Module III - Advocate Health Care
advertisement

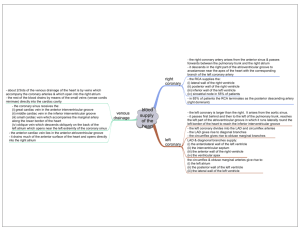
Cardiovascular Emergencies and 12 Lead EKG’s Condell Medical Center EMS System ECRN Packet Module III 2007 Prepared by: Sharon Hopkins, RN, BSN, EMT-P Objectives Upon successful completion of this program, the ECRN should be able to: –understand the normal anatomy & physiology of the cardiovascular system –describe anatomical changes to the heart during ischemic episodes –differentiate presentations of patients with cardiorespiratory complaints –recognize ST elevation on the 12 lead EKG –identify and appropriately state interventions for a variety of dysrhythmias –review discussion of case presentations –successfully complete the quiz with a score of 80% or better Cardiovascular System This system is composed of the heart and blood vessels Delivers oxygenated blood to all cells Transports hormones throughout the body Transports waste products for waste disposal The heart is a pump –right pump is under low pressure –left pump is under high pressure 3 Components of The Circulatory System Functioning heart Sufficient blood volume Intact blood vessels If any one of the above 3 are not working properly, the patient may be symptomatic and could be in need of intervention Superior vena cava Right atrium Right ventricle Aorta Left atrium Left ventricle Myocardial Blood Flow The heart is a muscle (myocardium) 3 layers epicardium - smooth outer surface myocardium - thick middle layer, responsible for cardiac contraction activity endocardium - innermost layer of thin connective tissue Myocardial blood flow – via coronary arteries immediately off aorta – heart is the 1st structure to receive oxygenated blood - it’s that important! Coronary Arteries Left main coronary artery –left anterior descending coronary artery (LAD) supplies left ventricle, septum –circumflex coronary artery supplies left atrium, left ventricle, septum, part of right ventricle Right coronary artery (RCA) supplies right atrium & ventricle Coronary Blood Flow Collateral Circulation Development of new blood vessels to reroute blood flow around blockage in a coronary artery New arteries may not be able to supply enough oxygenated blood to heart muscle in time of increased demand Ischemia occurs when blood supply to the heart is inadequate to meet the demands Influences of Heart Function Preload – pressure under which a ventricle fills; volume of blood returning to fill the heart Afterload – the resistance the ventricle has to pump against to eject blood out of the heart – the higher the afterload the harder the ventricle has to work Ejection fraction (EF) – percentage of blood pumped by the ventricle with each contraction (healthy >55%) – damage to heart muscle decreases EF Influences On Preload & Afterload Preload Afterload increased oxygen arteriosclerosis demand increases induced high B/P volume of blood can cause left returning to heart ventricle to become exhausted temporarily not a & stop working problem efficiently heart enlarges when preload remains increased (FrankStarling law) Problems That Decrease Ejection Fraction (EF) Myocardial infarction (MI) Congestive heart failure (CHF) Coronary artery disease (CAD) Atrial fibrillation Cardiomyopathy Anemia Excess body weight Poorly controlled blood pressure Coronary Artery Disease (CAD) Leading cause of death in USA – Narrowing or blockage in coronary artery decreasing blood flow – Atherosclerosis - thickening & hardening of the arteries due to fatty deposits in vessels – Plaque deposits build up in arteries arteries narrow arteries become blocked blood clots form Overtime, CAD can contribute to heart failure & dysrhythmias Coronary Artery Disease (CAD) Plaque in a coronary artery breaks apart causing blood clot to form and blocks artery Symptoms of Cardiovascular Problems Breathing problems – Shortness of breath (SOB) – Paroxysmal nocturnal dyspnea (PND) suddenly awakens with shortness of breath –Orthopnea dyspnea when lying down –Breath sounds are they clear or not clear? Peripheral edema –excess fluid found in tissues of the most dependent part of the body presacral area in bedridden person feet and ankles in someone up and about Syncope –fainting when cardiac output falls –fainting while lying down is considered cardiac in nature until proven otherwise Palpitations –sensation of fast or irregular heartbeat Pain Initial Impression Not necessarily important to know exactly what to “name” the patient’s problem (diagnosis) Important to identify signs and symptoms that need to be treated – think “what’s the worse case scenario?” Important to recognize the possible medical condition the signs and symptoms may be representing Important to determine the right treatment approach Patient Assessment: OPQRST of Pain Symptoms Onset – Sudden or gradual? – Anything like this before? Provocation or palliation – What makes it better/worse? – What was the patient doing at the time? Quality – What does it feel like (in patient’s own words)? Radiation – From where to where? Severity – How bad is it on a scale of 0-10? Timing – When did it start – How long did it last? – Continuous or intermittent? Vital Signs: Tools for Pt Assessment Heart rate –too fast ventricle does not stay open long enough to adequately fill –too slow rate too slow to pump often enough to maintain an adequate volume output Blood pressure –could be elevated in anxiety and pain –low in shock –serial readings (trending) tell much Respirations – Abnormally fast, slow, labored, noisy? Clear - hear breath sounds enter & exit normal Crackles - pop, snap, click, crackle fluid in lower airways Rhonchi - rattling sounds; resembles snoring mucus in the airways Wheezes - whistling sound; initially heard on exhalation narrowing airways (ie: asthma) Absence of sound - not good!!! Pulse oximetry (SaO2) –Measures percent of saturated hemoglobin in arterial blood –<95% indicates respiratory compromise –<90% indicates dire problem –Need to evaluate reading with patient’s clinical presentation do they match? Inaccurate SaO2 Readings Hypotensive or cold patient (falsely low) Carbon monoxide poisoning (falsely high) Abnormal hemoglobin (sickle-cell disease) (falsely low) Incorrect probe placement (falsely low) Dark nail polish (falsely low) Anemia (falsely high - whatever hemoglobin patient has is saturated) EKG monitoring – Indicates electrical activity of the heart – Evaluate mechanical activity by measuring pulse, heart rate and blood pressure – Can indicate myocardial insult and location ischemia - initial insult; ST depression injury - prolonged myocardial hypoxia or ischemia; ST elevation; injury reversible infarction - tissue death –dead tissue no longer contracts –amount of dead tissue directly relates to degree of muscle impairment –may show Q waves ST depression ST elevation Q wave Acute Coronary Syndrome Variety of events that represent acute myocardial ischemic pain (plaque rupture) Unstable angina Intermediate severity of disease between stable angina and acute MI; tissue ischemia Non-Q wave infarct (NSTEMI) No ST elevation but MI is present with tissue necrosis (death) Q wave infarct (STEMI) ST elevation MI with tissue necrosis (death) Usually a large/significant infarct Acute Myocardial Infarction Coronary blood flow deprived so that portion of muscle dies – occlusion by a thrombus (blood clot superimposed on ruptured plaque) – spasm of coronary artery – reduction in blood flow (shock, arrhythmias, pulmonary embolism) Location and size of infarct depends on which coronary artery is blocked & where – left ventricle most common AMI Signs & Symptoms Chest pain - most common especially in men – lasts >15 minutes – does not go away with rest – typically felt beneath sternum – typically described as heavy, squeezing, crushing, tight – can radiate down the arm (usually left), fingers, jaw,upper back, epigastrium Pain not influenced by coughing, deep breathing, movement Atypical AMI Signs & Symptoms Persons with diabetes, elderly, women, and heart transplant patients Atypical presentation - from drop in cardiac output (CO) – sudden dyspnea – sudden lose of consciousness (syncope) or near-syncope – unexplained drop in blood pressure – apparent stroke – confusion – generalized weakness Atypical AMI Signs & Symptoms Women at greater risk – symptoms ignored (by patient & MD) – under-recognized – under-treated Typical presentation in women – nausea – lightheadedness – epigastric burning – sudden onset weakness – unexplained tiredness/weakness Region X SOP Initial Treatment Acute Coronary Syndrome Regardless of the end diagnosis, all patients treated initially the same – IV-O2-monitor-vital signs-history – aspirin – nitroglycerin – morphine if necessary – 12 lead EKG obtained (transmitted to ED by EMS) Treatment fine-tuned as more diagnostic information is obtained Congestive Heart Failure Heart unable to pump efficiently Blood backs up into systemic system, pulmonary system or both – Right heart failure most often occurs due to left heart failure can occur from pulmonary embolism can occur from long-standing COPD (esp chronic bronchitis) – Left heart failure most commonly from acute MI also occurs due to chronic hypertension Right Heart Failure Blood backs up into systemic circulation – gradual onset over days to weeks – jugular vein distension (JVD) – edema (most visible in dependent parts of the body) from fluids pushed out of veins – engorged, swollen liver due to edema – right sided failure alone seldom a life threatening situation Pre-hospital treatment most often symptomatic More aggressive treatment needed when accompanied with left heart failure Left Sided Heart Failure Heart unable to effectively pump blood from pulmonary veins Blood backs up behind left ventricle Pulmonary veins engorged with blood Serum forced out of pulmonary capillaries and into alveoli (air sacs) Serum mixes with air to produce foam (pulmonary edema) Progression Left Heart Failure Think “left - lungs” Impaired oxygenation – compensates by respiratory rate Fluid leaks into interstitial spaces – auscultate crackles interstitial pressure narrows bronchioles – auscultate wheezing Dyspnea & hypoxemiapanicrelease of adrenalineincreased work load on heart Left Heart Failure Sympathetic nervous system response – Peripheral vasoconstriction peripheral resistance (afterload) increases weakened heart has to pump harder to eject blood out through narrowed vessels blood pressure initially elevated to keep up with the demands and to pump harder against increased vessel resistance diaphoretic, pale, cold skin Asthma or Heart Failure? Asthma Left heart failure younger patient older patient hx of asthma poss hx heart problems unproductive cough orthopnea meds for asthma recent rapid weight gain wheezing cough with watery or foamy fluid accessory muscles being used meds for heart problems wheezing JVD Pedal or sacral edema Which Came First - CHF or AMI? Not unusual to see the AMI patient in pulmonary edema - watch for it! Often hard to determine which came first and triggered the development of the other problem Heart failurepoor perfusion & hypoxemia myocardium suffers from inadequate blood & oxygen supplyacute myocardial ischemiaacute coronary syndrome AMIpoor pumping performance of heartacute failure of left heart pumpleft heart failure Cardiogenic Shock Heart extensively damaged; it can no longer function as a pump 25% of heart damage causes left heart failure if >40% of the left ventricle is infarcted, cardiogenic shock occurs High mortality rate Signs & Symptoms Cardiogenic Shock Altered level of consciousness – confusion to unconsciousness Restless, anxious Massive peripheral vasoconstriction – pale, cold skin, poor renal perfusion Pulse rapid and thready Respirations rapid and shallow Falling blood pressure Treatment Goals Acute Coronary Syndrome Goals – early recognition of a possible cardiac problem – minimize size of infarction – reduce myocardial oxygen demand – decrease patient’s fear & pain (minimizes sympathetic discharge) – salvage ischemic myocardium – prevent development of dysrhythmias – improve chances of survival Region X SOP - Acute Coronary Syndrome Oxygen – may limit ischemic injury Aspirin - 324 mg chewed – blocks platelet aggregation (clumping) to keep clot from getting bigger – chewing breaks medication down faster & allows for quicker absorption – hold if patient allergic or for a reliable patient that states they have taken aspirin within last 24 hours Nitroglycerin 0.4 mg sl every 5 minutes – dilates coronary vessels to relieve vasospams – increases collateral blood flow – dilates veins to reduce preload to reduce workload of heart – if pain persists after 2 doses, Morphine to be started Morphine - 2 mg slow IVP – decreases pain & apprehension – mild venodilator & arterial dilator reduces preload and afterload –2mg slow IVP repeated every 2 minutes as needed, max total dose 10 mg Treatment Goals Congestive Heart Failure Goals – improve oxygenation – decrease workload of the heart (ie: decrease preload & afterload) Region X SOP Treatment Stable Acute Pulmonary Edema (B/P>100) Nitroglycerin - 0.4 mg sl – Vasodilator to create venous pooling – Reduces preload & afterload – Maximum 3 doses (repeated every 5 minutes if blood pressure remains >100) Consider CPAP - use if indicated Region X SOP cont’d Lasix - 40 mg IVP – Diuretic - excess fluid excreted via kidneys – Venodilating effect to pool venous blood – Dose to 80 mg IVP if patient on Lasix at home Morphine - 2 mg slow IVP – Venodilator to increase pooling of blood – Anxiolytic to calm anxious patient – May repeat 2mg dose every 2 minutes – Maximum total dose 10 mg Albuterol - 2.5 mg/3ml nebulizer – Wheezing may indicate bronchoconstriction from excessive fluid – Bronchodilator could be helpful Region X SOP cont’d Hypotensive side effects from treatments used for stable pulmonary edema – Treatment used (NTG, Lasix, Morphine, CPAP) can all cause venodilation B/P – Blood pressure needs to be carefully monitored Region x SOP Treatment Unstable Acute Pulmonary Edema (B/P<100) Contact Medical Control CPAP on orders of Medical Control Consider Cardiogenic Shock Protocol If wheezing (indicating bronchoconstriction), contact Medical Control for Albuterol order – if patient needs to be intubated, Albuterol to be delivered via in-line Treatment Goals Cardiogenic Shock Goals – Improve oxygenation – Improve peripheral perfusion – Avoid adding any workload to the heart Region X SOP Treatment Cardiogenic Shock Oxygen via nonrebreather mask – BVM if respirations ineffective – Intubation may become necessary Positioning – Supine if lungs are clear – Head somewhat elevated if pulmonary edema is present (semi-fowler’s) IV/IO fluid challenge in 200ml increments if lung sounds are clear – The shock may include a hypovolemic component Treatment Cardiogenic Shock Cardiac monitor – Arrhythmias are likely May cause hypotension decreasing cardiac output Dopamine Infusion - maintain B/P >100 – Effects dose related & dependent on clinical condition of patient –5 - 20 g/kg/min has beta influence on the heart Increases contractility strength of heart To a lesser degree increases heart rate Dopamine cont’d – Doses >20g/kg/min Alpha stimulation predominate & vasoconstriction my negatively affect circulation Extravasation - leaking out of vessels – Can cause tissue necrosis – IV infiltration reported to ED staff; document Dosing - start at 5 g/kg/min – Refer to table in SOP page 13 OR – Take patient’s weight in pounds, take 1st 2 numbers, & subtract 2 (ie: 185 pounds: 18 - 2 = 16 gtts/min to start drip) EKG Monitoring & 12 Lead EKG’s Goal EKG monitoring – Identify a disturbance in the normal cardiac rhythm – Arrhythmias caused by Ischemia Electrolyte imbalances Disturbances or damage in electrical conduction system Goal of obtaining 12 lead EKG – Early recognition Acute Coronary Syndrome Treat clinical condition, not the monitor! 12 Lead EKG’s EMS to transmit EKG to Medical control when following the Acute Coronary Syndrome SOP Many patients can be monitored by a Lead II but not all patients need a 12 lead. Some patients experiencing angina or an acute MI will not yet have any EKG changes indicated on the 12 lead. 12 Lead Transmitted From The Field ECRN to complete the radio report ECRN immediately after radio report to retrieve faxed copy of the field 12 lead EKG 12 lead EKG to be immediately presented to the ED physician 12 lead EKG from EMS is to be placed on the patient’s chart after MD review A normal EKG DOES NOT necessarily mean there is nothing acute going on! Cardiac Conduction System SA node - dominant pacemaker – upper right atrium – blood supply from RCA Internodal pathways – to spread electrical impulse thru-out atria AV node in region of AV junction – in 85-90% of people, blood supplied by RCA to AV node – in 10-15% of people, blood supplied by left circumflex Conduction System cont’d bundle of His Right and left bundle branches Purkinje fibers - through ventricular muscle Changes in electrolyte concentrations influence depolarization and repolarization sodium (Na+), potassium (K+), calcium (Ca++), Magnesium (Mg++) Conduction System LLeft bundle lbranches EKG Wave Forms P wave – depolarization of atria PR interval – depolarization of atria & delay at AV junction – normal PR interval 0.12 - 0.20 seconds QRS complex – depolarization of ventricles – normal QRS complex <0.12 seconds T waves – repolarization of ventricles (and atria) The J Point J point - end of QRS complex & beginning of ST segment ST segment elevation - evaluated 0.04 seconds after J point Precordial Chest Leads For every person, each precordial lead placed in the same relative position V1 - 4th intercostal space, R of sternum V2 - 4th intercostal space, L of sternum V4 - 5th intercostal space, midclavicular V3 - between V2 and V4, on 5th rib or in 5th intercostal space V5 - 5th intercostal space, anterior axillary line V6 - 5th intercostal space, mid-axillary Precordial Leads Lead Placement The more accurate the lead placement, the more accurate the 12-lead interpretation when interpreted from all other EKG’s taken on this patient 12-leads are often evaluated on a sequential basis, each interpretation made trying to consider the previous one V4-6 should be in a straight line 12 Lead Printout Standard format 81/2 x 11 paper 12 lead views printed on top half I aVR V1 V4 II aVL V2 V5 III aVF V3 V6 Additional single view of rhythm strips usually printed on bottom of report Machines can analyze data obtained but humans must interpret data Limb Leads (Bipolar) Lead I - views the left (lateral) side of heart Lead II - views the bottom (inferior) side of heart Lead III - another inferior view of the heart I+ Limb Leads (Unipolar) aVR - view from right arm aVL - lateral view from left arm aVF - inferior view from left leg Precordial (Chest) Leads Views the septal, anterior, & lateral portions of the heart Heart in the Thoracic Cavity Myocardial Insult Ischemia – lack of oxygenation – ST depression or T wave inversion – permanent damage avoidable Injury – prolonged ischemia – ST elevation – permanent damage avoidable Infarct – death of myocardial tissue – may have Q wave Evolution of AMI A - pre-infarct B - Tall T wave C - Tall T wave & ST elevation D - Elevated ST, inverted T wave, Q wave E - Inverted T wave, Q wave F - Q wave ST Depression Can indicate ischemia electrolyte abnormality rapid heart rate digitalis influence reciprocal changes to ST elevation ST depression measurement – 1 mm (1 small box) below baseline measured 2 mm (2 small boxes) after end of QRS ST elevation is more significant so should be looked for in opposite leads when depression noted T Wave Inversion T wave represents ventricular repolarization – Normally upright in all leads except V1 and aVR Inverted T waves tend to represent ischemia Note T wave inversion aVL, V4 -6 ST Segment Elevation Myocardium exposed to prolonged hypoxia or ischemia Finding indicates injury or damage Injury probably due to occluded coronary artery Muscle can still be salvaged If corrective intervention not taken in timely manner, tissue necrosis/death is likely (infarction) TIME IS MUSCLE! Significant ST Elevation ST segment elevation measurement – 0.04 seconds after J point ST elevation – > 1mm (1 small box) in 2 or more contiguous chest leads (V1-V6) – >1mm (1 small box) in 2 or more anatomically contiguous leads Contiguous lead – limb leads that “look” at the same area of the heart or are numerically consecutive chest leads Contiguous Leads Inferior wall: II, III, avF Lateral wall: I, aVL, V5, V6 Septum: V1 and V2 Anterior wall: V3 and V4 Posterior wall: V7-V9 (leads placed on the patient’s back 5th intercostal space creating a 15 lead EKG) ST Segment Elevation Coved shape usually indicates acute injury Concave shape is usually benign if patient is asymptomatic Groups of EKG Leads Inferior wall - II, III, aVF Septal wall - V1, V2 Anterior wall - V3, V4 Lateral wall - I, aVL, V5, V6 aVR is not evaluated in typical groups Standard lead placement does not look at posterior wall or right ventricle of the heart - need special lead placement for these views Pathological Q Waves - Infarction Death of tissue Pathological Q wave –>0.04 seconds wide or – 1/3 of R wave height –when seen with ST elevation indicates ongoing myocardial infarction Remember: ST segment probably single most important element on EKG when looking for evidence of AMI Pathological Q Wave Reciprocal Changes Changes seen in the wall of the heart opposite the location of the infarction Observe ST segment depression Usually observed at the onset of infarction Usually a short lived change Lead Reciprocal changes II, III, aVF I, aVL I, aVL, V5, V6 II, III, aVF V1-V4 V7-V9 Acute MI Locator Table Location Leads Reciprocal changes Inferior (RCA) Septal (LAD) Anterior (LAD) Lateral (Circumflex) II, III, aVF I, aVL V1, V2 V3, V4 II, III, aVF V5, V6, I, aVL II, III, aVF Acute Myocardial Infarction Acute myocardial infarction (AMI) is part of a spectrum of disease known as acute coronary syndrome (ACS) ACS – Larger term to cover a group of clinical syndromes compatible with acute myocardial ischemia – Chest pain is due to insufficient blood supply to the heart muscle that results from coronary artery disease (CAD) – Clinical conditions include unstable angina to non-Q wave MI and Q wave MI Common Complications of AMI V1-2: septal wall - infranodal heartblock, BBB V3-4: anterior wall - LV dysfunction, CHF, BBB, 3rd degree HB, PVC’s I, aVL, V5-6: lateral wall -LV dysfunction, AV nodal block in some II, III, aVF: inferior & posterior wall LV - hypotension, sensitivity to Nitroglycerin & Morphine Practice Identifying ST Segment Elevation > 1mm (1 small box) in 2 leads from any group or 2 or more contiguous leads (>2 mm (2 small boxes) in limb leads considered alternative elevation by some) measured 0.04 seconds after J point Think Pattern Recognition Inferior Wall MI I Lateral aVR V1 Septum V4 Anterior II Inferior aVL Lateral V2 Septum V5 Lateral III Inferior aVF Inferior V3 Anterior V6 Lateral Think Pattern Recognition Lateral Wall MI I Lateral aVR V1 Septum V4 Anterior II Inferior aVL Lateral V2 Septum V5 Lateral III Inferior aVF Inferior V3 Anterior V6 Lateral Think Pattern Recognition Anterior Wall MI I Lateral aVR V1 Septum V4 Anterior II Inferior aVL Lateral V2 Septum V5 Lateral III Inferior aVF Inferior V3 Anterior V6 Lateral Think Pattern Recognition Septal Wall MI I Lateral aVR V1 Septum V4 Anterior II Inferior aVL Lateral V2 Septum V5 Lateral III Inferior aVF Inferior V3 Anterior V6 Lateral Test Yourself What pattern would indicate an anterior/septal wall MI? I Lateral aVR V1 Septum V4 Anterior II Inferior aVL Lateral V2 Septum V5 Lateral III Inferior aVF Inferior V3 Anterior V6 Lateral Practice Identifying Leads Showing ST Elevation Evaluate the top 3 rows of the 12-lead EKG Answers follow the 12 lead ST Elevation II, III, aVF Inferior Wall Involvement ST Elevation V5, V6, aVL - Lateral ST Elevation V1-V4 - Ant/Septal ST Elevation II, III, aVF, V6 Inferior & Lateral Wall ST Elevation I, aVL, V2-6 ST Elevation II, III, aVF Case Discussion #1 66 year-old male presents with “indigestion” for past 2 hours, frequent belching, nausea, paleness, diaphoresis, left arm discomfort Vital signs – 102/76 What HR 98 RR 20 SaO2 98% is your impression and what initial treatment is indicated in the prehospital setting? Case #1 Impression: possible AMI (assume and treat for the worse) SOP: Acute Coronary Syndrome Prehospital treatment: – IV-O2-monitor-pulse ox – Vitals stable – History unremarkable – Aspirin chewed (any contraindications?) – Nitroglycerin sl (ask about Viagra use) – Morphine if pain unrelieved after 2 NTG – 12 lead transmitted to ED for interpretation Case #1 12-Lead Case #1 Impression of 12 lead? – no ST segment elevation noted Does lack of ST segment elevation change field treatment for this patient? – Normal EKG does not preclude that acute myocardial event is occurring – Acute Coronary Syndrome SOP to be followed Case Discussion #2 77 year-old female with history of CABG, hypertension, cholesterol, and long standing diabetes Presents with vague complaints of not feeling well, very tired & no energy over the last day Meds: –Aspirin, Isoptin, Toprol, Hydrochlorothiazide, Lipitor, Glucophage Case #2 Vitals: 110/72 HR-72 RR-18 SaO2 97% Monitor (lead II rhythm strip): Case #2 What is your initial impression? Need to at least consider possible MI Remember: –women, elderly, and long standing diabetics report the most atypical complaints Remember: –a lead II only looks at one view of the heart –a normal EKG does not rule out AMI Case #2 Prehospital treatment: –IV-O2-monitor (SR with PVCs)-vitals –Aspirin appropriate? –Nitroglycerin indicated? –12 lead EKG necessary? –What about antidysrhythmic for the PVC’s? call Medical Control for guidance oxygen is often enough to suppress PVC activity Case #2 Aspirin – if patient reliable and took own dose within last 24 hours, can omit, document why omitted and when taken Nitroglycerin – patient not having chest pain. Defer to Medical Control for orders – no contraindications noted (B/P >100; no viagra type drug used within past 24 hours - ask, don’t assume!) 12 lead should be obtained on high index of suspicion Case #3 81 year-old female complaining of shortness of breath for past 2 days. Unable to tolerate lying flat; JVD noted History of CHF, angina, arthritis, and mild COPD Vitals:126/92 HR-170 RR-24 SaO2 97% Medications: nitroglycerin PRN, – Lasix 40 mg daily – Potassium – Aspirin, one daily – Proventil inhaler PRN Case #3 - What is this rhythm? Check the rhythm strip on the bottom Rhythm Case #3 Rapid atrial fibrillation Initial impression? Rapid atrial fibrillation heart rate ineffective pumping cardiac output Prehospital treatment initiated IV-O2-monitor-vitals-history Goal of therapy - slow down heart rate Is patient stable or unstable? – Stable - B/P >100, alert & cooperative Case #3 Prehospital ALS treatment – If Diltiazem not available, then what? Verapamil – 5 mg IVP slowly over 2 minutes – If no response after 15 minutes and B/P remains >100, repeat 5mg slow IVP Carefully monitor patient for development of further deterioration and increased difficulty breathing Position of comfort - usually sitting up Verapamil / Isoptin® Action Calcium channel blocker Slows conduction thru AV node to control ventricular rate Relaxes vascular smooth muscle Dilates coronary arteries Region X SOP - Verapamil Indications Alternative to Diltiazem/cardizem SVT not responsive to 2 doses of Adenosine - to terminate rhythm Stable rapid atrial flutter/fibrillation to control heart rate Dosing 5 mg IVP slowly over 2 minutes If no response after 15 minutes and B/P >100, may repeat Verapamil 5 mg IVP slowly over 2 minutes Verapamil Side Effects Headache, dizziness B/P from vasodilation nausea & vomiting Contraindications B/P Wide complex tachycardias of uncertain origin Heart block without implanted pacemaker WPW, short PR & sick sinus syndromes Case #4 32 year-old male patient with complaints of chest tightness, shortness of breath, and just not feeling well for past 2 days. Also states sore throat and ear pain. Very anxious & scared. No history, no meds Jogs 2-3 miles 5 times per week Vitals: 110/70 HR-68 RR-20 SaO2 98% Lungs clear; skin warm, dry & pink Case #4 Initial impression Cardiac? Musculoskeletal (what has patient been doing)? Viral illness (sore throat & ear pain)? What treatment would EMS begin? Cardiac - can give Aspirin but call Medical Control for NTG or Morphine Normal EKG cannot rule out ACS process Case #5 68 year-old male called 911 due to non-radiating chest discomfort (not relieved with 3 of the patient’s own nitroglycerin) with some minor shortness of breath History: – stable angina – GERD – hypertension (controlled with medications) – Type II diabetic (recently diagnosed) Case #5 Allergies - aspirin Medications – nitroglycerin PRN – isordil – nexium – verapamil – glucophage Vital signs – 136/78 HR-78 RR-18 SaO2 99% What is the initial impression & what prehospital treatment is initiated? Case #5 Initial impression: acute coronary syndrome IV-O2-monitor-SaO2-vitals & history Lead II EKG strip: The patient in case #5 was just hooked up for a 12-lead EKG when they grabbed their chest and became unresponsive Case #5 What is this rhythm strip? What action needs to be taken by EMS? Case #5 - VF Confirm no breathing, no pulse Begin CPR until the defibrillator is ready and is charged to maximum joules Clear the patient & deliver 1 shock Immediately resume CPR for 2 minutes (5 cycles of 30:2) Check rhythm, defibrillate Meds: vasopressor (Epinephrine) antidysrhythmic (choose 1) 1 shock in between meds & 2 min CPR VF/Pulseless VT SOP Meds Epinephrine 1mg every 3-5 minutes IV/IO for duration of arrest Antidysrhythmic: Amiodarone 300 mg IV/IO 1st dose OR Lidocaine 1.5 mg/kg IV/IO 1st dose Repeat dose antidysrhythmic x1 in 5 min: If Amiodarone given, then 150 mg IV/IO OR If Lidocaine given, then 0.75 mg/kg IV/IO Antidysrhythmics in VF/VT Amiodarone to the vein) needs to be diluted (irritable – total of 20 ml syringe (med mixed with saline) – rapid push in VF/VT (slow if pt has pulse!) Lidocaine - – if unsuccessful defibrillation contact Medical Control for 3rd dose order – if defib successful & bolus given < 10 min, begin drip 2mg/min (30 mcgtts) – if defib successful & bolus given >10 min, give Lido 0.75 mg/kg IV/IO & start drip Case #5 The patient was defibrillated twice and received 1 dose of epinephrine After the 3rd shock, 2 minutes of immediate CPR resumed After 2 min of CPR, what is the rhythm? Case #5 Rhythm: sinus rhythm EMS action? – Determine if there is a pulse (yes!!!) – Reevaluate airway, breathing, circulation-B/P – Medications: because no antidysrhythmic were given, need to call Medical Control for direction if Lidocaine, usually 0.75 mg/kg IV/IO if Amiodarone, 150 mg diluted into 100 ml bag D5W; run thru mini-drip tubing; run piggyback at rapid drip over 10 minutes May not want any antidysrhythmic given ETT Route Endotracheal tube route is discouraged, not eliminated. Absorption found to be unpredictable ETT drugs if this route is used L - Lidocaine E- Epinephrine A- Atropine N - Narcan Double the calculated amount for the IV/IO route Bibliography American Heart Association Guidelines CPR ECC 2005 Beasley, B., West, M. Understanding 12Lead EKG. Pearson Ed, 2001. Caroline, Nancy. Emergency Care in The Streets, Jones & Bartlett, 2008. Page, B. 12-Lead EKG, Pearson, 2005. Phalen, T, Aehlert, B. The 12-Lead EKG in Acute Coronary Syndromes, 2006. www.clevelandclinic.org www.nhlbi.nih.gov/health/dci/Diseases