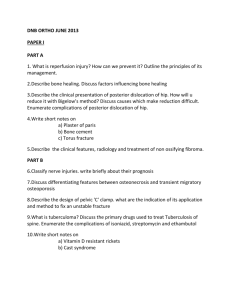
2013.11.21 Mortality review (Intraabdominal injury)
advertisement

MORTALITY REVIEW: CRITICAL INCIDENTS Dr Tengku Abdul Kadir Tengku Zainal Abidin Supervised by: Dr Khairuddin Ismail Patient History • Mr MASR • 17YO Malay male • Alleged MVA MB vs car near UNISZA – unsure mechanism, wearing helmet, unsure drug influence • Brought to ED by JPAM Arrival at ED • Arrived at 1 am • GCS E1V2M5 (8/15), pupils (R) 4 mm sluggish (L) 3 mm reactive • Haemodynamically: BP 70-90/40-60, HR persistently tachycardic 110-160 • Intubated for airway protection by ED team • Fluid resuscitation: Total 14 pints IVD, 8 pints whole blood, 2 cycles DIVC then started on noradrenaline infusion Investigations • FBC • ABG: pH 7.14 pCO2 52 pO2 188 HCO3 17 BE -12 sO2 99 • FAST scan: Initially –ve x 4, then free fluid seen at hepatorenal and splenorenal area • Radiographs: • CXR normal • Pelvic x-ray: Dissociation of left SIJ 0.9 cm, pubic diasthesis 5 cm post pelvic binder pubic diasthesis 1.5 cm • Left humerus: Comminuted # midshaft • Left radial/ulnar: # distal 3rd radius with DRUJ disruption • Left hand: # neck of 5th MCB, # base 3rd and 4th MCB • CT brain normal Clinical Findings • Multiple abrasion and laceration wounds over face and • • • • • scalp No signs of basal skull fracture Chest spring –ve Abdomen distended over right side but soft Deformed and oedematous left UL with puncture wound over hand Swelling and haematoma extending from RIF to midthigh area, including bilateral scrotum Problem List Alleged MVA with polytrauma: 1. Severe head injury 2. Open book fracture 3. Intraabdominal injury 4. Open comminuted fracture midshaft left humerus 5. Open left Galeazzi fracture 6. Open fracture base of 3rd and 4th left MCB 7. Open fracture neck of 5th left MCB Progress • Primary team (surgical and orthopaedics) decided for • • • • • operation Surgical concerned of pelvic instability Ortho: surgical should proceed in view of intraabdominal injury as pelvis stabilised with pelvic binder + external fixator may impede laparotomy Case notified to anaes OT and confirmed OT at 6.07 am by ortho and 6.30 am by surgical Called to OT at 6 am and was sent stat Vital signs during transfer supported by noradrenaline double strength 10 ml/hour – BP 100/50, HR 100-127 Events in OT • Arrived in OT 6.25 am • Patient intubated on manual bagging, GCS 2T/15, pupils • • • • (R) 4 mm sluggish (L) 3 mm sluggish Clinically very pale, poor perfusion, poor PV Abdomen distended and tense Sedation IV midamorphine 1 ml/hour, noradrenaline 10 ml/hour CVL inserted in OT (USG guided) Intra-operative Events • External pelvic fixation by orthopaedics started at 7.25 am • • • • and exploratomy, splenectomy and abdominal packing by surgical at 7.49 am Intra-operatively, ventilated on PC FiO2 1 / PIP 14 / PEEP 8 BP 94-125/40-60 (MAP 36-50), HR 80-98 titrate up noradrenaline to 25 ml/hour Fluid resuscitation: 6 pints NS, 5 pints gelafundin, 1 cycle DIVC, 8 pints WB (urine output not documented) Surgery ended 8.50 am, EBL 3000 ml Post-operative Events • BP 120/49, HR 89 (IV noradrenaline 25 ml/hour) • spO2 highest 93% on 100% O2 • Bradycardic then PEA at 9.25 am • CPR 20 minutes, IV adrenaline total 10 mg, blood and colloid pushed in • Persistent oozing from laparotomy site spilling onto bed – surgical informed • Fresh blood from ETT • Transferred to ICU with BP 120/77, HR 101 Arrival in ICU ~ 9:45am • Arrived in ICU with IVI noradrenaline 35 ml/hour, IV dopamine 10 ml/hour • Cold peripheries, poor perfusion, very pale • Pupils 7 mm bilaterally fixed and dilated • Continuous bleeding from external fixation pin site and laparotomy wound with abdomen distended Deterioration ~10:00am • Cardiac monitor: HR 80-90, NIBP 66/30 • Slowly bradycardic then PEA • CPR commenced x 50 minutes • Total IV adrenaline total 10 mg • 1 pint crystalloid, 2 pints colloid, 3 pints WB pushed in; 1 cycle DIVC requested • Noradrenaline increased to 60 ml/hour, dopamine 20 ml/hour • Not reverted – asystole at 10:40am • COD: Severe abdominal injury complicated with DIVC and hypovolaemic shock Pelvic XR before pelvic clamp Pelvic XR after pelvic clamp FBC pre operation – on arrival PTTK, pre operation ABG trend Intraoperative monitoring Intraoperative monitoring Intraoperative monitoring FBC pre and post OP. Open for discussion… • 1. Delayed operation. • - time of resuscitation in ED • - late pelvic fixation. • - decision of operation 2. Intraoperation - Difficulty of IVL, art line, call for help? adequate team? - inform progress to sp? Communication. - unstable hemodynamically 3. Degree of bleeding - Diagnose severity of bleeding, %?, ABG, - restore perfussion, control bleeding. 4. Pre op assessment,plan. 5. Communication to specialist, team to team