Clonal Evolution in CLL: Impact on Timing of Therapy
advertisement

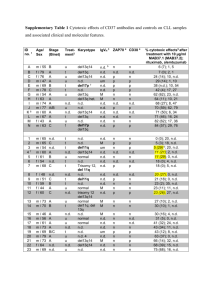
Clonal Evolution in CLL: Impact on timing of therapy Nicholas Chiorazzi The Feinstein Institute for Medical Research North Shore – LIJ Health System Manhasset, NY Three principles relevant for a discussion of clonal evolution At all points in time, CLL clones are heterogeneous based on a number of criteria CLL worsens as subclones exhibiting new or different DNA mutations and hence biology emerge over time – “clonal evolution” The occurrence of new structural abnormalities in the DNA of leukemic subclones requires that new strands of DNA be made, i.e., for cells to divide and proliferate Intra-clonal heterogeneity All CLL clones are heterogeneous based on: Surface membrane and intracellular phenotypes CD38 – Damle et al. Blood 1999; Ghia et al. Blood 2003 ZAP-70 – Rassenti et al. N Engl J Med 2005 CD49d – Gattei et al. Blood 2008 Telomere length and telomerase activity Bechter et al. Cancer Res 1998 Damle et al. Blood 2004 Roos et al. Blood 2008 Survival and growth requirements Pepper et al. Leukemia 2006 Ongoing IGHV mutations Gurrieri et al. J Exp Med 2002 Volkheimer et al. Blood 2007 Sutton et al. Blood 2009 Chromosomal and specific gene differences Shanafelt et al. J Clin Oncol 2006 Landau et al. Leukemia 2013 Time since birth/last replication – “Age” Calissano et al. Mol Med 2011 Evolution and growth in our understanding of CLL heterogeneity over time Gruber and Wu. Semin Hematol 51:177-187, 2014 Evidence for clonal evolution occurring in CLL A. Sequential analyses of: Karyotype and FISH abnormalities Shanafelt et al. J Clin Oncol 2006 Global DNA abnormalities by comparative genomic hybridization and SNP profiling Grubor et al. Blood 113: 1294-1303, 2009 Braggio, Kay et al. Leukemia 2102 B. Analyses of DNA abnormalities by next generation sequencing of CLL genomes/exomes Clonal evolution A. Sequential analyses of FISH abnormalities, microRNA abnormalities, and global DNA abnormalities ~25% of patients develop a new genetic abnormality over time in coding or non-coding genes Occurs more frequently in: Most common new lesions: U-CLL clones and in M-CLL clones of patients that eventually require therapy CD38+ clones ZAP-70+ clones CD49d+ clones del(13q) del(17p) – harbinger of accelerated disease Greater the number of clonal aberrations the shorter the time to treatment and survival Karyotype evolution and survival Shanafelt et al. J Cin Oncol;26:e5-e6, 2008 The greater the genomic complexity, the shorter progression-free survival (CGH) Kay et al. Cancer Genet Cytogenet 203:161-8, 2010 Evidence for clonal evolution occurring in CLL A. Sequential analyses of: FISH abnormalities Shanafelt et al. J Clin Oncol 2006 Global DNA abnormalities by comparative genomic hybridization and SNP profiling Braggio, Kay et al. Leukemia 2102 B. Analyses of DNA abnormalities by next generation sequencing of CLL exomes and genomes Clonal evolution in CLL B. Analyses of DNA abnormalities by next generation sequencing of CLL exomes and genomes Initial studies in 2011: Puente et al. Nature 475: 101-105, 2011 Fabbri et al. J Exp Med 208: 1389-1401, 2011 Wang et al. N Engl J Med 365: 2497-2506, 2011 Since then a number of additional and more intricate studies: Quesada et al. Nat Genet 44: 47–52, 2012 Schuh et al. Blood 120, 4191–4196, 2012 Landau et al. Cell 152: 714–726, 2013 Summary of consistent findings B. Analyses of DNA abnormalities by next generation sequencing of CLL exomes and genomes Genomic complexity exists in CLL of a degree less than that of solid tumors and DLCBL; similar to AML Over 20 recurrent mutations were identified. Most common abnormality is in NOTCH1 Specific mutations associate with at least 7 biological pathways Mutations appear to fall into two categories: initiating clonal driver mutations and secondary, subclonal mutations Subclonal mutations often emerge after therapy but many/most exist prior to therapy Significantly mutated genes and associated pathways Landau et al. Cell 152, 714–726, 2013 Associations between specific gene mutations and other characteristics Wang et al. N Engl J Med 365: 2497-2506, 2011 Genetic Evolution and Clonal Heterogeneity Result in Altered Clinical Outcome Genetic evolution and clonal heterogeneity result in altered clinical outcome Landau et al. Cell 152, 714–726, 2013 Frequency of genetic alterations in CLL, early and later in disease progression Gruber and Wu. Semin Hematol 51:177-187, 2014 A model for the stepwise evolution of CLL Landau et al. Cell 152, 714– 726, 2013 Clonal evolution in CLL C. Acquisition of therapy resistance as a consequence of clonal evolution Example: resistance to ibrutinib treatment Woyach et al. N Engl J Med 370: 2286-2294, 2014 Furman et al. N Engl J Med 370: 2352-2354, 2014 Effect of C481S mutation of BTK on ibrutinib binding and the ability of ibrutinib to inhibit BTK phosphorylation Furman et al. N Engl J Med 370: 2352-2354, 2014 Functional characterization of PLCγ2 with the R665W and L845F mutations Woyach et al. N Engl J Med 370: 2286-2294, 2014 A model for the stepwise evolution of CLL Landau et al. Cell 152, 714– 726, 2013 Background All CLL clones are heterogeneous based on: Surface membrane and intracellular phenotypes Telomere length and telomerase activity Survival and growth requirements Ongoing IGHV mutations Chromosomal and specific gene abnormalities Time since last replication – “Age” Calissano et al. Mol Med 2011 This type of heterogeneity is not “fixed” and “mutant” but is “dynamic” and “physiologic ” Deuterated (“heavy”) water - 2H2O 2H O 2 DNA Hydrogen Deuterium In vivo “pulse-chase” study CLL cells DNA Gas chromatography/ Mass spectrometry What can these studies tell us? Birth and death/elimination rates of CLL clones Messmer et al. J Clin Invest 115: 755, 2005 van Gent et al. Cancer Res 68: 10137, 2008 deFoiche et al. Br J Haematol: 143: 240, 2008 Means to indirectly identify cells that have most recently been born/divided in patients Calissano et al. Blood 114: 4832-4842, 2009 Calissano et al. Mol Med 17: 1374-82, 2011 Cell fractions with more cells with 2H-labeled DNA contain the most recently replicated/born cells Deuterium content of fractions sorted based on reciprocal densities of CXCR4 and CD5 CXCR4brightCD5dim CXCR4 CXCR4intCD5int CXCR4dimCD5bright CD5 Gas chromatography/ Mass spectrometry The CXCR4dimCD5brite fraction is significantly enriched in cells with 2H-labelled DNA CXCR4dim CD5bright: “DIM” (proliferative) 30 PROL INT/BULK REST CXCR4bright CD5dim: “BR” (resting) 2H CXCR4int CD5int : “INT” (tumor bulk) enrichments in DNA 20 10 0 0 21 Days 42 % Ki-67 positive cells The CXCR4dimCD5brite fraction is significantly enriched in cells expressing Ki-67 P<0.01 4.5 4.0 3.5 3.0 2.5 2.0 CXCR4 br CD5 dim CXCR4 int CD5 int CXCR4 dim CD5 br N=13 1.5 1.0 0.5 0.0 CXCR4 br CD5 dim CXCR4 int CD5 int CXCR4 dim CD5 Ki67 G0 G1 S G2 M br Intraclonal heterogeneity – time since birth/replication Resting, re-entry compartment Blood CD38 Life Death Bulk CD38 BCR CLL CXCR4 CD5 CLL CXCR4 CD5 BCR CD38 Solid Tissue Re-initiate or survive/rest CD38 CD38 CLL CD5 SDF-1 CXCR4 Release BCR (CXCL12) CXCR4 BCR CD38 CLL Stromal cell Nurse like cell CD5 BCR CD38 CXCR4 BCR signaling TLR signaling CLL BCR CD5 CD5 Blood CLL CXCR4 CLL Exit CXCR4 BCR Proliferative compartment CD5 Why should we care about the “proliferative fraction” if it represents only ~1% of a CLL clone? CLL patients progress to more severe disease when members of the clone develop new DNA mutations over time – “clonal evolution” Permanent new DNA mutations can only occur when new strands of DNA are made, as cells divide and proliferate Hence, the “proliferative fraction” contains potentially very dangerous CLL cells since they just replicated their DNA What is the “mutational process” that can induce somatic point mutations and DNA deletions as causes of ongoing genomic lesions in CLL? Is the “mutational process” more active in the proliferative fraction of CLL cells? Activation-induced cytidine deaminase (AID) 1. Essential and sufficient to initiate DNA point mutations that lead to repair with different nucleotides during a germinal center reaction. 2. Essential and sufficient to initiate DNA deletions that are an intimate component of IGH class switch recombination, although other elements are required to repair the break points and seal off the deletion 3. Shown to have “off target activity” (i.e., mutate or delete outside the IGV locus) in a wide range of both hematological and non-hematological cancers -AID can act as an oncogenic enzyme AID mRNA is enriched in the peripheral blood proliferative fraction Sort Strategy: CXCR4 Proliferative fraction CD5 CXCR4 CD23 Resting fraction CD5 AID PCR FOR AID Beta Actin Patten et al. Blood 120:4802, 2012 AID protein expression is inducible in peripheral blood CLL co-cultures AID+ t= 0 hrs t= 72 hrs cells<1% + Cells Clear: CD5+AID CD19 + cells 27% Tinted: CD19 Cells t= 168 hrs AID+ cells 65% Stimulation strategy: CLL PBMCS cultured with murine fibroblasts (L cells) plus anti-CD40 and IL-4 CD23 Composite RPA AID x630 Patten et al. Blood 120:4802, 2012 AID protein is expressed primarily in dividing cells UNSTIMULATED STIMULATED PBMCs with L cells PBMCs with L-cells plus anti-CD40 and IL-4 0.1% 0.1% 75% 0.1% AID: Blue IMC: Red CD5+CD19+ cells D7 culture No Division CD5+CD19+ cells D7 culture Multiple Divisions Is this inducible AID functional? • Confocal assay for the presence of double strand DNA breaks within cell nuclei – Anti-phospho-histone H2A.X staining (pH2A.X) • Evidence of immunoglobulin class switching • Appearance of new mutations in IGHV/D/J transcripts by single cell PCR Increased double strand DNA breaks are seen in divided CLL cells: anti-pH2A.X staining Stimulated Cells: D14 of culture x630 CD23 pH2A.X CD23:Red (DSBs) CFSE All CFSE All Unstimulated Cells: D14 of culture x630 CD23 pH2A.X (DSBs) CD23:Red Increased double strand breaks are seen in divided CLL cells: anti-pH2A.X staining % Stimulated cells expressing pH2A.X greater than unstimulated cells AID expression by stimulated cells CFSE % of cells AID IMC CD5+CD19+ Cells CFSE (Log Scale) n=3 Is this inducible AID functional? • Confocal assay for the presence of double strand breaks within cell nuclei – Anti-phospho-histone H2A.X staining (pH2AX) • Evidence of immunoglobulin class switching • Appearance of new mutations in IGHV/D/J transcripts by single cell PCR Immunoglobulin class switching CD5+CD19+ Cells Sort 2 populations: UNDIVIDED or MULTIPLY DIVIDED FSC-A STIMULATION: for up to 14 days 20 cell aliquots CFSE UNSWITCHED: m transcripts SWITCHED: transcripts (a transcripts) Sequencing: analysis only on clone specific V-D-J RT PCR with clone specific VH and CH primers Patten et al. Blood 120:4802, 2012 Divided cells contain Ig class switched transcripts Percentage % Positive wells for switched transcripts Wells without switched transcripts Wells with switched transcripts Divided 113 22 Undivided 89 1 Unstimulated 45 0 p=0.0002 (n=3) Surface IgG expression increases with cell division CD5+CD19+ Cells CLL1299 FSC-A % IgG expression vs division CFSE CD19 1% IgG Undivided <0.1% CD19 Multiply Divided IgG Is this inducible AID functional? • Confocal assay for the presence of double strand breaks within cell nuclei – Anti-phospho-histone H2A.X staining (pH2AX) • Evidence of immunoglobulin class switching • Appearance of new mutations in IGHV/D/J transcripts by single cell PCR Mutations in IGHV/D/J genes • Sorted single cells: same strategy as for class switch analysis • High fidelity reverse transcriptase and polymerase • The experimental ERROR RATE following both steps: – less than 6 x 10-6 per base pair No of mutations per 104 base pairs Mutations in IGHVDJ rearrangements CLL1278: UNMUTATED IGHV CLL1082: MUTATED IGHV Lymph node CLL cells can express AID protein Red-CD23;Blue-Ki67;Green-AID 10 Cases: 5 demonstrate scattered AID+cells x630 AID+ cells are Ki-67+; many Ki-67+ cells are AIDDAB staining anti-AID x100 Patten et al. Blood 120:4802, 2012 Lymph node: flow cytometry AID + Blocking Peptide CD5 93% AID 0.02% AID Alone 1.2% CD19 MFI AID+ Cells MFI All CD5+CD19+ Cells % Greater in all CD5+CD19+ Cells % Greater in AID+ Cells of surface markers for the proliferative and resting CLL phenotypes Does AID expression correlate with clinical course in patients? AID+ CLL patients correlate with increased numbers of cytogenetic aberrations and worse clinical outcomes P = 0.02 P = 0.001 P = 0.001 P = 0.02 P = NS P = NS P = 0.001 P = 0.001 Patten et al. Blood 120:4802, 2012 Summary All CLL clones are heterogeneous at all points in time This heterogeneity can be genetic/fixed or physiologic/dynamic Those clonal submembers that divide are more likely to upregulate AID and therefore develop new genetic changes The degree of intraclonal genetic heterogeneity correlates with CLL disease progression and shorter time-to-treatment and length of survival Over time, and especially with therapy, these intraclonal genetic variants can outcompete the initial major clonal submembers – Clonal Evolution