image transmission depends primarily on highspeed electronic communication networks, such as an ATM or the internet, which enable the rapid transmission of digital images without loss of content or resolution. Why is teleradioogy necessary? Teleradiology provides a means to provide rapid diagnosis and report turnaround for radiological examinations acquired locally or transmitted to a radiologist from anywhere in the world. At Hospital for Special Surgery (HSS), teleradiology has been employed to provide improved and timely care to patients imaged at a hospital, as well as to provide our radiology subspecialty expertise in orthopaedic and rheumatologic conditions. Through teleradiology services the musculoskeletal imaging and diagnosis can be network with orthopaedic centers or expanded worldwide with other hospitals in the world to maximize the diagnostic information needed to treat their patients. With the constant improvement of digital imaging modalities, the role of teleradiology will continue to expand in the future, enabling expert diagnostic interpretation by HSS radiologists around the globe or around the corner. How is teleradiology performed? The interpretation of digital images, whether MRI, CT, ultrasound or conventional x-ray images, acquired digitally e.g. computed radiography (CR) or direct radiography (DR), is accomplished utilizing workstations with highresolution monitors. Each workstation is part of an image management network, which also has access to image archives and patient databases. Current computer software innovations provide the capacity to transmit and receive images from outside a medical facility while maintaining image security and patient confidentiality. Modalities of image acquisition Computed Tomography (CT) Radiographic (X-ray) Ultrasound Magnetic Resonance Imaging (MRI) Nuclear Medicine Imaging (NMI) etc Radiographic (X-ray) Function: It is a painless test used by medical professionals to help diagnose and treat a wide range of medical problems. Feature: An X-ray uses electromagnetic radiation (shorter wavelength) to take photo like images of different areas of the human body. X-rays, demonstrate body structures proportionally with their density , bone (high body tissue density) which is white and fat(low density) which is gray or air (no density) which is black. Benefits: X-ray is the fastest and easiest way to assess sprains, torn muscles and broken bones. Computer Tomographic (CT) Function: It good for bone spine and joints abnormalities (abdomen, pelvis or head), bony structures, joints, soft tissue structures, and soft tissue calcifications. Feature: A type of x-ray examination using a thin x-ray beam with a series of detectors that are contained in a doughnut shaped machine. Benefits: still digital x-rays with multiple shots without movement or noise disturbances. Cons: cost involved with digital x-ray is twice x-ray film. Some CT examinations will require an injection of an iodinated contrast agent into your vein. Magnetic Resonance Imaging (MRI) Function: MRI scans can be used to diagnose tumors, strokes and torn ligaments. Many MRIs are done on the head to determine the cause of headaches, nervous system problems or developmental disorders of the brain. Feature: MRI is a diagnostic test that depicts both soft tissue and bone. MRI depicts soft tissue injury and abnormalities with greater sensitivity and specificity than x-ray even CT. Benefits: MRI scans are better than Xrays at showing soft tissue, showing inflammation, detailing blood vessels and creating cross-sectional pictures. In addition, the patient is not subjected to any radiation. Ultrasound (sonography) Function: The ultrasound waves enable things inside the body to be measured, such as fetuses, gallstones, kidney stones, cysts or other growths. Features: The probe sends out sound waves, and receives their echos. The sonographic scanner, which interprets the echos to determine the size, shape, depth and what the internal object is made of (fluid, solid). Benefits: non-invasive and non-radiation tool for diagnostics. An ultrasound is able to capture more information about soft tissue than an x-ray scan, though it has trouble with harder tissue such as bone. Ultrasounds are also readily available, and less expensive than other diagnostic or treatment options. 3D/4D ultrasound Nuclear Medicine Imaging (NMI) Function: a bone scan, lung scan, cancer scan, gallium scan or Indium III WBC scan Features: A nuclear medicine examination relies on specific radioactive isotopes to detect specific suspected pathology. Nuclear materials called radiopharmaceuticals are either injected, ingested or inhaled. They travel through the body and cause the organs to release gamma rays. These rays illuminate the organs or bones, and make them easily observable by a special gamma camera. Benefits: This exam is used mainly to allow evaluation of organs and regions within organs that cannot be seen or tested on conventional X-Ray images. Digital mammography Function: the early detection of breast cancer, typically through detection of characteristic masses and / or microcalcifications. Feature: is the process of using low-energy-X-rays (usually around 30 kVp) to examine the human breast and is used as a diagnostic and a screening tool. Benefits: low radiation. Most doctors believe that mammography reduces deaths from breast cancer, although a minority do not. X-Ray/ CT Ultrasound Nuclear (+) excellent (–) no, (+) except for heart (+) growing (+) extensive use cardiac in heart applications (+) widely used (+) excellent (+) excellent, (–) problems with gas Merge w/ CT (+) minor role (+) widely used (–) bleeding, trauma (–) poor (+) PET (+) standard Chest (+) widely used Abdomen Head Cardiovascu(+) X-ray lar Skeletal / Muscular (+) strong for skeletal system (+) real-time, (+) Excellent, (+) functional non-invasive, with (-) catheterinformation on cheap, (–) but, injected contrast perfusion poorer images (+) strong for skeletal system MR (+) getting better High resolution Myocardium viability (–) not used (+) Research in (+) functional (-) (+) excellent elastography bone marrow How are plain film (standard radiograph) images captured? Standard radiographs can be digitized by either a video camera or a film scanner. Video cameras (commonly referred to as a "camera on a stick") were in fact the method of digitizing any image for transmission as recently as about 15 years ago. Typical camera systems utilize a light box designed to illuminate radiographs, an extension arm for holding the camera above the film, and a high-sensitivity video camera with a zoom lens. This is an inexpensive but poor-quality method of image acquisition. Film scanners and digitizers arrived on the teleradiology scene about 10 years ago. There are two basic types of film scanners: CCD (charge coupled device) digitizers and laser digitizers. Over the past few years, and today high quality CCD digitizers produce images as good as (or nearly as good as) top-of-the-line laser digitizers. The major difference between images produced with laser digitizers and CCD digitizers is in the optical density captured from the film. DICOM and PACS DICOM (Digital Imaging and Communications in Medicine) is a standard for handling, storing, printing, and transmitting (TCP/IP) information in medical imaging. It consists of a number of attributes, including items such as name, ID, etc., and also one special attribute containing the image pixel data. Pixel data can be compressed using a variety of standards, including JPEG, JPEG Lossless, JPEG 2000, and Runlength encoding (RLE). DICOM enables the integration of scanners, servers, workstations, printers, and network hardware from multiple manufacturers into a picture archiving and communication system (PACS). PACS typically comprised of an image acquisition device, data management system, image storage devices, local or wide area network, display stations, and devices to produce hard-copy images. DICOM format: size and transmission Medical Image Processing Medical image processing that produces from modalities allows physicians to view the inside of the human body for clinical purposes or medical sciences. Medical image processing techniques can yield more detailed and easily manipulated images. This allows for a more in-depth review of the internal organs and structures of the human body. Medical Image processing Cancer in the posterior right breast on digital mammography. All images courtesy of Maxine Jochelson, MD. Enhancement after contrast. Same view on MRI. Medical Image Processing Structure of digital images Improvement of image quality Enhancement of abnormal lesions Determination of image features of abnormal lesions Image Analysis Image analysis involves manipulating the image data to determine exactly the information necessary to help solve a computer imaging problem. It can be divided into three primary stages: Preprocessing: It is used to remove noise and eliminate irrelevant, visually unnecessary information. Data Reduction: It involves either reducing the data in the spatial domain or transforming it into another domain called the frequency domain and then extracting features for the analysis process. Feature Analysis: In this the features extracted by the data reduction process are examined and evaluated for their use in the application. After the analysis we have a feedback loop that provides for an application-specific review of the analysis results. Input Image Preprocessing Transform Segmentation Filtering Feature extraction Feature Analysis Image Compression Image compression involves reducing the size of image data files, while retaining necessary information. The resulting file is called the compressed file and is used to reconstruct the image, resulting in the decompressed image. It consists of two parts: Compressor: It consists of a preprocessing stage and encoding stage. The first stage in preprocessing is data reduction. For example, the image data can be reduced by gray level and/or spatial quantization. The second step in preprocessing is the mapping process, which maps the original image data in to another mathematical space, where it is easier to compress the data. Next, as part of the encoding process, is the quantization stage, which takes the potentially continuous data from the mapping stage and puts it in discrete form. The final stage of encoding involves the coding the resulting data, which maps the discrete data from the quantizer onto a code in an optimal manner. Decompressor: In this the decoding process is divided into two stages. First, it takes the compressed file and reverses the original coding by mapping the codes to the original, quantized values.Next, these values are processed by a stage that performs an inverse mapping to reverse the original mapping process. Finally, the image may be postprocessed to enhance the look of the final image. Compressor- System Model Decompressor- System Model Open source software for medical image analysis ImageJ 3D Slicer ITK OsiriX GemIdent MicroDicom FreeSurfer ClearCanvas Seg3D [2] NumPy + SciPy + MayaVi/Visvis InVesalius ImageJ ImageJ can display, edit, analyze, process, save, and print 8-bit, 16-bit and 32bit images. It can read many image formats including TIFF, PNG, GIF, JPEG, BMP, DICOM, FITS, as well as raw formats. ImageJ supports image stacks, a series of images that share a single window, and it is multithreaded, so time-consuming operations can be performed in parallel on multi-CPU hardware. ImageJ can calculate area and pixel value statistics of user-defined selections and intensity thresholded objects. It can measure distances and angles. It can create density histograms and line profile plots. It supports standard image processing functions such as logical and arithmetical operations between images, contrast manipulation, convolution, Fourier analysis, sharpening, smoothing, edge detection and median filtering. It does geometric transformations such as scaling, rotation and flips. The program supports any number of images simultaneously, limited only by available memory. CVIPTools Image Analysis Segmentation & Morphological Filtering Fourier Transform Histogram Features Image Restoration Image Enhancement Image Compression Fix line and satellite technologies PSTN (public switched telephone network): Telkom, Indosat ISDN (integrated service digital network) Satellite Connection Wireless Technology Microwave Connection Leased line ATM (asynchronous transfer mode) Cellular Technology: CDMA, GSM Barrier to Telemedicine Physician/Patient Acceptance Funding/ Reimbursement Issues Convenience Legal Availability of Technology at a Reasonable Cost Privacy and Security Concerns Application 1: Medical Imaging centered on Mobile phone The World Health Organization (WHO) has reported that about 75% of the world's population is without access to ultrasounds, X-rays, magnetic resonance images, and other medical imaging technology that can detect tumors, diagnose tuberculosis infections, and monitor pregnant women. Around 95% of medical technology in developing countries is imported“. More than 50% of the medical equipment in developing countries is left unused or broken because it is too complicated or expensive to operate and repair, ….” The combined components of medical imaging devices (data acquisition hardware, image processing software, and a display device) into a solitary unit, causes the cost is substantially increased. Boris Rubinsky. A New Concept for Medical Imaging Centered on Cellular Phone Technology. Hebrew University of Jerusalem, April 30, 2008. Application 1, Cont ... Conventional stand-alone medical imaging device, image reconstruction, control and transmit processed images from the patient site. A new medical imaging system made of two independent components connected through cellular phone technology. The independent units are: a data acquisition device (DAD) at a remote patient site that is simple, with limited controls and no image display capability and an advanced image reconstruction and hardware control multi-server unit at a central site. the breast cancer tumors patient self-test screening Frequency-Division Multiplexing EIT, Seven AC currents (at different frequencies) are injected simultaneously. Signals from voltage electrodes (V1 to V8) are connected to an analogue multiplexer Application 2: Ultrasound imaging with a smartphone William D. Richard, Ph.D at Washington University coupling USB-based ultrasound probe technology with a Windows mobilebased smartphones, $100,000 grant by Microsoft awarded in 2008. It is possible to ultrasound probes for imaging the kidney, liver, bladder and eyes, endocavity probes for prostate and uterine screenings and biopsies, and vascular probes for imaging veins and arteries for starting IVs and central lines. http://news.wustl.edu/news/Pages/13928.aspx, April 20, 2009 Application 3: A Viewing and manipulated Medical Image on Smartphone A: A remote physician is equiped with iOAS. ResolutionMD is visualization server and picture archiving and communication system (PACS) is connected. B.1: secure http connection, B.2: user select an image for interpretation. D.1: This produce a touch event, D.2: which is sesnt into visualization server, D.3: interaction event causes a new rendered frame, D.4: that display on iOS device. E: User exits the iOS application. (+) no patient data is located outside the firewall; the large data can be viewed and manipulated on iOS without using its memory. C.1: load patient exam into memory, C.2: reformat 2D into 3D JPEG compression, C.3: This frame is sent to iOAS appl, C.4: display it on iOS device. J Ross Mitchel . A Smartphone Client-Server Teleradiology System for Primary Diagnosis of Acute Stroke. J Med Internet Res 2011;13(2):e31. http://www.jmir.org/2011/2/e31/ Satellite Teleradiology In a poster presentation at the 2003 Symposium for Computer Applications in Radiology (SCAR), Dr. Lance Williams of Womack Army Medical Center (WAMC) at Fort Bragg, NC, detailed a telemedicine solution the Army used to provide radiology coverage both in Bosnia and at WAMC. Running Researches Analisis metode perbaikan citra untuk mengidentifikasi kanker pada hasil mamografi menggunakan adaptive contrast enhancement II. Optimalisasi sistem pemantauan gizi menggunakan perangkat mobile dengan algoritma genetika dalam kasus diabetes. Kemungkinan smartphone untuk pengolahan gambar medis Pengolahan citra irisan mata menggunakan mobile phone. Etc. Thank you