NURS 2410 Unit 3
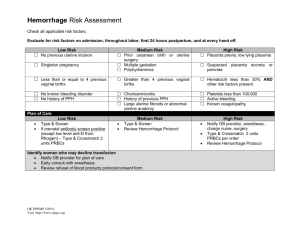
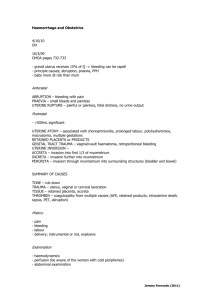
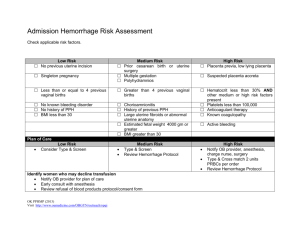
advertisement
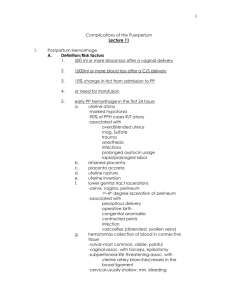
Nancy Pares, RN, MSN Metro Community College Relate specific pathophysiology and nursing process specific to postpartum. Idenitify specific post partum complications and nursing management ◦ Placental issues, uterine issues, vaginal issues Fundal height and tone Vaginal bleeding Signs of hypovolemic shock Development of coagulation problems Signs of anemia Cesarean delivery Unusually large episiotomy Operative delivery Precipitous labor Atypically attached placenta Fetal demise Previous uterine surgery Uterine atony Lacerations of the genital tract Episiotomy Retained placental fragments Vulvar, vaginal, or subperitoneal hematomas Uterine inversion Uterine rupture Problems of placental implantation Coagulation disorders Uterine massage if a soft, boggy uterus is detected Encourage frequent voiding or catheterize the woman Vascular access Assess abnormalities in hematocrit levels Assess urinary output Encourage rest and take safety precautions Health-seeking Behaviors related to lack of information about signs of delayed postpartal hemorrhage Fluid Volume Deficit related to blood loss secondary to uterine atony, lacerations, hematomas, coagulation disorders, or retained placental fragments Adequate prenatal care Good nutrition Avoidance of traumatic procedures Risk assessment Early recognition and management of complications Fundal massage, assessment of fundal height and consistency Inspection of the episiotomy and lacerations if present Report: ◦ Excessive or bright red bleeding, abnormal clots ◦ Boggy fundus that does not respond to massage ◦ Leukorrhea, high temperature, or any unusual pelvic or rectal discomfort or backache • • • • • Clear explanations about condition and the woman’s need for recovery Rise slowly to minimize orthostatic hypotension Woman should be seated while holding the newborn Encourage to eat foods high in iron Continue to observe for signs of hemorrhage or infection Risk factors ◦ Overdistension of the uterus ◦ Uterine anomaly ◦ Poor uterine tone Assessment findings ◦ Excessive bleeding, boggy fundus Management ◦ Fundal massage ◦ Blood products if loss is excessive ◦ Medications Oxytocin, methergine, carboprost tromethamine (Hemabate) Risk factors ◦ Mismanagement of third stage ◦ Placental malformations ◦ Abnormal placental implantation Assessment findings ◦ Excessive bleeding, boggy fundus Accreta villi attach to the outer layer myometrium Increta villi attach within the muscle layer of the myometrium Percreta villi attach deep within the myometrium Management ◦ Manual exploration of the uterus ◦ D&C ◦ Blood products if loss is excessive Risk factors ◦ ◦ ◦ ◦ Operative delivery Precipitous delivery Extension of the episiotomy Varices Assessment findings ◦ Excessive bleeding with a firm uterus Management ◦ Suture if needed ◦ Blood products if loss is excessive Identify nursing process for post partum psycho social disorders Depression scales Anxiety and irritability Poor concentration and forgetfulness Sleeping difficulties Appetite change Fatigue and tearfulness Occurs within 3 to 10 days of delivery Generally transient Usually resolves without treatment Assessment findings ◦ Tearful, fatigue, anxious, poor appetite Etiology ◦ Hormonal changes and adjustment to motherhood Longer than two weeks in duration requires medical evaluation Onset slow, usually around the fourth week after delivery Assessment findings ◦ Depressed mood, fatigue, impaired concentration, thoughts of death or suicide Risk factors ◦ History of depression, abuse, low self-esteem Management ◦ Psychotherapy, medications, hospitalization Generally after the second PP week Assessment findings ◦ Sleep disturbance, agitation, delusions Risk factors ◦ Personal or family history of major psychiatric illness Management ◦ May lead to suicide or infanticide ◦ Hospitalization, medications, psychotherapy • • • • • • Help parents understand the lifestyle changes and role demands Provide realistic information Anticipatory guidance Dispel myths about the perfect mother or the perfect newborn Educate about the possibility of postpartum blues Educate about the symptoms of postpartum depression Signs and symptoms of postpartum depression Contact information for any questions or concerns Foster positive adjustments in the new family Assessment of maternal depression Teach families symptoms of depression Give contact information for community resources Make referrals as needed Ineffective Individual Coping related to Risk for Altered Parenting related to postpartum depression postpartal mental illness Risk for Violence against self (suicide), newborn, and other children related to depression Components of grief work ◦ Accepting the painful emotions involved ◦ Reviewing the experiences and events ◦ Testing new patterns of interaction and role relationships Four stages of grief ◦ ◦ ◦ ◦ Shock and numbness Searching and yearning Disorientation Reorganization Symptoms of normal grief Inability to conceive Spontaneous abortion Preterm delivery Congenital anomalies Fetal demise Neonatal death Relinquishment SIDS Review nursing interventions associated with ◦ DVT, Hematoma, hemorrhoids, endometritis, wound infections, urinary infections and STD R: redness E: edema E: ecchymosis D: discharge A: approximation Fever Malaise Abdominal pain Foul-smelling lochia Larger than expected uterus Tachycardia • • • • Risk for Injury related to the spread of infection Pain related to the presence of infection Deficient Knowledge related to lack of information about condition and its treatment Risk for Altered Parenting related to delayed parent-infant attachment secondary to woman’s pain and other symptoms of infection Infection of the uterine lining Risk factors ◦ Cesarean section Assessment findings ◦ Fever, chills ◦ Abdominal tenderness ◦ Foul-smelling lochia Management ◦ Antibiotics Breast consistency Skin color Surface temperature Nipple condition Presence of pain Infection of the breast Risk factors ◦ Damaged nipples ◦ Failure to empty breasts adequately Assessment findings Management ◦ Fever, chills ◦ Breast pain, swelling, warmth, redness ◦ Antibiotics ◦ Complete breast emptying Proper feeding techniques Supportive bra worn at all times to avoid milk stasis Good handwashing Prompt attention to blocked milk ducts Importance of regular, complete emptying of the breasts Good infant positioning and latch-on Principles of supply and demand Importance of taking a full course of antibiotics Report flu-like symptoms Health-seeking Behaviors related to lack of information about appropriate breastfeeding practices Ineffective Breastfeeding related to pain secondary to development of mastitis • • • • • Home care nurse may be the first to suspect mastitis Obtain a sample of milk for culture and sensitivity analysis Teach mother how to pump if necessary Assist with feelings about being unable to breastfeed Referral to lactation consultant or La Leche League Homan’s sign Pain in the leg, inguinal area, or lower abdomen Edema Temperature change Pain with palpation Inflammation of the lining of the blood vessel due to clot formation ◦ Can occur in the legs (DVT) or pelvis (SPT) Risk factors ◦ Cesarean section ◦ Prolonged bed rest ◦ Infection Assessment findings ◦ Pain, fever, redness, warmth, tender abdomen/calf Management ◦ Anticoagulants ◦ Antibiotics for septic pelvic thrombophlebitis Avoid prolonged standing or sitting Avoid crossing her legs Take frequent breaks while taking car trips Condition and treatment Importance of compliance and safety factors Ways of avoiding circulatory stasis Precautions while taking anticoagulants Pain related to tissue hypoxia and edema secondary to vascular obstruction Risk for Altered Parenting related to decreased maternal-infant interaction secondary to bed rest and intravenous lines Altered Family Processes related to illness of family member Deficient Knowledge related to self-care after discharge on anticoagulant therapy Large mass in abdomen Increased vaginal bleeding Boggy fundus Cramping Backache Restlessness Frequency and urgency Dysuria Nocturia Hematuria Suprapubic pain Slightly elevated temperature Risk factors ◦ Urinary catheterization ◦ Long labor, operative delivery Assessment findings ◦ Dysuria, frequency, urgency ◦ Fever ◦ Suprapubic pain Management ◦ Antibiotics Good perineal care Hygiene practices to prevent contamination of the perineum Thorough handwashing Sitz baths Adequate fluid intake Diet high in protein and vitamin C Good perineal hygiene Good fluid intake Frequent emptying of the bladder Void before and after intercourse Cotton underwear Increase acidity of the urine Frequent monitoring of the bladder Encourage spontaneously voiding Assist the woman to a normal voiding position Provide medication for pain Perineal ice packs Risk for Infection related to urinary stasis secondary to overdistention Urinary Retention related to decreased bladder sensitivity and normal postpartal diuresis Pain with voiding related to dysuria secondary Health-seeking Behaviors related to need for to infection information about self-care measures to prevent UTI Activity and rest Medications Diet Signs and symptoms of complications Importance of completion of antibiotic therapy May need assistance when discharged from the hospital May need a referral for home care services Instruct family on care of the newborn Instruct mother about breast pumping to maintain lactation if she is unable to breastfeed Instruct family members on care of mother and newborn Referral for home care if necessary Provide resources for follow-up or questions Teach all families to observe for signs and symptoms Assessment findings ◦ Severe perineal pain ◦ Ecchymosis ◦ Visible outline of the hematoma ◦ Blood loss may not be visible Treatment ◦ ◦ ◦ ◦ Surgical drainage Antibiotics Analgesics Blood products if loss is excessive Hypotension Tachycardia, weak, thready pulse Decreased pulse pressure Cool, pale, clammy skin Cyanosis Oliguria, anuria Thirst Hypothermia Behavioral changes (lethargy, confusion, anxiety) Pg 664- table Monitor vital signs frequently Large-bore IV for fluids, blood products Administer oxygen, assess oxygen saturation Assess hourly urine output Assess level of consciousness Administer and monitor fluids, blood products Draw/monitor laboratory results Assess quantity and quality of bleeding Provide emotional support to patient/family Fever > 100.5 Severe pain, redness,swelling at incision site Passing of large clots Increased bleeding Burning on urination Insomnia Impaired concentration Feeling inadequate