Infection Prevention Surveillance in Home Care
advertisement

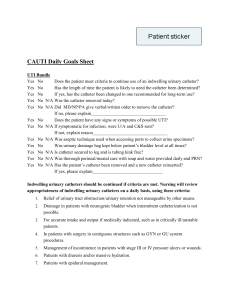
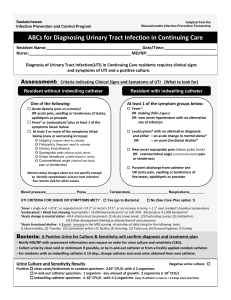
Carole Yeung, RN CIC Nothing to disclose Surveillance (in general) HAI Surveillance Practical Application ◦ CAUTI Reduction Discuss methods for identifying potential infections using OASIS and applying the APIC-HICPAC Surveillance Definitions for HHC and Home Hospice Infections Describe the use of surveillance to improve outcome and process measures Analyze and report findings of the surveillance data including the development of action plans The hospice must maintain and document an effective infection control program that protects patients, families and hospice personnel by preventing and controlling infections and communicable diseases A plan for the appropriate actions that are expected to result in improvement and disease prevention Current: ◦ No requirement for agency wide program ◦ Must comply with accepted professional standards & principles that include infection prevention Proposed: ◦ Maintain and document a program to prevent and control infections & communicable disease ◦ Follow accepted standards, including standard precautions, and educate staff, patients, and caregivers about proper infection control procedures Surveillance is defined as “the ongoing, systematic collection, analysis, interpretation and evaluation of health data closely integrated with the timely dissemination of this data to those who need it”. (Centers for Disease Control and Prevention. CDC surveillance update. Atlanta: Centers for Disease Control and Prevention, 1988) Essential component of an infection prevention & control program to reduce frequency of adverse events Comprehensive method of measuring outcomes and other processes of care Systematic methods of collecting, consolidating and analyzing data concerning distribution & determinants of a given disease or event Dissemination of information to those who can improve outcomes Outbreak investigation/Performance Improvement No “single” or right method Based on population served , services provided, & regulatory or other requirements (Infection Prevention Risk Assessment) Requires direct involvement of organization leaders Team work and collaboration across the healthcare spectrum are important in the development of surveillance plans Designed in accordance with current recommended practices and defined elements Incorporate into Safety & PI Programs Written plan serves as the foundation and should outline important objectives and elements: ◦ HAI ◦ Non HAI (community) ◦ Non infectious disease events Multidisciplinary team Identify areas of risk and potential impact on patients, staff, and agency. Identify risks based on: ◦ Geographic location, community, and population served ◦ Care, treatment, or services provided Evaluate each potential risk in each of the three categories of probability, impact, and current systems. http://www.apicdfw.org/seminar/2008/lee1.pdf Terrie Lee adapted for BHHHN Measure outcomes and processes Monitor a variety of outcomes/processes Monitor high-risk/high-volume events Cost/negative impact Mandates to monitor specific indicators Determine time period for observation CLABSI (Central line associated blood stream infections) CAUTI (Catheter associated urinary tract infections) Skin and soft tissue infections Flu vaccination rates (patients and hcw) Sharp injuries in HCW Include community (if applicable) Adherence to published standards/best practices (hand hygiene, infectious disease precautions) Training and competence of care provided by family/care givers Evaluation of specific infection prevention and control measures (home care bag checks) Best practices for invasive device infection prevention Outcome: ◦ Catheter Associated Urinary Tract Infection Reduction by 10% Process: ◦ Assure best practices are being followed for care of a patient with an indwelling catheter Goals (broad statements) Objectives (specific and measurable) Strategies (steps to take to achieve goals) Evaluation (how you will measure your achievement of objectives) Progress (current measure and next steps) Standard definitions to ensure precise surveillance (preferably published) Definitions should be consistently used in the collection, analysis, and reporting of surveillance data When to collect data? ◦ Concurrent ◦ Retrospective Who will collect the data? Where to find data? How to collect data? Unique to the organization Specific to surveillance plan Learn from colleagues, reports in the literature Collect data from a variety of sources ◦ ◦ ◦ ◦ ◦ Clinicians OASIS Data Medical Records (paper, electronic) Lab reports Direct Observation Data Collection Form ◦ Identify data elements to be collected ◦ Limit data collection to elements that are needed to identify a case or determine the case criteria are met for condition or event being studied Data must be analyzed, interpreted, and reported Expressed in numerical measurement of the outcome/process observed Essential that appropriate calculations be performed and reported with a consistency of methodology over time for interpretation of each surveillance component Data can be non useful if numerator too small or denominator of inappropriate size Rates accurately calculated? Major changes from previous data Substantially high rates ◦ May signify a problem ◦ Investigate risk factors/processes ◦ No obvious observation Design a report Federal, state, and local authorities Referring or receiving facilities Systemic ongoing process ◦ Tables, graphs, charts, and summary graph ◦ Disseminate to managers and healthcare providers who can use the findings to improve performance ◦ Healthcare workers ◦ Supervisors/Managers Goals: ◦ Enhance safety and quality of patient care ◦ Reductions in: Morbidity and mortality Emergent care Acute care hospitalizations Cost Purpose: ◦ Assess the safety and quality of patient care by establishing a baseline and monitoring trends ◦ Use findings to improve care to prevent infections and other complications ◦ Detect & investigate clusters or outbreaks (including community) ◦ Assess effectiveness of prevention & control measures ◦ Ensure regulatory compliance Do not routinely include identification of community-acquired infections Report infections to other facilities May be useful to: ◦ Know patients with MDRO’s in the agency and notify patient infectious status to another agency/facility if patient is transferred ◦ Assure appropriate precautions Describing an infection to the agency does not mean that they caused it. The following can increase the risk of infection: ◦ Certain conditions or therapies place pts at increased risk ◦ Other elements not directly associated with a persons healthcare status can increase the risk ◦ Environmental factors ◦ Agent factor Not intended to be used to make clinical decisions or to determine treatment Consultation with hospital IP may be beneficial APIC-HICPAC Surveillance Definitions for Home Health Care & Home Hospice Infections, 2008 Surveillance Form Clinicians reporting Case Conferences Local hospitals Networking with local IP’s OASIS data • Designated person to review the evidence to determine if definition for HAI is met M2300. Since last time OASIS data collected has the patient utilized the Emergency Department: 0 No 1 Yes, use hospital ED without hospital admit 2 Yes, use hospital ED with hospital admit UK M2310 Reason for Emergent Care Time Point M2300 & M2310: ◦ Transfer to inpatient facility, with or without agency discharge ◦ Discharge from agency M2430 Reason for Hospitalization Time Point: ◦ Transfer to inpatient facility, with or without agency discharge M2310 and M2430 3 – Respiratory Infection 13 – UTI 14 – IV catheter-related infection or complication 15 – Wound infection/deterioration M1600: has this patient been treated for a UTI in last 14 days 0 - No 1 - Yes NA - Patient on prophylactic antibiotics UK – Unknown Time Points: ◦ SOC/ROC ◦ DC from the agency – not to inpatient facility Internal: ◦ agency historical data External: ◦ Must use same case findings ◦ Must use same case definitions IPRA – CAUTI 2009 rate: 0.9 CAUTI/1,000 catheter days Goal: Reduce CAUTI in patients with indwelling catheters Objective: Reduce CAUTI by 20% next 2 years. (Decrease antibiotic use. Decrease MDRO acquisitions) Improvement strategies: ◦ Review the literature – best practices ◦ Update procedures as necessary ◦ Monitor patients with indwelling catheter during supervisor visits including hand hygiene ◦ Education – all disciplines Evaluation/Progress: Quarterly report to Administration Team and healthcare workers Must meet one of the following criteria and had an indwelling catheter within the last 7 days: 1. Two of the following signs/symptoms: ◦ ◦ ◦ ◦ Fever or chills Flank pain, suprapubic pain, tenderness, frequency, urgency Worsening mental/functional status Changes in urine character AND urinalysis or culture not done 2. One of the following two signs or symptoms: ◦ Fever or chills ◦ Flank pain, suprapubic pain, tenderness, frequency, urgency AND ◦ Bacteria (positive culture or nitrite)and pyuria (>10 wbc/hpf or leukocytes) on urinalysis (APIC-HICPAC Surveillance Definitions for Home Health Care and Home Hospice Infections, 2008) Potential for subjectivity: 48hrs vs 72 hrs after admission to HC Changes in urine character? What constitutes a potential pathogen? Colony count? Why is worsening of mental or functional status not included in criteria 2? ◦ Why 7 days after catheter discontinued? ◦ ◦ ◦ ◦ ◦ Need for more “concrete” criteria if HHC Clinicians reporting Case Conferences OASIS data M2310 and M2430 13 – UTI OASIS data M1600 (treatment of a UTI in the last 14 days) Source: BHHHN - LR 43 Indwelling urinary catheter days vs patient days (do not include suprapubic) ◦ Clinicians reporting ◦ Computer profiles Clinicians document Develop a report (may need IT help) 6 CAUTI 2,132 Catheter Days X 1,000 = 2.8 CAUTI/1,000 catheter days Sterile technique for insertion Consider using smallest bore catheter as possible (14–16fr with a 5cc balloon) Discourage irrigation Urinary Catheter Maintenance Patient/caregiver education S/S infection Specimen collection/transportation Catheter removal Develop check sheet Assess care when perform home visits: ◦ Skilled nurses ◦ Supervisory Visits ◦ AIDES Compliant Catheter connected to closed drainage system Urinary catheter is secure to prevent movement Drainage bag below level of the bladder Family has education sheet Non Compliant N/A 1 Hand hygiene before patient contact or putting on gloves Hand hygiene after patient contact or removing gloves Hand hygiene before reaching into home care bag 2 3 4 5 6 7 Total % Formal – Education days ◦ SN ◦ Therapy and AIDES Informal – Case conferences Best Practices 1.2 Supervisor check list 1 0.8 Education 0.6 0.4 0.2 0 Jan Mar May Jul Sep Nov Jan Mar May Jul Sep Nov 1.2 1 Total 58% 0.9 0.8 0.57 0.6 0.38 0.4 ↓36% ↓33% 0.2 0 2009 2010 2011 CAUTI rate for 2011 is 0.38/1,000 indwelling catheter days. A reduction of 58% compared to 2009. Procedure updated. Removed standing orders for irrigating a catheter Developed a UTI Prevention CBL for SN and for Therapy and Aides Patient care giver education sheet Care of patient with indwelling catheter resulted in > 90% compliance Education completed by 98% (141/144) clinicians Reported infections do not meet the criteria but being treated. Over culturing that may lead to antibiotic resistance Specimen collected inappropriately – clinical UTI but culture contaminated Most patients with catheters have bacteria if left in >30 days APIC: Guide to Elimination of CAUTI, 2008 HICPAC/CDC: Guideline for Prevention of Catheter Associated Best Practice for Indwelling Catheter in the Home Care Setting. HHN vol.22, no12, Dec 2004 Catheter Management in a Home Care Setting. The Quest for Best Practice in Caring for the HC Patient with an Indwelling Urinary Catheter: The New Jersey Experience. Urinary Tract Infections, 2009 Caring, April 2009 HHN vol. 25, No 2, Feb. 2008 Rhinehart E., & McGoldrick ,M..M. (2006). Infection Control in Home Care and Hospice. Sudbury MA.Jones and Bartlett. Good surveillance does not necessarily ensure the making of right decisions, but it reduces the chances of wrong ones” Alexander Langmuir Questions? Carole.Yeung@baptist-health.org