the importance of occupational and environmental epidemiology for
advertisement

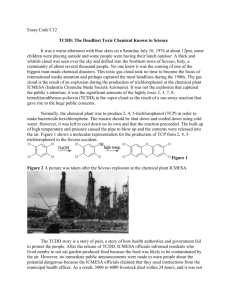
6° EASOM Summer School August 31st - September 2nd, 2006 THE IMPORTANCE OF OCCUPATIONAL AND ENVIRONMENTAL EPIDEMIOLOGY FOR THE OCCUPATIONAL HEALTH PRACTICE Pier Alberto Bertazzi University of Milan & IRCCS Maggiore Hospital Foundation Milan, Italy Outline • Challenges ahead • Epid. designs to address them • Seveso as a case in point OH Practice • Traditionally, the recognition, diagnosis and control of occupational risks and diseases have been following well specified and standardized procedures (regulated sometimes not just by medical and scientific competence but even by law). The OH practice was essentially called to comply with those regulations. Occup/envir. epidemiology • Occup/envir epidemiology has mainly been serving OH practice by addressing particular, specific issues, in particular occupational cancer hazards identification. Changes at the workplace Today, things have changed and still are changing at work, in science and in medicine. • Workplace hazards are less obvious to identify and to measure. • Occupational factors increase the risk of “common” diseases (a-specific effects) • Specific effects are vague, psychological, subjective (distress, discomfort). • Genetics and behaviour are becoming more and more relevant. • Working population is changing in terms of age structure, sex composition, and ethnicity. Change in hazards Workplace hazards are less obvious to identify and measure (and hence to control) • Population vs. sick individual approach • Longitudinal observation of exposed (exposure-dose-early effect-disease) Change in effects I Occupational factors increase the risk of common diseases (a-specific effects). • Populations comparison (exposed vs. reference) • Small increase in risk visible only in relative terms (vs. background) • Need to observe large groups. Change in effects II Specific effects are vague in nature, mainly psychological, subjective (distress and discomfort). • Accuracy and validity of diagnostic means and procedures • Surveillance of healthy population not of sick individuals • Need to observe large groups. Novel causative components Genetic and behavioural components are becoming more and more relevant. • Gene – environment interaction as population effect • Psychic and psychosomatic effects (lagoon of causative factors) • Avoid bias, control confounding, consider interactions. Working population change Working population is changing in terms of age structure, sex composition, and ethnicity. • Relevance of inherited and acquired susceptibility. • Multi-component causative web • Targeted interventions including re-training and health promotion The core type of activity needed in such a changing context: OBSERVATIONAL STUDY OF EXPOSED POPULATION OVER TIME This is…… ….What we ought to contribute to, when we practice Research ….What we have to teach to our students Teaching ….What can confer appropriateness and effectiveness to OH practice and intervention Practice ….What makes evaluation possible Evaluation PRIORITIES IN OCCUPATIONAL HEALTH RESEARCH - UK • Natural history of work related ill health Musculoskeletal disorders (back & upper limb) Asthma Accidents Skin disease Vibration induced disease Suicide Depression Hearing loss • Audit in occupational health screening procedures • Environmental impact of industrial activity Community > individual level • Stress related disease • Neuro-psychological effects • Cost-effectiveness of occupational health • Risk assessment • Reproductive hazards • Effects of pharmacological agents • Development of biomarkers as early evidence of an exposure effect Need to answering new questions about safety and health at the workplace: Which study design? Depends on the exposure and nature of health outcome of interest, and on feasibility Cohort Follow up of an exposed population and determination of subsequent incidence of health outcomes • Historical - long induction and latency period • Prospective – short temporal relation between exposure and subsequent risk Cross sectional Comparison of disease prevalence among groups classified according to exposure. • Study of persistent conditions (rather than transient and reversible) • Repeated measurement study Case-control Exposure comparison between an index case group and a reference group of persons free of the disease at the time of case definition • • Nested within a cohort Community based Case-cohort Multiple case groups and a common comparison group, “reference sub-cohort”, random sample of the source population (cohort) • Efficient in testing associations with multiple health outcomes Case-crossover Comparison of cases’ exposure immediately before their events with exposure that occur at other typical times. Each case serves as his/her matched control. • Suitable for risk factors of health outcomes that occur in close temporal sequence to exposure (disease triggers). • Full control of time invariant confounders (genetics) CASE CROSSOVER DESIGN (Mc Lure 1991) In the light of the specific issues we are facing today in OSH….. • Strategy of choice appears to often be a combination of epidemiologic studies. • The best way to illustrate and to teach this is through examples (hypothetical, at least) of complex multi-causal effects and given workplace exposure or case studies of complex exposures related to multiple effects (e.g., the Seveso accident). Lombardy Region ICMESA, the Seveso Accident plant Dept. B: Production of 2,4,5-trichlorophenol TCP Seveso, Italy, 1976 TCP production plant Cl O Cl Cl O Cl 2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) Seveso, Italy, 1976 DESIGN and CONDUCT ISSUES • • • • • • • • • Exposure: type, entity, duration. Exposed/Pop. at risk: definition, identification. Effects: type, latency, diagnosis. Follow-up: contact, observation, means and procedures. Study: type of design, study population (sample), duration. Reference population: control of confounding. Information: validity and quality. Analyses and interpretation. Communication: scientific and social. OBJECTIVES ADDRESSED AFTER THE ACCIDENT - Ascertaining the exposure, its nature and characteristics, the extent of contamination and number of people involved - Managing the risk with preventive measures for people and their environment - Planning and conducting health surveillance programs EXPOSURE ASSESSMENT EMISSION SOURCE - pollutant type - amount released ECOLOGICAL AND ENVIRONMENTAL MEASUREMENTS - surface soil - deeper soil layers - water - airborne dust - vegetation - animals - cow’s milk HEALTH EFFECTS - early and mid-term - long term HUMAN EXPOSURE/ DOSE - personal habits and activities - chloracne - biological samples Exposure The Seveso area Zone A Accident Zone A Zone Pop Population: 804 Soil TCDD (1976): 15.5-580.4 µg/m2 Soil concentration Min Zone B Max Reference 580.4 zone A 804 15.5 B 5,941 1.7 4.3 R 38,624 0.9 1.4 Reference 232,745 NA NA Zone R Bertazzi et al., Environ Health Perspect 1998 The Seveso area Zone B Accident Zone A Zone Pop Population: 5,941 Soil TCDD (1976): 1.7-4.3 µg/m2 Soil concentration Min Zone B Max Reference 580.4 zone A 804 15.5 B 5,941 1.7 4.3 R 38,624 0.9 1.4 Reference 232,745 NA NA Zone R Bertazzi et al., Environ Health Perspect 1998 The Seveso area Zone R Accident Zone A Zone Pop Population: 38,624 Soil TCDD (1976): 0.9-1.4 µg/m2 Soil concentration Min Zone B Max Reference 580.4 zone A 804 15.5 B 5,941 1.7 4.3 R 38,624 0.9 1.4 Reference 232,745 NA NA Zone R Bertazzi et al., Environ Health Perspect 1998 The Seveso area Reference Accident Zone A Zone Pop Population: 232,745 Soil TCDD (1976): NA Soil concentration Min Zone B Max Reference 580.4 zone A 804 15.5 B 5,941 1.7 4.3 R 38,624 0.9 1.4 Reference 232,745 NA NA Zone R Bertazzi et al., Environ Health Perspect 1998 TCDD plasma levels, 1976 Plasma TCDD (ppt) 100,000 10,000 1,000 100 10 } Zone Zone AA Zone B Background Zone R Needham et al., Chemosphere 1998 Plasma TCDD after 20 years Plasma TCDD (ppt) . 70 TCDD Range: 1.0-89.9 ppt, lipid adjusted 60 Females 50 Males 40 30 20 10 0 Zone A Zone BB Zone Zone A Reference Landi et al., Lancet 1997 Early cross-sectional studies CHROMOSOMAL ABERRATIONS IN LYMPHOCYTES, 1977 Exposure No. No. Aberrant cells % Subjects Mitoses Gaps + Gaps - Acute Chronic Controls (De Carli et al. 1982) 145 69 87 6470 3040 3958 2.49 2.53 1.64 0.99 0.92 0.48 CONGENITAL MALFORMATIONS ZONES A+B+R vs. REFERENCE DEFECTS JAN-APR 1977 RR TOTAL MAJOR MILD 90% CI 1977-1982 RR 90% CI 1.49 0.64-3.45 0.97 0.83-1.13 0.93 0.26-3.32 0.83 0.67-1.04 2.50 0.79-7.94 1.14 0.92-1.42 (Mastroiacovo et al. 1988) CHLORACNE CASES 1976-1977 ZONE A total A-max B R R Polo Outside SUBJECTS CHLORACNE PERCENT 3-14 YRS. CASES 214 54 1,468 8,680 750 48,263 (Caramaschi et al. 1981) 42 26 8 63 19 51 19.6 48.1 0.5 0.7 2.5 0.1 Incidence studies Mortality (Zone A+B) Males Females Obs RR* (95% CI) Obs RR* (95% CI) All Causes 438 1.0 (0.9-1.1) 307 1.0 (0.9-1.1) All Cancers 166 1.1 (1.0-1.3) 83 0.9 (0.7-1.1) Lympho/Hemato 15 1.7 (1.0-2.8) 13 1.8 (1.1-3.2) Rectum 10 2.4 (1.2-4.6) 3 1.1 (0.4-3.5) 28 1.4 (0.9-2.0) 18 1.0 (0.6-1.5) CHD *Analysis adjusted for age and sex Bertazzi et al., Am J Epidemiol 2001 Cancer incidence (Zone A+B) Males Females Obs RR* (95% CI) Obs RR* (95% CI) All Cancers 122 1.0 (0.8-1.1) 82 1.0 (0.8-1.2) Lympho/Hemato 15 1.9 (1.1-3.1) 10 1.6 (0.9-3.1) Non-Hodgkin 8 2.6 (1.3-5.6) 3 1.2 (0.4-3.7) Multiple Myeloma 2 1.9 (0.5-8.0) 3 4.9 9 2.0 (1.0-3.9) 3 1.1 (0.3-3.4) 10 1.3 (0.7-2.4) 7 2.4 (1.1-5.1) Breast - - - 23 0.9 (0.6-1.3) Endometrium - - - 2 0.5 (0.1-2.0) Ovary - - - 1 0.2 (0.1-1.6) Vagina - - - 2 5.5 Rectum Hepatobiliary *Analysis adjusted for age and sex (1.5-16) (1.3-24) Pesatori et al., Ind Health 2003 OFFSPRING SEX RATIO AND PARENTAL TCDD LEVELS ZONE A BLOOD TCDD RANGE (ppt), 1976 Family # Father OFFSPRING (1977-84) Mother Male Female 1-9 104-2340 126-1650 0 12 10-13 29.3-65.4 4 1 (Mocarelli et al. 1996) ND-36.5 Case-control retrospective study Chloracne Case-Control Study Higher TCDD exposure: The only determinant of chloracne? 101 chloracne cases Median age: 8 years 211 controls Enrollment: 1993-1998 Opportunity to identify susceptibility factors! Plasma TCDD range 450 400 475 ppt 350 300 250 200 150 125 ppt 100 50 0 nd Chloracne Cases Chloracne Cases nd Controls Healthy Controls Mean plasma TCDD Chloracne 10 Plasma TCDD (ppt) . 9 8 7 6 5 4 3 2 1 0 Chloracne NO Controls YES Potential Susceptibility Factors TCDD>10 ppt 10 9 p-interaction=0.02 Odds Ratio 8 7 p-interaction=0.04 9.2 (2.6-33) 7.4 (1.8-30) 6 5 4 3 2.1 3.7 (1.6-8.8) (0.7-6.1) 1.3 2 (0.6-3.1) 1 all All subjects <=8 <=8 years years >8 years years >8 AGE Light Light Dark Dark HAIR COLOR Analysis adjusted for age, sex and zone of residence Health conditions after 20 years No differences between chloracne cases & healthy controls • • • • • • Allergic diseases Gastrointestinal disorders Infectious diseases Endocrine disorders Respiratory diseases Offspring health status Baccarelli et al., Br J Dermatol, 2005 Late cross-sectional studies Subclinical conditions after 20 years Subjects with high plasma TCDD • Decreased IgG plasma levels (Baccarelli, EHP 2002) • AhR-related transcript alterations (Landi Carcinogenesis 2003, Baccarelli Tox Lett 2004) IgG plasma levels 1600 1400 p=0.03 p=0.01 IgG (mg/dl) 1200 1000 800 600 400 200 0 Reference Reference Zone ZoneBB Zone ZoneAA Baccarelli et al., Environ Health Perspect 2002 Plasma TCDD vs. IgG 2500 n = 109 r = -0.35 p = 0.0002 IgG (mg/dl) 2000 1500 1000 750 1 5 10 20 30 50 90 Plasma TCDD (ppt, lipid adjusted) Baccarelli et al., Environ Health Perspect 2002 Need to rediscover population approach coupled with high risk individual approach Epidemiology has largely ceased to function as part of a multidisciplinary approach to understanding the causation of disease in populations and has become a set of generic methods for measuring associations of exposure and disease in individuals. ……. (for studying) decontextualized individual risk factors, rather than to study population factors in their social and historical context. …… We seem to be using more and more advanced technology to study more and more trivial issues, while the major causes of disease are ignored. Epidemiology must reintegrate itself into public health and must rediscover the population perspective”. (N. Pearce, Am J Public Health, 1996, 86:678-683) PREGNANCY LOSS RATE, 1976-1977, BY TRIMESTER TRIMESTER ZONE B 07-09 ‘76 10-12 ‘76 01-03 ‘77 04-07 ‘77 07-09 ‘77 10-12 ‘77 (Bisanti et al 1980) 11.1 22.2 17.2 28.5 31.2 13.7 ZONE R REFERENCE 13.7 16.3 12.7 12.5 11.4 13.8 11.0 14.8 16.6 13.0 10.5 14.3 Effect of plasma TCDD Plasma TCDD p=0.03 AhR p=0.01 p<0.001 AhR EROD ARNT p=0.001 DRE + _ Uncultured cells p=0.03 p=0.001 p<0.001 CYP1A1 TCDD stimulated Cells CYP1B1 Baccarelli et al., Tox Lett 2004