Presentation heading - Pharmacy Management National Forum
advertisement

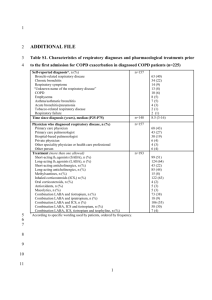
Virtual clinics in COPD and high dose ICS step down Dr Azhar Saleem GP Respiratory Lead, Lambeth CCG GP Lead London Procurement Partnership GP and Lung co-lead TOHETI, Guys & St Thomas’ Hospital www.toheti.org Oct 2015 Disclosures for Dr Azhar Saleem I never do promotional speaking Research Support/P.I. No relevant conflicts of interest to declare Employee No relevant conflicts of interest to declare Consultant No relevant conflicts of interest to declare Major Stockholder No relevant conflicts of interest to declare Speakers Bureau No relevant conflicts of interest to declare Honoraria TEVA, Pfizer Scientific Advisory Board No relevant conflicts of interest to declare What the difference between COPD and True Love? COPD lasts forever NHS best in the world Worst crisis in 20 years? Value based interventions APPROPRIATE Health outcomes True Value = Cost + COST OF WASTE Value based pyramid WISDOM STUDY • 2485 patients with moderate to severe COPD with exacerbations • Randomised after 6 week run in to either ICS continuation or stepwise withdrawal to dual bronchodilatation with LAMA/LABA (tio/salm) over 52 weeks • Mean FEV1 34% Mean mMRC 1.8 • Primary end point – time to first moderate or severe COPD exacerbation • Magnussen H et al. NEJM Sept 2014 DOI: 10.1056/NEJMoa1407154 WISDOM STUDY RESULTS • 2027 patients completed study • No difference in exacerbation rate between 2 groups (HR 1.06 CI 0.94-1.19) • At week 18, ICS group had 38ml greater trough FEV1 (p<0.001) and week 52 - 43 ml (p<0.001) • Slight difference in SGRQ at weeks 52 in favour of ICS continuation (1.22 difference p=0.047) • CONCLUSION • Many patients with severe to very severe COPD and exacerbations may not benefit from addition of ICS on top of LAMA+LABA Evidence from UK White P et al. PLoS One. 2013 Oct 23;8(10):e75221. doi: 10.1371/journal.pone.0075221. eCollection 2013. Applying medicines optimisation principles • 35% of patients on COPD registers did not have spirometry consistent with this diagnosis Principle 1 : Understanding the patient experience • 38% of patients were receiving inhaled corticosteroid (ICS) therapy outside national guidance • lack of focus on high value interventions like quit smoking support and pulmonary rehabilitation Patrick White et al, 2013. 41 London general practices (population 310,775) - Population 366,574 - Densely populated and ethnically diverse borough - 48 General Practices - 3 Locality Care Networks - North Lambeth (95,816) - SE Lambeth (113,701) - SW Lambeth (157,054) Lambeth & Southwark IRT Pulmonary rehabilitation SECONDARY CARE Chest clinic Integrated Respiratory Team Oxygen assessment & review Virtual clinics PRIMARY CARE Tier 3 smoking cessation Advanced lung function One referral form IRT Structure Respiratory physio team GSTT GSTT Chest clinic GP Lambeth Respiratory nurses GSTT & KCH Respiratory physio team KCH 50% SECONDARY CARE Consultant Chest Physician KCH Chest clinic 50% PRIMARY CARE Respiratory pharmacist GP Southwark The joint MO and IRT plan • COPD: Review of Inhaled Corticosteroid in mild & moderate • Asthma: Step down clinics for pts on high dose ICS (at step 4) • Metric. Reduction in high dose ICS as a % of all ICS items What is a virtual clinic? Virtual clinics Virtual Clinics – a model for change • Delivered in GP practice by an integrated respiratory consultant and/or respiratory pharmacist or GP respiratory lead. Principle 4: Making medicines optimisatio n part of routine practice • 2-hour structured sessions for practice clinicians to discuss optimal patient management on a case by case basis. • Pre-work – searches and templates • Follow up – sustainability (GP/nurse actions) and patient engagement in the plan; ideally within 2 weeks. 19 Why Virtual Clinics ? • Information alone doesn’t change behaviour • Asthma and COPD registers are currently quite inaccurate for many different reasons • Diagnostic spirometry is not performed well in primary care • COPD is often incorrectly staged and there are ‘false’ Asthma diagnoses • Respiratory prescribing is often poorly understood 20 21 22 23 VCs - Typical changes • Many patients on high dose LABA/ICS but not on a LAMA • Many patients had not had PR or smoking cessation prior to being on high dose ICS • Many patients on high dose ICS with FEV1 % predicted above 50% • Some patients on high dose ICS didn’t even meet diagnostic criteria for Asthma or COPD • Poor understanding between different devices and doses of equivalent steroid eg Accuhaler vs Evohaler 24 Evaluation of an ICS withdrawal programme in patients with Mild/Mod COPD in Lambeth CCG Grainne d’Ancona, National Institute of Health Research (NIHR) Irem Patel, Consultant Respiratory Physician, KCH Dr Azhar Saleem, GP Respiratory Lead, Lambeth CCG Cathrine McKenzie, Consultant Pharmacist, GSTT Vanessa Burgess, Chief Pharmacist Lambeth CCG Tariq Sethi, Head of Respiratory Medicine, KCH 26 Lambeth CCG ICS stepwise withdrawal programme • Feasibility study in one CCG (48 practices) • withdrawal by GP upon recommendation by the multidisciplinary Integrated Respiratory Team in a virtual clinic • 370 patients with FEV1 >50% reviewed – 320 had COPD • 2/3 patients had a change in medicines recommended • Of these, 76% to gradually stop or step down ICS dose • 60% attempted (95% patient acceptance) Lambeth ICS prescribing Percentage high-dose ICS prescribing (of all ICS) 34% 2012-13 2013-14 2014-15 33% 32% 31% 30% 29% 28% Launch of Respiratory Virtual Clinics 27% 26% 25% 24% Q1 2012- Q2 2012- Q3 2012- Q4 2012- Q1 2013- Q2 2013- Q3 2013- Q4 2013- Q1 2014- Q2 2014- Q3 201413 13 13 13 14 14 14 14 15 15 15 Lambeth ICS prescribing pattern 17% reduction in high dose ICS Tiotropium items, Lambeth CCG 3,400 Tiotropium Items 3,300 3,200 3,100 3,000 2,900 2,800 Tiotropium Items 2,700 2,600 2,500 2,400 1st Quarter 2013/2014 2nd Quarter 2013/2014 3rd Quarter 2013/2014 4th Quarter 2013/2014 1st Quarter 2014/2015 2nd Quarter 2014/2015 3rd Quarter 2014/2015 30 PR referrals increased by 40% 1000 Pulmonary Rehabilitation – referrals 900 800 700 600 GP Referrals, Lambeth CCG 500 400 All referrals incl hospital referrals 300 200 100 0 Total referrals for 2012 1st & 2nd Q’s 2013 3rd & 4th Q’s 2013 Total Referrals for 2013 31 Lambeth ICS prescribing Q2 2014/2015 Q2 2013/2014 Admissions data • Between 2011/12 and 2013/14 COPD admissions in Southwark decreased by 6%, saving £37,016 and £43,926 per year. Lambeth has shown a smaller impact to date. • From 2011/12 to 2013/14 neither borough had an increase in COPD admissions attributable to the ICS “step down. 33 It can be done! ! What now? • Lambeth and Southwark CCG are now targeting Asthma with the high quality Asthma pyramid • Lambeth and Southwark have developed two algorithms for use by primary care to work up patients presenting with breathlessness and cough. • London Procurement Partnership in conjunction with UKMI and the ABPI are developing an NHS digital inhaler resource to be free at the point of use for all NHS HCPs and to be editorially managed and control by the NHS The high quality asthma pyramid Key SABA = short-acting B-agonist ICS = Inhaled Corticosteroid QST = Quit Smoking Treatment PAAP = asthma action plan VBA = Very Brief Advice (smoking cessation) The reality of how it’ll look Key SABA = short-acting B-agonist ICS = Inhaled Corticosteroid QST = Quit Smoking Treatment PAAP = asthma action plan VBA = Very Brief Advice (smoking cessation) Breathlessness Algorithm Cardiac Respiratory Mental Illness /Addiction Fitness/Lifestyle Anaemia/Kidney disease Breathlessness Algorithm NHS Lambeth Clinical Commissioning Group NHS Southwark Clinical Commissioning Group NHS Lambeth Clinical Commissioning Group NHS Southwark Clinical Commissioning Group ( STEP(4(((( ((Tier(2(Investigations(for(presentation(of(chronic(breathlessness Only(order(tests(if(you(would(act(upon(the(results. Common(Causes(of( Breathlessness( Further(Examinations/Tests( · · Possible(Diagnoses/Reasons( for(Breathlessness( · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · Feeling'Breathless'Guide'for'Patients’' ( STEP(5(( ( · · · · · · · Consider(Contributing(Factors(to(Breathlessness( Order(each(of(the(possible(contributory(factors(for(the(chronic(breathlessness · · ( ( ·