ESF-8 Resource Roundup: Texas Disaster Medical System
advertisement

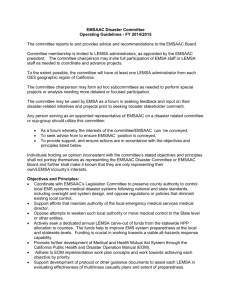
ESF-8: Resource Roundup TEXAS DISASTER MEDICAL SYSTEM TEXAS EMERGENCY MANAGEMENT CONFERENCE APRIL 2012 Objectives Define Emergency Support Function (ESF)-8 Describe ESF-8 Resources Local State Federal Illustrate Resource Request Process Emergency Support Functions 1 Transportation 2 Communications 3 Public Works and Engineering 4 Firefighting 5 Emergency Management 6 Mass Care, Housing, and Human Services 7 Resources Support 8 Public Health and Medical Services 9 Urban Search and Rescue 10 Oil and Hazardous Materials Response 11 Agriculture and Natural Resources 12 Energy 13 Public Safety and Security 14 Long-term Community Recovery and Mitigation 15 External Affairs ESF-8 Functional Areas Health and Medical Supplies/Equipment To support: general / medical shelters, existing medical facilities & EMS assets Assessment of Health and Medical Needs PH infrastructure Mental health care Hospital, dialysis, and LTC facilities and capacity EMS Home-bound population ESF-8 Functional Areas Evacuation Medical ground and air assets Staging Facility evacuations and destinations Embarkation/reception triage/shelter placement In-Hospital Care Surge Resources ESF-8 Functional Areas Medical/PH Care Personnel Deployment teams and staff (see handouts) Health Surveillance General and medical shelters Hospitals, dialysis, and LTC facilities Illness, injuries, and death ESF-8 Functional Areas Food/Drug/Medical Devices Mental Health Services Food safety Disaster behavioral Pharmacy services health Substance abuse services Supplies and equipment O2 ESF-8 Functional Areas Mortuary Services PH/Medical Information Victim Identification Risk messaging Mortuary services Worker health and safety EMS PH policy and guidance ESF-8 Functional Areas Environmental Health Recovery Potable water/ Re-entry of evacuees wastewater Solid waste disposal Infrastructure Vector control Emergency Management Emergency Management EMS Fire Police Law Enforcement ESF-8 Requires Multi-agency Coordination ESF-8 Coordination Local PH Depts Regional PH Depts Non-Profit Orgs Community Based Orgs Faith Based Orgs Public Health RACs LMHA Dialysis Centers Healthcare Providers Academic Health Centers Clinics Nurses Hospitals Doctors Acute Medical Care Local ESF-8 Resources EMS Providers Local Public Health Departments Healthcare institutions Local Mental Health Agencies Trauma Regional Advisory Councils (RACs). Regional DSHS Offices (Health Service Region) Disaster District Committees Regional Advisory Councils 22 Regional Advisory Councils in Texas (A-V) Coordinating body for a trauma service area (TSA) Advancement of healthcare services (trauma, stroke, pediatric, cardiac care) and disaster preparedness Multi-disciplinary approach of regional coordination Hospitals, LTAC, EMS, public safety, public health Trauma Service Areas Correlate with Regional Advisory Councils (RAC) regions What can Regional Advisory Councils do for you? Manage Available Beds HPP Ventilators PPE Supplies Pan Flu PPE Cache Surge Beds Bariatric Cache Regional DSHS Offices 11 Health Service Regions 8 Regional DSHS Headquarters Coordination of local, regional, and state public health partners Ensures the provision of public health services to the community Including during disasters and disease outbreaks Health Service Regions Anchored with Regional DSHS Offices Disaster District Committees Offices (DDCs) that serve as the initial source of state emergency assistance to local jurisdictions Committee Chairman is the local Texas Highway Patrol (Captain or Lieutenant) District Coordinators (formerly RLOs) coordinate disaster preparedness and response in the region Multi-disciplinary response Law enforcement, fire, EMS, emergency management, transportation, public health and medical DPS Regions Correlate with Disaster District Committee (DDC) Regions 7 1. Dallas Region 2. Houston Region 3. McAllen Region 4. El Paso Region 5. Lubbock Region 6. San Antonio Region 6. 7 Capital Region WebEOC & TWIRP Web-based Crisis Information Management System for decision-making before, during, and after disasters Texas WebEOC Interoperability Project (TWIRP) Provision of interoperable communications Consistency throughout the state Improvement of application from Lessons Learned Texas ETN Texas ETN = Emergency Tracking Network Activated by TDEM/DSHS during statewide emergencies Connects 4 disparate standalone systems into an integrated statewide tracking system EMTrack + EvacCenter + SNCA + WebEOC State ESF-8 Resources Department of State Health Services (DSHS) Lead agency for ESF-8 coordination in Texas per Texas Emergency Management Plan, Annex H Texas Disaster Medical System (TDMS) DSHS Public Health Deployable Teams Emergency Medical Task Force (EMTF) Texas Disaster Medical System “Alphabet soup” of Texas ESF-8 Resources drove the need for a coordinated system Formed and funded in 2010 The Texas Disaster Medical System is the collaboration of all public health and acute medical care preparedness initiatives within the State of Texas relating to the mitigation of, response to, and recovery from natural and manmade disasters and other significant events within any region in Texas, with respect to Emergency Service Function (ESF)-8 functions. Steering Committee Objectives Overview – Strategy Document EMTF Oversight Coordination Guidance Training and Exercise for Disaster Teams Medical Information Management and Communication ESF-8 Coordination Acute Care Public Health TDMS Steering Committee ESF-8 Coordination TDMS Today… Gaining knowledge of current planning and operational groups around the state Identifying gaps and overlaps in ESF-8 response Educating local jurisdictions about TDMS Forming 4 subcommittees Resource Typing, Education, Staffing, Document Constructing Overview Document and Strategic Plan DSHS PH Deployable Teams MIST •Medical Incident Support Team •Support medical response efforts of the EOC/DDC RAT •Rapid Assessment Team •Assess public health events and available resources CAT •Command Assistance Team •Public Health-centric Incident Management Team DOG •Diversified Occupational Group •Strike team based on public health specialty DSHS PH Deployable Teams AST(L) ASM CASPER BHAT •Ambulance Strike Team (Leader) •Augment medical transport capacity •Ambulance Staging Manager •Oversight of the Ambulance Staging Area Team •Community Health Assessment for Public Health Response •Documents population-based needs post-disaster •Behavioral Health Assistance Team •Provides crisis counseling, behavioral health resources DSHS PH Deployable Teams MBT •Medical Bus Transport Team •Coordinate use of medical buses in evacuation SST •Shelter Support Team •Provide admin and PH support to shelters RSS •Receiving, Staging, and Storing •Management and inventory control of SNS assets DMS •Disaster Mortality Strike Team •Provide mortuary and victim identification services mergency edical ask orce Need for EMTF? EMTF Response Strategy Rapidly deployable for statewide incidents Builds upon regional capability Integrated command & control elements Self-sufficient for 72 hours NIMS-compliant Modular deployment options ASPR-funded strategy for FY11 & FY12 EMTF Structure Regional & Statewide Strategic Oversight Group Budget, Strategy, Legal, Policy Issues Final Decision-Making Authorities Regional & Statewide EMTF TFL/Managers Operations, Protocols, Mission Profile, Equipment, Position Descriptions, Personnel Management Emergency Medical Task Force Leadership Team •Command/General Staff (from EMS agencies/hospitals in local jurisdictions) •ICS 100, 200, 300, 400, and AHIMT certs, with position specific certs as well •Must have EMS/ER/IMT management experience •Full comms package to communicate with all group and Local EOC/DDC/MACC/DSHS/TDEM-SOC •Logistics package to support all groups 5 Ambulance Strike Teams •5 Ambulances in each Strike Team (25 total ambulances) •Each Strike Team has pre-assigned Strike Team Leader •Teams are Prerostered •10 min launch time for <12 hr deployment •4 hour launch time for minimum for 72 hr deployment with additional gear as needed. 5 RN Strike Teams 2 Ambuses Mobile Medical Unit •5 RN’s in each Strike Team (25 total RN’s) •Each Team has preassigned Strike Team Leader •3 ER Strike Teams •1 ICU Strike Team •1 Specialty area (Burn, OB, Pedi, NICU, etc) •6 hour launch time for minimum of 72 hr deployment •Ambuses are capable of transporting up to 20 litter patients at one time •Pre-plumbed for O2, medical gases, etc •Assigned to EMS agencies that will deploy 4-6 paramedics •10 min launch time for 12 hour deployment •4 hour launch time for 72 hour deployment •16-32 bed capacity •Able to provide emergency stabilizing care (23 hrs only) •Fully staffed with EM physicians, ER nurses, techs, logistics, clerical and other support •6-12 hour launch time for 72 hr deployment •Further typing for MMT integration is in progress Ambulance Strike Teams Currently 32 ASTs engaged, 150+ units 5 Ambulances/AST (25 total) Pre-identified teams No-notice regional deployment Statewide tasked missions Common communications Mobile Medical Units 16-32 bed capacity Provide emergency stabilizing care and transfer Staffed with physicians, nurses, techs, logistics, clerical, etc 6-12 hr launch time for 72-96 hr deployment Standardized cache of supplies, pharmaceuticals, and capabilities EMTF Deployable Zumro Capability AMBUS Project MPV = Multi-Patient Vehicle Transport >12 litter patient at a time Pre-plumbed for O2 and medical gases No-notice regional and statewide taskings 4-6 paramedics/AMBUS MPV: Current Response Statewide Response Within 30 Minutes MPV: Current Response Statewide Response Within 1 hour MPV: Current Response Statewide Response Within 1.5 hrs MPV: Current Response Statewide Response Within 2 hrs MPV: Current Response Statewide Response Within 2.5 hrs What’s in store for 2012? MPV: 2012 Response Statewide Response Within 30 min MPV: 2012 Response Statewide Response Within 1 hr MPV: 2012 Response Statewide Response Within 1.5 hrs MPV: 2012 Response Statewide Response Within 2 hrs MPV: 2012 Response Statewide Response Within 2.5 hrs RN Strike Teams Nurses deployed into a “like” environment – standardized training Must be qualified nurses with critical thinking skills during disaster situations Understand NIMS and disaster response Statewide tasking missions Still being developed Federal ESF-8 Resources Department of Health and Human Services, Office of the Assistant Secretary for Preparedness and Response (ASPR) Lead Agency for Federal ESF-8 Support Supported by 12 Federal agencies and American Red Cross National Disaster Medical System Public & Private sector NDMS partnership Provides medical support to DoD/VA conflicts overseas Supplement state/local medical resources during disasters Major Components of NDMS Supported by: DHHS Definitive Care DHS VA DoD Medical Response Patient Evacuation NDMS Regional & State Teams Disaster Medical Assistance Team (DMAT) National Veterinary Response Team (NVRT) Disaster Mortuary Operations Response Team (DMORT) Specialized Teams (Burns, Peds, Mental Health, Med/Surg, etc) DMAT 35 personnel/team Deploy within 6 hours of activation (14-day deployment) Provide emergency care within 30 minutes of arrival Sustain 24-hr ops for 3-days without external support DMAT Response Capabilities Care Provided Single Team (D+0) 35 PAX 14 Teams (D+1) 490 PAX Treat & Release (Outpatient Facility) 250 patients/day 3,500 patients/day Treat & Limited Holding (Alternate Care Facility) 160 2,250 outpatients/day outpatients/day 112 inpatients Entire NDMS System 7,000 patients/day 4,500 outpatients/day 224 inpatients Standard Medical (Hospital Ward) 50 patients 700 patients 1,400 patients Holding & Collection Facility 150 patients 2,100 patients 4,200 patients 50 DMATs Across the Nation AK MN-1 MINNEAPOLIS AK-1 MI-1 ANCHORAGE WESTLAND NY-2 IA-1 WA-1 TOLEDO DUBUQUE MN ND WA SEATTLE DAYTON MI SD OR EUGENE ID WY HI-1 NV UT KS VT NH NY MD OH HI AZ OK ALBUQUERQUE MO-1 TX LA CA-6 SAN FRANCISCO RI-1 CT PROVIDENCE NC AL GA CT-1 HARTFORD VA NJ-1 LYONS SC CHATTANOOGA NY-4 ROCKLAND CO. NC-1 ST LOUIS NM SC-1 FL AL-1 WINSTON-SALEM CHARLESTON GA-4 BIRMINGHAM AUGUSTA PR AL-3 MOBILE CA-11 SACRAMENTO CA-2 SAN BERNARDINO TN-1 MS NJ DC KY IN AR WORCESTER RI DE WV TN NM-1 MA-2 MA PA NORFOLK MO ME ERIE YOUNGSTOWN IL TULSA CO KY-1 IA BOSTON PA-3 VA-1 OK-1 CA WAILUKU, MAUI DERRY OH-6 M I NE PA-2 PITTSBURG FORT THOMAS WI OR-2 PA-1 OH-5 MT MA-1 VALHALLA OH-1 CA-1 NV-1 CO-2 TX-1 TX-4 SANTA ANA LAS VEGAS DENVER EL PASO DALLAS FL-1 AR-1 PENSACOLA LITTLE ROCK TX-3 FL-6 FL-4 LAMARQUE ORLANDO JACKONSVILLE CA-9 LOS ANGELES CA-4 SAN DIEGO AZ-1 TUCSON GA-3 FL-2 RIVERDALE PORT CHARLOTTE FL-3 ST PETERSBURG FL-5 MIAMI PR-1 SAN JUAN Mobile Acute Care Strike Team 18-person MAC-ST deployed with 24 hours of notification (72 hour deployment) Operational within 1 hour of arrival time Able to receive six critically ill patients and provide critical care from handoff from ambulance personnel transfer to transport personnel NDMS Response Teams 50 • Disaster Medical Assistance Teams 11 • Disaster Mortuary Operational Response Tams 3 • National Pharmacy Response Teams 3 • National Nurse Response Teams 3 • National Medical Response Teams 4 • Burn Teams 2 • Pediatric Teams 1 • Crush Medicine Teams 3 • International Medical/Surgical Teams 2 • Mental Health Teams 5 • National Veterinary Response Teams US Public Health Teams Incident Support Teams Operational Teams 10 Regional IST 5 Rapid Deployment 5 National IST Force Teams 5 Applied Public Health Teams 5 Mental Health Teams 1 National Capital Region IST 5 Emergency Management Group Support Teams Aeromedical Evacuation Definitive Care Patients from area hospitals Disaster Aerial Staging Facility (DASF) At an Aerial Port of Embarkation (APOE) National Disaster Medical System (NDMS) /Federal Coordinating Center (FCC) At Aerial Port Of Debarkation (APOD) National Ambulance Contract Contracted with FEMA Ground Ambulances 300 ALS/BLS Ambulances (split 70%/30%) Air Ambulances 25 Helicopter and/or Fixed Wing Ambulances Para-transit Ability to transport 3,500 individuals NOT 3,500 vehicles Federal Coordinating Centers Receives patients transported from a disaster area (or war zone) Monitors the status of patients once they are placed into a medical facility Coordinates lodging & fiscal information Assists discharged patients in returning home Transport those requiring continued care to their point of origin FCC Locations WA AK MT ND ME MN VT OR NH WI SD ID CA WY PA IA NJ NE UT OH IL CO MO AZ OK NC TN MS DE VA KY AR Services MD WV IN KS 65 FCCs coordinate > 82 receiving areas Solicit and Organize Community Support RI CT MI NV Network of about 2,000 non-Federal hospitals MA NY SC AL TX LA Enroll Non-Federal Local Hospitals in NDMS NM FL USVI Coordinate Bed Availability HI Coordinate with Local/State Authorities GUAM Army FCC GA PR Navy FCC Air Force FCC VA FCC Strategic National Stockpile Provides medicine and medical supplies Stored in different locations across the US Exact locations are not made public 1st push pack available within 12 hours Includes vaccines Managed by HHS/CDC; Deployed by HHS ASPR What is NOT Provided by SNS? Transportation after received by state agency Physical security during state transport Pharmaceuticals in “distribution packages” They arrive in bulk packaging Special handling of vaccines Specialized drug requests (takes additional time) All functions can be supported by DoD if necessary. Federal Medical Stations DHHS asset, managed by CDC, deployed by ASPR Cache of medical supplies and equipment (no personnel) Temporary non-acute medical care facility Requires building (no tents are provided) Inventory = 60+ Provides temporary shelter support for medically fragile, non-hospitalized patients. DoD Deployable Medical Treatment Facilities Army Air Force • Combat Support Hospital • Large and Heavy • Level III care • Expeditionary Medical Support • Light and lean • Needs Base Operating Support • Modular Navy • Comfort/Mercy (Level III care) • Other ships of opportunity (up to level III care) ESF-8: The Spectrum of Care & Federal Medical Resources Volunteers NDMS DMORT NDMS Hospitals NDMS DMATs USPHS RDF Medical Reserve Corps USPHS MHT USPHS APHT Individual Resources Food / Water Safety Basic First Aid Drug / Blood Safety Health Surveillance Mental Health Outpatient Care Pre-hospital Care Emergency Departments Nursing Home Care Hospital Inpatient Care ICU/ Trauma Critical Care Fatalities Management When Disaster Strikes… Follow the standard resource How do I get these resources? request procedure Otherwise reimbursement will be challenging if not impossible Describe your needs and request functions rather than specific teams Understand that there will be a delay – deployments take time Resource Request Flow ALL incidents begin and end LOCALLY Local Resources Mutual Aid Agreements DDC RMOC SOC SMOC TFS EMAC FEMA DDC State Operations Center (SOC) ESF-2 ESF-8 liaison County / Regional MOC (RMOC) requests State assistance for PH&M resources through DDC ESF-6 ESF-11 ESF-8 Lead Agency DSHS State Medical Operations Center (SMOC) RMOC EMTF coordinator Local area requests assistance from county or RMOC Local area requests mutual aid assistance from surrounding areas Mutual Aid not available Other PH/M Resource City/County EOC Local area runs out of PH&M resources Disaster Access to State ESF-8 Resources Access to HHS ESF-8 Resources Locals request support State determines need and submits Action Request Form (ARF) FEMA and ESF-8 Lead evaluate need FEMA generates Mission Assignment (MA) ESF-8 determines best resource to meet need State of Texas Assistance Request Less complicated than its predecessors Fast, easy-to-use interface Statewide consistency and interoperability Able to request resources, information, and missions Updates visible from all levels Does not change request protocol Local State Federal Wrap-Up Regionally, statewide, and federally – we have A LOT of available ESF-8 resources By understanding what is available, you can better prepare your jurisdiction Know the proper procedure for requesting these resources