Audit and Inspection in Clinical Trial
advertisement

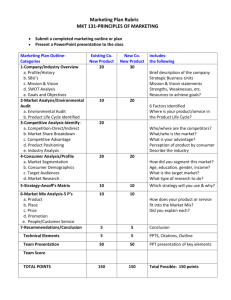
WHAT IS AUDIT PURPOSE OF AUDIT WHAT IS INSPECTION DIFFERENCES BETWEEN AUDIT AND INSPECTION WHO IS RESPONSIBLE FOR AUDIT AND INSPECTION TYPES OF AUDIT AND INSPECTION REASON FOR AUDIT AND INSPECTION WHEN AND WHAT GET AUDITED AUDIT PROCEDURES RULE PREPRATION FOR AUDIT MULTIPLE CHOICE QUESTION A Systematic and independent examination of trial related activities and documents to determine whether the evaluated trial related activities were conducted and • the data were recorded, analyzed and accurately reported according to the Protocol, sponsor sop’s, GCP, and Applicable regulatory requirements. • (ICH-GCP Sec. 1.6) The purpose of a sponsor’s audit is to evaluate the trial conduct and compliance with:• Quality Systems and SOPs • Protocol • Good clinical practices & other applicable regulatory requirements Auditors are independent of the clinical trial/ data collection system(s) Sponsor or CRO or Site Organization and personnel Responsibilities and functions - Ensure clear responsibilities exist so as to minimize ambiguity between: Investigator and sub-investigator Sponsors and contractors Contractors/suppliers (CROs, Labs, IRBs) – audit suppliers! Qualification, training and adequacy of staff List of monitors List of all investigators What to audit (Cont…) Quality management systems Management responsibilities Procedures and their adequacy Training Documentation control Change control Deviations and non conformities management QC, QA Internal Monitoring Program Internal Auditing Program What to audit (Cont…) Investigational drug Manufacturing, packaging, labeling and coding of the investigational product (including placebo and active comparator where applicable) in accordance with applicable GMP standards Labeling requirements, “For Clinical Trial Use Only” to protect blinding where applicable Drug Product Accountability Control Quantity IRB/EC › › › › Responsibilities Composition, functions and operations Procedures Records Investigators and sub-investigators › Qualifications and agreements Essential documents Essential documents: › Investigator’s brochure Has all current info been provided to the investigator? › Signed protocol and amendments › › › › How are changes and deviations to the protocol handled? Advertisements for subject recruitment Informed consent forms Approved by IRB/IEC? All been signed off according to requirements? Financial aspects of the trial Approved by IRB/IEC? Insurance statement (where required) What to audit (Cont…) Essential Document : • • • • • • • • • • • Subject Databank Subject screening log Subject identification code list Subject Enrollment log Case report forms Documentation of CRF corrections Serious adverse events reporting Signature sheet Signed agreements between parties IRB/IEC approval/favorable opinion IRB/IEC composition Essential Document : Regulatory authorities authorization/approval/ notification of the protocol Normal value(s)/ranges for medical/laboratory tests Certifications or accreditation of labs (or other means that establishes competency of lab) What to audit (Cont…) Essential Document : At the clinical site:- investigational product and trial related materials Instructions for handling Shipping records Certificates of analysis of product shipped Accountability at the trial site Decoding procedures for blinded trials Master randomization list and method What to audit (Cont…) Essential Document : Records of retained body fluids/tissue samples (if any) Monitoring visit reports • Pre trial • During trial • Post trial Final report by investigatory Clinical study report Archiving What to audit (Cont…) Bio-analytical Laboratories : Documentation control including archiving Qualification of instruments Qualifications and Training of staff Bio-analytical method validation Receipt and storage of samples Handling of reagents and solution Testing conducted as outlined in protocol CFR 11 compliance What to audit (Cont…) Computerized systems (used to create, modify, maintain, archive, retrieve or transmit data): Identify software and hardware used, when and where? Check security of the system (individual Login, secure passwords) Check traceability Check audit trail capabilities where applicable:• • • Who made the changes? When and Why, Certification of changes by appropriate authorities Check validation status where applicable Check record retention capabilities What to audit (Cont…) Computerized systems (used to create, modify, maintain, archive, retrieve or transmit data) : Adequate procedures that need to be in place:• • • • • • • • System setup/installation Data collection and handling System maintenance Data backup, recovery and contingency plans Security Change control Alternative recording methods Personnel training What to audit (Cont…) Statistical component: Check statistical procedures and methods used are according to protocol Check statistical package used has been validated Review statistical analysis and results Check integrity of data and timely locking of database “The act by a regulatory of conducting and official review of documents, facilities, records, and any other resources that are deemed by the authority to be related to the clinical trial and that may be located at the • • • Site of the trial, Sponsor’s and/or CRO’s facilities, Other establishments deemed appropriate by the regulatory authority” (ICH-GCP Sec 1.29) FDA Office Site Location 1. Select Site 4. Arrive (482) 2. Contact Site 5. Review Records 3. Schedule Site 6. Interview Staff 9. Write Report (EIR) 7. Present Findings 10. Classify Inspection 8. Depart (483) A summary report of inspectional observations. It is a list of objectionable conditions or practices observed during the inspection, prepared by the FDA investigator and presented to the auditee at the conclusion of an inspection. AUDIT INSPECTION Inspectors are employed of the company who work for a active clinical quality assurance (CQA) function (i.e. Sponsor/CRO) Inspector are employed by government, through the agency of the regulatory or competent Authority (i.e. FDA/DCGI) To ensure that a site is complying with Protocol, SOP, GCP and Applicable regulatory requirements. To ensure that trial related obligations and acceptability of resultant clinical data is in support of a new drug approval. The following entities have rights to conduct the Audit/Inspection at site based on regulation • • • • • FDA/CDSCO OHRP: ( Department of health and Human Services) The Sponsor of the clinical trial CRO/ Cooperative Groups/Grant-Funded Research IRBs and Institutions In connection with a clinical study, An Audit/inspection may be undertaken if there are - Concerns about its safety, data or ethics - Monitor standards of clinical research - When there is suspicion of fraud or scientific misconduct - When there is serious quality systems breakdown Routine: For-Cause: To ensure that a site is complying with Protocol, SOP, GCP and Applicable regulatory requirements. This is referred as “ROUTINE AUDIT” If the site is out of compliance and the sponsors want to either verify the problem or be reassured that no problem exists. This is referred as “FOR-CAUSE AUDIT” “Study-oriented Audit” “Investigator – oriented Audit” • FDA: To evaluate data supporting a new drug or device application • Sponsor: To verify site data and conduct To verify how the study was monitored • In-house (CRO): To evaluate quality of research ongoing at the institution. To Justify placing a grant Continuous Funding To Verify data • Cooperative Groups/Grant Funded Research: Done by FDA / Sponsor/In-house (CRO)/ IRB Cause: 1. 2. 3. 4. Allegation/Suspicion of non-compliance. Safety or efficacy data is inconsistent with other study sites. PI conducting research outside area of specialty. Accrual is abnormally high for geographical or ethnicity/race location. At anytime during the study After the study is completed prior to regulatory approval for the product At any time after regulatory approval (15 years) if a safety concern with the product (rare) 5 Categories : 1. 2. 3. 4. 5. Regulatory and protocol compliance Subject Records Investigational Product Adverse events, SAEs or complications Documentation Study oriented audits Investigator oriented audits Patient Enrollment: Highest It generally occur when the drug regulatory authority has cause to suspect particular research’s conduct i.e. “For-cause Audit enrolling sites Patient Retention: Large number of screen failures, unusually high patient drop-out rates Adverse Events: Large number of severe adverse events at only one or two sites Trial Importance: Pivotal studies. 3 to 5 minutes rule : To provide documents requested by Inspector If not available be truthful Beyond five minutes inspector may assume that it has been fabricated Documentation thumb rule: If not documented means not done If documented does not mean that it is done Do not provide or copy these information for FDA/Auditor: Financial data (salary information, budgets) (except financial disclosure of clinical investigators) Personnel data (performance appraisals) (except qualifications [job descriptions] and training records) Remember 3-5 minute rule Pre Audit Procedure During Audit Procedure After Audit Procedure 1) CRC Preparation: Notify all staff involved in study about the audit with date, time & duration of the audit. Ensure the Investigator’s attendance during the Audit. Reservation/Arrangement for quiet, comfortable place to work and to assemble the necessary documents for Auditor Defined SOP/Agenda should be present and properly reviewed by all staff involved in trial before audit about interaction of auditor with site, from his welcome to exit 1) CRC Preparation (Continue): Assemble all study documents in one place, they should be complete and well organized Assure accessible photocopier, provide a backup if necessary (to provide document when requested by them) Confirm / Verify about the CRA’s presence during the Audit and Review all the essential documents or any other problem which is found during this review so that the situation may be able to be remedied before audit 2) CRA’s Preparation: Review and verification of every essential document should be complete and properly placed Ensure resolution of unresolved queries before audit Notify confirmation of audit agenda to site for conduct of audit at selected site 3) Auditor’s Preparation: Auditor should have Audit plan/Agenda Auditor may also prepare working documents for use during audit, sometimes it becomes necessary to generate Auditspecific working Notify conduct of audit to CRA and Site Auditors present their credentials (photo ID) & a Notice of Inspections (Form 482) to the Clinical Investigator Conduct Introductory Meeting Auditor will start auditing by reviewing specific data related to trial study and regulatory requirements. They will document all their findings Auditor also interview site staff directly involved in trial activities and process Auditor’ s common observations for study: 1. Protocol Non-adherence 2. Inadequate & inaccurate records 3. Failure to report adverse events 4. Failure to report concomitant therapy 5. Inadequate drug accountability 6. IRB/IEC problems 7. Informed Consent issues Closing meeting (exit interview): At site visit completion, Auditor conducts “exit interview” with all responsible site personnel to: Review findings Clarify misunderstandings Describe any deviations from current regulations Suggest corrective action, if appropriate Auditor (FDA) may issue a Form FDA 483 (Notice of Observation) to the Investigator. This form will detail the findings from the audit that may constitute compliance violation After the Audit is complete, the Auditor prepares an: Audit certificate: A declaration of confirmation by the auditor that an audit has taken place. Audit report / Establishment Inspection Report (EIR): A written evaluation by the sponsor's auditor of the results of the audit • EIR Classification: Inspector should present a Form FDA 482 “Notice of Inspection.” Have all subject records organized and available. Give the inspected only those records specifically requested. Make scrupulous notes of comments/concerns/ deficiencies pointed out by the inspected Question entries in the inspector’s notes regarding adverse findings. Clarify or attempt to resolve issues as they are made known. (remember 3-5 rule) If the questions seems vague, ask for clarification before answering. Make sure the inspection understands your response. Be courteous, professional and available. Do’s (Cont…) Object to requests for unreasonable information (e.g. Financial records and Home addresses of subjects). In this case, the investigator may ask for a written request from the FDA Let the sponsor know of the outcome as soon as possible Answer- Politely, co-operate, understanding them factfully, without speculation or guess work Do not give more information than asked for. Do not offer to change data unless it can be verified with the sponsor and supported by source documents. Do not discuss other studies. Do not discuss financial arrangement between you and sponsor Do Not (cont…) Do not hide information or volunteer information Do not sign affidavits. Do not allow pictures Do not leave the inspector alone Do not initial/sign any errors. Compliance is Organizational responsibility & mandatory act Compliance is not a individual responsibility Integrity as a culture Document properly what you do Do not document what you do not do Do it right at for the first time, at right time, in right manner