投影片 1
advertisement

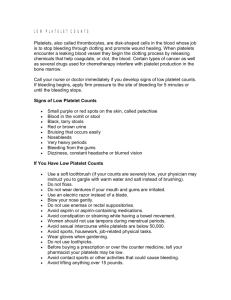
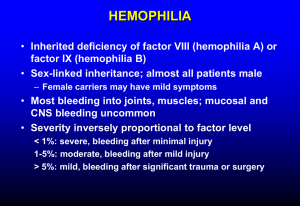
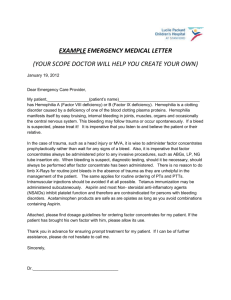
Outline • 1. Introduction • 2. Body • Hemostasis • Platelet disorder - Disorder of Plt function - Thrombocytopenia • Inherited coagulation disorder - Hemophilia - Von Willebrand Disease • 3. Conclusion Introduction • All materials from Wintrobe’s Clinical Hematology, 11th edition - Ch 51-59 Hemostasis • All component onset at same time and close at different time • Primary(3-5 mins to onset) – Vessel – Platelet • Secondary( 5-10 mins to onset) – Coagulation • Fibrinolysis( need 2-3 days to onset) How to D/D primary or secondary hemostasis Clinical Distinction between Disorder of Vessels and Platelets and Disorders of Blood Coagulation Finding Petechiae Deep dissecting hematomas Superficial ecchymoses Hemarthrosis Delayed bleeding Bleeding form superficial cuts and scratches Sex if patient Positive family history Disorder of Coagulation Rare Characteristic Common, usually large and solitary Characteristic Common Minimal 80-90% of inherited forms occur only in male patients Common Disorder of Platelets or Vessels Characteristic Rare Characteristic, usually small and multiple Rare Rare Persistent, often profuse Relative more common in females Rare ( Except vWD and hereditary hemorrhagic telangiectasia) acquired inherited 一定有 answer Drugs: Cpz, fortum, Usually acquired disease Trauma Hx( bone fracture) Also Consider mild deficiency of F VIII,IX,XI ( around sen 30-40%) and dysfibinogenemia Pts with mild bleeding disorder and normal aPTT; cause aPTT did not dected the mild deficiecy of F VIII,IX,XI Urea [5M] solubility test See You Symptom(+) Lab (+) and Sym(-) Condition with abnormal screening tests but no hemorragic diathesis Factor XII deficiency Prekallikrein deficiency High-molecular-weight kinogen deficiency Mild to moderate factor VII defiency Lupus anticoagulant Exscess citrate anticoagulant (eg with Hct >60%) Screen Lab: APTT, PT and PLt (-) (+) Confirmatory test mixted aPTT; mixed PT 0 and 2 hour If corrected (N+P < buffer+normal) Factor deficiency Or weak antibody If not antibody 1. Anti phospholipid Ab ( no clincal importance) on 0 hr 2. Factor antibody ex: VIII ab ( delay titier: 2 hr more long) if aPTT,PT,TT and Plt all is normal R/O F XIII problem check urea [5M] solubility test( clot stability test) : if abnormal F XIII resolution in minutes( hydrogen bond peptide bond by FXIII) Coagulation Factor (1) • All factor including protein C,S synthesis by liver cells except FVIII( endothelial cells) – Only Hypofibrinogen may rare from deficiency liver biosynthesis – Filling with vit K did not compensate the FII,VII,IX,X prove the hapatocyte cell inj in main cause • Half life – Shortest: VII(4-6 hr) – Longest: XIII 168hrI=frbrinogen (120 hr) Coagulation Factor (2) • Cofactor – V , VIII, tissue factor, HMWK, protein S, thrombomodulin, EPCR • • • • Protease : others Not in liver “cell” product: VIII Vit K dependent : II,VII,IX,X,C,S,Z Level newborn= adult – Factor I, V, VIII, XIII, vWF • Molecular weight – > 300K : factor I, V, VIII, XIII, vWF – < 50 K : Tissue factor, VII 1. A Jew patient had minimal bleeding tendency and occasional surgical bleeding since childhood, the most possible factor deficiency is (A) V (B) VIII (C) XI (D) XII (E) X Ans: C 2. Which of the following diagnosis may be compatible with the following coagulation profile: normal prothrombin time and platelet count, prolonged activated partial thromboplastin time ? (1) Deficiency or inhibitor of factor VIII, IX or XI (2) von-Willebrand’s disease (3) Heparin induced (4) Fibrinogen deficiency Ans: 1,2,3 3. Which the following coagulation factors has the longest in-vivo half-life? (A)factor II (B)factor V (C)factor VII (D)factor VIII (E)factor XIII Ans : E 3. A patient with congenital bleeding tendency, his APTT is normal, but PT is prolonged, which factor deficiency is most likely? (A) XII (B) XIII (C) VII (D) V (E) X Ans : C 4. Which of the following factor deficiencies would be expected to result in prolongation of both the prothrombin time and partial thromboplastin time ? (A) Factor XI (B) Factor X (C) Factor IX (D) Factor VIII (E) None of above Ans : B 5. If a patients has congenital factor XIII deficiency, which screening test is useful for detection? (A) Prothrombin time (B) Activated partial thromboplastin time (C) Urea solubility test (D) Euglobulin lysis test (E) Assay for fibrin degradation products Ans : C Disorder of Platelet Function 1. 2. 3. 4. 5. Adhension • Bernard soulier syndrome • Collagen receptor deficiency • Plt-type vWD Aggression • Galmzman’s thrombobasthenia Secreation • αgranule : gray plt syndrome • δgranule (dense) : storage pool disease, Hermansky-Pudlak syndrome, Chediak-Higashi syndrome, Wiskott- Aldrich syndrome, Thrombocytopenia and absent radii Acquired disorder • Drug induced : analgesics, antibiotics, cardiovascular drugs, psychotropic drugs • Uremia • Disorder of hematopoietic system: MDS, MPD, paraproteinemias Platelet procoagulant activity defect • Scott syndrome CD 41,61 CD 42 Bernard Soulier Syndrome • • • • • AR, chromosome 17 Defective Ib-IX complex ( second abundant plt receptor) Mucocutaneous bleeding Thrombocytopenia with giant platelet, prolong bleeding time Platelet aggregation test: – Ristocetin : failure – Other agonists ( ADP, collagen, epi) : normal – Low dose thrombin : may be delayed • Tx: local measure, hormonal management of menses, plt transfusion , DDAVP, factor VIIa, anti-Gp Ib-IX complex alloantibody Galmzman’s Thrombobasthenia • AR, chromosome 17 • Defective PLT integrin IIb-IIIa complex ( most abundant plt receptor) • Repeated mucocutaneous bleeding at early age • Normal PLT count , bleeding time prolong • Platelet aggregation test: – Ristocetin : normal – Other agonists ( ADP, collagen, epi, thrombin) : absence of secondary aggregation • Tx: PLT transfusion Storage Pool Disease • Hermansky-Pudlak syndrome (HPS) – AR, HPS-1 gene (10q) – Tyrosinase- positive, severe oculocutaneous albinism associated with photophobia, rotatory nystagmus , and loss of visual acuity – Excess accumulation of ceroid –like material in RE cell – Mild to moderate bleeding diathesis – Major cause of death: pulmonary fibrosis • Chediak-Higashi syndrome (CHS) – AR(1q) – Partial albinism : caused by abnormal large melanosomes – Large intracytoplasmic granules in leukocytes, lymphocytes, monocytes and platelets – Immune dysfunction : poor mobilization of marrow leukocyte pool, defective chemostaxis and bactericidal activity – Often die in first two decades of life : overwhelming infection or lymphoproliferative disorders Scott Syndrome • Platelet factor 3 activity – Activated platelets : as once of the principle sites for plasma coagulation reactions – Providing a surface on which coagulation factors complexes assemble, accelerating these reactions • Binding of factors Va-Xa and factors VIIIa-IXa complexes is impaired – Prolong bleeding after dental extractions or surgical procedures, spontaneous retroperitoneal hematoma – No increase bruising or bleeding from superficial cuts – BT, PLT morphology, aggregation and secretion, standard screening for PT and aPTT : normal – Dx : shorten serum prothrombin time due to prothrombin consumption decrease ( decrease thrombin generation) – Tx : PLT transfusion Thrombocytopenia • Pathophysiology and classification • Inherited platelet disorder : qualitative and quantitative • Immunologic platelet destruction • Nonimmunologic platelet destruction Inherited Platelet Quantitative Disorder • Pancytopenia (all AR, but DC XR) – Fanconi anemia – Dyskeratosis congenita (Zinsser-Cole-Engman syndrome) – Shwachman-Diamond syndrome – Pearson syndrome – Reticular dysgenesis – Congenital amegakaryocytic thrombocytopenia Congenital thrombocytopenia • • • • With megakaryocytic hypoplasia – Thrombocytopenia absent radii (TAR) (AR) – Thrombocytopenia with radioulnar synostosis and HOXA11 gene mutations (AD) Autosomal dominant giant platelet disorder (MYH9 gene defect) – May-Hegglin anomaly – Sebastian syndrome and variants – Fechtner syndrome – Epstein syndrome X-linked microthrombocytopenia ( WAS gene mutation) – Wiskott-Aldrich syndrome (WAS) – X-linked thrombocytopenia (XLT) X-likned macrothrombocytopenia with dyserythropoiesis (GATA1 mutation ) Congenital Amegakaryocytic Thrombocytopenia • AR, c-mpl gene (1p34) • Marked elevated thrombopoietin • Thrombocytopenia in infancy, pancytopenia later – – – – – – – Median age at diagnosis: 1 m/o S/S : bleeding in skin, mucous membranes or GI tract PLT count: not improved with age BM : normal cellularity with absence of megakaryocytes With or without birth defects Risk of development of aplastic anemia (40%) Median survival : 7 y/o • Treatment : SCT Thrombocytopenia Absent Radii (TAR) • AR • Diagnosis : usually at birth – Bilateral absence of radii with thumbs present(100%) – Hemorrhagic at birth : often petechiae, bloody diarrhea (60 % within first week) – Thrombocytopenia : < 50K/ μL (75%) – Normal BM cellularity, but absence of megakaryocytes • After infancy: very good prognosis – – – – Bleeding in infancy then improvement after the 1st year > 1 y/o : PLT > 100K/ μL Spontaneous remission : plateau of 75 % survival by 4 y/o Major case of death : ICH, GI bleeding • Tx: PLT transfusion Autosomal-Dominant Macrothrombocytopenia (MYH9 gene defect) • Ineffective thrombopoiesis: PLT 20K- 100k/ μL, Normal PLT survival and BM megakaryocytes. • Easily bruising early in life • MYH9 gene mutation (22q12.3-13.1) for nonmuscle myosin heavy chain Syndrome caused by MYH9 gene defects Syndrome May-Hegglin Sebastian Fechtner Epstein Macrothrombocytopenia Dohle-like bodies Yes Yes Yes Yes Yes Yes Yes No Nephritis No No Yes Yes Deafness No No Yes Yes Cataracts No No Yes No X-Linked Thrombocytopenia • X-linked microthrombocytopenia – WASp gene at Xp11.22p11.23 – Thrombocytopenia + small platelet (half size) + eczema + T-cell immunodeficiency – Normal or megakaryocyte mass – Increase destruction in spleen thrombocytopenia and decrease PLT size – Splenectomy definitely improves PLT counts in these pts, which frequently return to normal • X-likned macrothrombocytopenia with dyserythropoiesis – GATA1 transcriptional activator missense mutation (Xp 11.23) which is necessary for megakaryocyte differentiation – Different severities of disease, GATA1 with FOG result in most severe macrothrombocytopenia and anemia – D/D with WAS : normal PLT size, no immune abnormality, severity of bleeding 1. How can we measure the platelet adhesion function by checking? (A) Von Willebrand’s factor (B) ristocetin cofactor assay (C) GPIb/IX (D) fibronectin (E) platelet factor 4 Ans : C 2. Which one is correct in the platelet function disorders? (A) Secretion disorder-- Glanzmann thrombasthenia (B) δ-Granule abnormality -- Gray platelet syndrome (C) Adhesion defect -- Bernard-Soulier syndrome (D) α-Granule abnormality -- Hermansky-Pudlak syndrome Ans: C 3. Thrombocytopenia is least likely to be found in which of the following conditions? (A) Caused by anticoagulant-dependent immunoglobulin (B) Bernard-Soulier syndrome (C) Posttransfusion purpura (D) Glanzmann thrombasthenia (E) Hypothermia Ans: D 4. How dose the vascular system prevent bleeding ? (1) vasoconstraction (2) diversion of blood flow around damaged vasculature (3) initiation of platelet aggregation and fibrin formation (4) secrete hepatan sulfate Ans: 1,2,3,4 5. Which of the following disease is characterized by giant lysosomes in granulocytes, a picture of partial oculocutaneous albinism, and neuropathy associated with decussation defects at the optic chiasm? (A) Alder-Reilly anomaly (B) Chediak Higashi anomaly (C) Chronic granulomatous disease (D) Leukocyte adhesion deficiency (E) May-Hegglin anomaly Ans : B 6. Which condition can be associated with prolong bleeding time ? (1) Thrombocytopenia (2) Bernard-Soulier syndrome (3) von Willibrand disease (4) Sever hypofibrinogenemia Ans: 1,2,3,4 7. Which of the following medical conditions may indicate for the bleeding tendency ? (1) acute or chronic liver disease (2) myeloma or paraproteinemia (3) renal insufficiency (4) myeloproliferative disorders Ans: 1,2,3,4 8. Which disease(s) will cause platelet adhesion defects? (1) Bernard-Soulier Syndrome (2) Storage pool deficiency of platelet (3) Von Willebrand’s disease (4) Hemophilia A and B Ans : 1,3 ITP •By exclusion Dx , no identifiable underlying case • 2nd TP Table 53.1. Autoimmune Thrombocytopenia Purpura Idiopathic (primary) Secondary Infection Collagen vascular diseases Lymphoproliferative disorders Solid tumors Drugs Miscellaneous ITP • • • • • • Most common antigens: GpIIb/IIIa, Ib/IX Serum antiplt IgG autoAb : 50-85% S/S : GU bleeding, GYN menses bleeding < 50000: even trauma->no bleeding <10000: spontaneous bleeding ICH < 1 % ITP • Childhood is usually benign and self-limited – Plt > 30K and no clinical bleeding : observation only – Plt < 20K + significant mucous membrane bleeding or plt <10K with minor purpura – • • • • • Steroid increase plt at 1 wk , peak at 2-4 wk IVIG increase plt at 2 days , peak at 1 wk • Anti-D Chronic ITP ( > 6 months) : < 20 % Adult : spontaneous remission <5% , so need long term treatment <25% after DC prednisolone can long tern PR and CR(Plt>50000) After prednisolone – response in 1 wk peak in 2-4 wkskep Tx try tapping or DC in week 4 (CR or PR :83% child, 59% adult) – if no response in 1-2 wks try other treatment and splenectomy ITP • Indication of splenectomy – <10k and Poor response to steroid >6 weeks – <30K and poor response to steroid >3 months • CR to splenectomy : 50- 80% – Accessory spleen : 15-20% ( 50 % relapse) • Immunosuppressive drugs (for refractory case) – Cyclophosphamide (16-55% response) – Vincristine and vinblastine – Anti-CD 20 monoclonal Ab ( 50 % response) Treatment of ITP in Adults Approach Initial Refractory Bleeding Chronic refractory Treatment Notes Steroids (prednisone 1-1.5 mg/kg/d po tapered over wks vs.dexamethasone 40 mg po x 4d) Useful acutely, but long term s/e Fc receptor on Mɸ anti-plt Ab production Anti-Rh(D) Ig 75μg/kg/d IV For Rh(D) +pts Ab-coated RBCs overwhelm Mɸ Fc receptors IVIG(1g/kg/d IV x 2-3d) If plt <5000 despite steroids Blacks Fc receptors on Mɸ anti-plt Ab production Splenectomy Plt clearance Rituximab (anti-CD20) Plt clearance, Ab against B cell Danazol, vincristine Plt clearance Azathioprine, cyclophosphamide Immunosuppressants anti-plt Ab production AMG531,AKR-501, eltrombopag Thrombopoiesis stim. proteins Aminocaproic acid Inhibits plasmin activation Methylprednisolone 1g/d IV x 3d See above IVIG See above Autologous HSCT Investigational (NEJM 2002;346:995 &2003;349:831&2006;355:1672) Drugs Associated ITP • • Gold persisted for weeks to months 當懷疑有藥物引起血小板低下時,可藉由受疑藥品的停用 來加以証實,通常停用5─7天即可得到証實。一般若想了解 究竟是哪些藥物造成病患血小板低下,可參考一些發表過 的個案報告,以評估該病患之用藥與血小板低下之間的關 係究竟有多大。在報告過的個案中,最常見的是Quinidine、 Quinine、RIF以及TMP-SMX。 Heparin-Induced Thrombocytopenia Feature Type I Type II Mechanism Direct effect of heparin Immune(Ab)-mediated IgG vs platelet factor 4-heparin complex Incidence 20% 1-3% Onset After 1-4 d of heparin therapy After 4-10d; but can occur early (<24h)with history of prior exposure within last 100d ( felt to be secondary to persistent Ab) Can occur after heparin discontinue. Platelet nadir > 100,000/μl 30-70,000/μl, >50% Sequelae None Thrombotic events (HITT) in 3050% Rare hemorrhagic complications Management Can continue heparin and observe Discontinue heparin Alternative anticoagulation (lepirudin or arga) Neonatal Autoimmune Thrombocytopenia • Pathogenesis – Infant of mothers with immune thrombocytopenia ( ITP, SLE, or other autoimmune disorder) – Placental transfer of maternal antoAbs • Clinical features – Less severe than NAIT – Risk of ICH : 1% – Both neonate and mother have thrombocytopenia • Treatment – PLT < 40-50 K – IVIG, steroids • • Neonatal Alloimmune Thrombocytopenia ( NAIT) Incidence : 1/2000 births Placental transferof maternal alloAbs directed against paternally inherited Ags present on fetal platelets but absent from maternal platelets – Transient , isolated , severe thrombocytopenia – Platelet alloAgs • Human platelet antigen (HPA) 1a, 5b • HLA class I • Blood group ABH • Features – – – – – • Severe thrombocytopenia (< 10K) on the 1st day Petechiae (90%), hematoma (66%), GI bleeding (30%) ICH (15%): prenatal (50%), postnatal Normal maternal platelet counts Can occur in both the first and subsequent pregancies Dx: serologic or genotypic testing – Immunophenotyping of maternal, paternal, and neonatal PLT – Anti-PLT Ab in maternal or fetal serum (< 2/3) • Tx: PLT transfusion • PLT < 30K or clinically significant bleeding • Washed, irradiated, maternal platelets 1. Which of the following statements about ITP is wrong? (A) It is an autoimmune disease in most adult ITP (B) The effect of IVIG last about 3 weeks (C) Children present with acute ITP and usually with spontaneous remission (D) For chronic ITP, the goal of therapy is to maintain platelet count over 80,000/cmm (E) Splenectomy is indicated in patients with refractory ITP with bleeding problem Ans: D 2. For the first line treatment of a 16 years male suffered from ITP with platelet count < 10,000/mm3, which of the following is not appropriate? (A) close observation (B) corticosteroid (C) IVIG (D) Anti-D (E) Splenectomy Ans : E 3. Which statements about immune thrombocytopenic purpura (ITP) are correct ? (1) Rituximab is effective in certain portion of patients with refractory ITP failing to respond to steroid treatment and splenectomy (2) ITP is caused by autoreactive antibodies that bind to platelets and shorten their life span. However, antiplatelet antibodies are not detected in at least 20% of typical cases of ITP (3) The response rate to prednisolone varies from 60-90 % depending on the intensity and duration of treatment. It is unlikely that additional benefit is achieved by continuing prednisolone beyond 3-4 weeks (4) IVIG is helpful in achieving long term remission of ITP Ans : 1,2,3 4. Concerning with ITP, which description is wrong? (A) Splenomegaly is a rare manifestation in ITP (B) Oral prednisolone has 10-30 % of response rate to induce long-term remission for adult ITP, and has much higher rate for pediatric ITP (C) Laparoscopic splenectomy has 70-85% of response rate to induce complete remission for adult ITP (D) Rituximab ( anti-CD 20 monoclonal antibody) recently emerges as a new alternativc treatments for refractory ITP (E) IVIG treatment (1g/kg for 1-2 days ) has 50-80% response rate for adult refractory ITP, and its effect usually lasts for more than one month Ans : E 5. Heparin-induce thrombocytopenia (HIT) is a difficult complication while using heparin to treat deep vein thrombosis. Which of the following statement is NOT correct? (A) Approximately 70% of patients will develop thrombocytopenia begins 5 to 10 ays after heparin therapy (B) HIT is dose dependent (C) HIT can be treated with IVIG, plasmapheresis with success (E) LMWH is contraindicated as treatment for HIT Ans: B •Thrombotic microangiopathy •TTP •HUS •DIC TTP • • • • • • • Incidence: 1-4/ million Penta: fever, renal , thrombocytopenia, neuro (gray matter and brain stem), hemolytic anemia 74% with 3( plt, anemia, neuro), 40% with penta Most common symptom: fever , HA Reversible aggregation of platelets in microvasculature , brain, abdominal viscera and heart are most common site F/M=2/1, adult 30-40 y/o Gene HLA II DR35 Disease Associated with Thrombotic Thrombocytopenic purpua Infection : HIV, E. coli, Shigella Pancreatitis Drug treatment: cyclosporin A, tacrolimus, antineoplastic agents, ticlopidine, clopidogrel, quinine Collagen-vascular disease Pregnancy and the puerperium Cancer Bone marrow transplantation TTP • TTP • Vascular abnormality – TTP is a disease due to ADAMTS13 (metaoprotease) deficiency <10% most and increase ULvWF • Point mutation family deficiency(Upshaw-Shulman syn) • Antibody or inhibitor related (居多) – Overproduct (release) of ULvWFthen use off the ADAMTS13 – PAF(platelet aggregation agents) disclosed in blood : PAF37, calpain,3rd?? • FFP ( with protease in FFP) can treatment TTP • DDX: HUS normal protease level TTP-Diagnosis Hint • • • • • • • • PB smear : polychromasia , stippling, nucleated RBC, schistocytes LDH 400~ more than 1000 Unconjugated bilirubin HgB<10, ret , hepatoglobin , hemoglobiuria, hemosiderinuria Plt<100k, most <50,000 Coagulation : normal ( FDP may slightly ) Agarose gel : abnormal vWF multimers Skin, BM, gingiva Bx: hyaline thrombi within arterioles( but also in DIC, HUS, some vasculitis… no specific) • Brain CT : reversible brain edema, ischemic strokes , and frank hematoma • Sensitive indices of the response to therapy : LDH level and platelet count TTP D/D • HUS – Microangiopathic blood destruction and vascular damage occur principally in kidney – High In child with prodromal infection – Abdominal pain, GI s/s, anuria, several renal failure and hypertension are common in the early course – Neurologic symptom are less common – C’ low, most self remission and relapse is rare • HELLP(pregnant female;eclampsia; hemolysis;elevated liver enzyme; low plt count) • SLE woth immune TTP • Vasculitis • PNH • TTP+AIHA Treatment of Thrombotic Thrombocytopenia Purpura Plasmaphresis with exchange at least one volume of plasma daily Inclusion of antiplatelet agents and corticosteroids is of unproven benefit Salvage therapy Infusion of fresh frozen plasma Plasmapheresis and exchange with cryosupernatant plasma Vincristine IVIG Splenectomy Prostacyclin •Plasma exchange should be several days after the plt is normal and minimal hemolysis •1/3 relapse after CR in 1 month •No PLT BT ( deterioration renal and neuro status) •Some people with chronic, relapsing TTP have responded to splenectomy Hemolytic-Uremic Syndrome • Annual incidence: 1/100,000 • Most often in infants and young children – Most common cause ARF in this age-group • Most common cause : acute infection – Shiga-like toxin ( EHEC O 157: H7) – Capillary thrombosis and ischemic necrosis: kidney ( most severe) , GI, CNS and other organs • Clinical features: • • • • • Usually following an acute diarrhea illness Non-diarrhea HUS ( atypical ) : 10 % Usually ARF Hemolytic anemia , thrombocytopenia : less severe than TTP Laboratory DIC : usually not present • Treatment : supportive 1. Which statements about thrombotic thrombocytopenic purpura is correct ? (1) Inhibitory antibodies against von Willebrand factor-cleaving protease occur in patients with acute thrombotic thrombocytopenic purpura (2) Detected in the plasma of patients with TTP (3) Deficiency of ADAMTS13 has been reported consistently in patients with TTP. Such defect may be constitutive, due to homozygous or double heterozygous mutations in the corresponding gene, or acquired, due to the presence of circulating inhibitory antibodies (4) ADAMTS13 is an inhibitory antibody against von Willebrand factor-cleaving protease Ans:1,2,3 2. A 72-year-old man, had a flu-like symptoms 2 weeks ago, started to have fluctuation of consciousness, skin ecchymosis, low grade fever, decreased urine amount, was sent to emergent service due to deterioration of consciousness disturbance. On PE: BP 136/82 mmHg, PR 112/min, regular heart beat, consciousness very drowsy, mild fever 37.9 oC, Blood tests: WBC 12300/ul, mild neutrophilia, Hb 8.3 g/dl, MCV 92 fl, Platelet 18000/ul. PB smear: marked thrombocytopenia, apparent RBC fragmentation, no blast. Serum Cr: 3.8 mg/dl, LDH 680 U/dl (high). Normal PT/aPTT. Under this situation, which of the following managements is (are) appropriate (1) Emergent hemodialysis for rapid deterioration of renal function (2) Aggressive transfusion of platelet concentrate to keep platelet count >50000/ul (3) High dose parenteral steroid, e.g. methylprednisolone as pulse therapy (4) Infusion of fresh frozen plasma (FFP), or exchanging plasmaphoresis if available Ans: 4 3. A 19-year-old female patient is a case of systemic lupus erythematosus (SLE) with normal renal function before. She suffered from abdominal pain and watery diarrhea for a few days. Sudden onset of oligouria with black urine and exertional dyspnea occurred later. Laboratory data showed WBC 1800/ul, Hgb 5.0g/dl, PLT 30000/ul; both direct and indirect Coombs’ test: negative; haptoglobin: very low; bilirubin 2.4 mg/dl; BUN/ Creatinin 130/7.0 mg/dl; stool culture: O157:H7 E. Coli. Blood smear displaced many fragment of erythocytes. What kind of disease is most likely? (A) Thrombotic thrombocytopenic purpura (B) Hemolytic-uremic syndrome (C) Disseminated intravascular coagulation (D) Autoimmune hemolytic anemia (E) Paroxysmal nocturnal hemoglobinuria Ans: B 4. Which of the following laboratory results may be presented in patients with hemolytic uremic syndrome ? (1) Microangiopathic hemolytic anemia (2) Renal failure (3) Thrombocytopenia (4) Abnormal screening test of coagulation Ans : 1,2,3 5. The most common cause of idiopathic thrombotic thrombocytopenia purpura ( TTP) is: (A) Drugs such as mitomycin, cyclosporin, etc (B) Autoantibody to ADAMTS 13 (C) ADAMTS13 gene mutation (D) Shiga toxin (E) Transplantation Ans : B 5. Which of the following about TTP is wrong ? (A) The best treatment is plasma exchange (B) The diagnosis is based on the exclusion of other disease that might cause microangiopathic hemolytic anemia (C) Coagulation studies are usually abnormal (D) TTP is due to vascular endothelial injury with release of unusually large vWF (E) Idiopathic TTP is an immune disorder Ans : C 6. About “Hemolytic Uremic Syndrome” (HUS) , which of the following statements is (are) correct? (1) One of the clinical expressions of schistocytic hemolytic anemia (2) Usually has severe thrombocytopenia (3) Most frequently associated with the infection by verocytotoxin producing microbes (4) The role of plasma therapy in HUS is less certain as in patients with TTP ( thrombotic throbocytopenia purpua) Ans: 1,2,3,4 7. Plasma exchange is the choice of treatment for thrombotic thrombocytopenic purpura. If patient has response to plasmapheresis, which three parameters are the early signs of good response? (1) Nonfocal neurologic symptoms, such as mental status changes (2) Serum LDH levels (3) Thrombocytopenia (4) Renal failure Ans: 1,2,3 Hemophilia Hemophilia • Incidence: 1/5000 male – 80-85% : hemophilia A ( factor VIII deficiency) – 10-15% : hemophilia B ( factor IX deficiency) – 1/1 million :hemophilia C ( factor XI deficiency) (Jews 5- 11%) • X-linked recessive ( Xq) – Hemophilia A gene: Xq28, most common intron 22 inversion ( 45%) – Hemophilia B gene: most common missense point mutations (>60%) , spontaneous mutation rate is low s – 1/3 : new mutations • • • 1 unit =the amount of factor found in 1 ml of normal plasma 100% activity (100 unit/dL)= the activity of factor found in 1 ml normal plasma Hemophilia in female – – – – – Skewed lyonization of a carrier female Testicular feminization of a genotypic male Turner syndrome (XO) A daughter of a maternal carrier and a father with hemophilia A Type 2N VWD ( mutation in factor VIII-binding region of VWF protein) Hemophilia • Hemarthrosis – Major long-term disabling complication – Most common affected joint : ankles (toddler), knees and elbows (older child) – arthropathy: • Synovitis : normal ROM, proximal muscle weakness • Arthritis : cartilage erosion , crepitus, ROM , proximal muscle weakness • Chronic hemophilic arthropathy : joint fusion and narrowing of joint space – Prophylactic therapy: 20-40 unit/kg factor VIII qod or three times a week to keep nadir > 1% • Primary: limit the develop of target joint • Secondary : cool down the affected joint • Intramuscular hematoma: often elusive – Iliopsoas bleeding: lift threatening – D.D. with hip hemarthrosis: unable hip extension, normal hip joint internal and external rotation • GI and GU bleeding • Traumatic bleeding : delayed bleeding is common Hemophilia • Hemarthrosis with significant orthopedic disability is rare in pt with coagulation disorder other than hemophilia A and hemophilia B. • Hemophilia C: hemarthrosis is uncommon, often delay bleeding after trauma and surgery or menorrhagia, associated with Noonan syndrome and Gaucher disease. • Dx: PTT prolong, PT normal ( also factor XI, factor XII, prekallikrein, HMWH deficiency, but latter three not associated with excessive clinical bleeding) • Mild form patient may have normal PTT value. • Type 2N vWD: – Indistinguishable from mild hemophilia A. – AR family history – Confirmatory test for vWD Hemophilia Treatment • Hemophilia A – Recombinant factor VIII concentrates, cryoprecipitate – Dose(units)= desire rise level (%) x BW (kg) x 0.5 – Half life : 10-12 hrs • Hemophilia B – Recombinant factor IX concentrates, FFP – Dose(units)= desire rise level (%) x BW (kg) – Half life : 18-24 hrs • DDAVP – Increase plasma factor VIII and vWF mild and moderate hemophilia A , type 1 vWD – No effect foe severe hemophilia A , severe vWD, any form of hemophilia B, life-threatening hemorrhage Initial Treatment of Specific Hemorrhages in Hemophilia Type of hemorrhage Hemophilia A (units/kg factor VIII concentrate) Hemophilia B (units/kg factor IX Hemarthrosis 20-50 30 Muscle or subcutaneous hematoma 20 30 Tooth extraction 20 30 Epistaxis 20 30 Major surgery, life threatening hemorrhage 50-75 80 Iliopsoas hemorrhage 50 80 Hematouria Bed rest; 20 Bed rest; 30 concentrate) Hemophilia – Factor VIII (or IX) Inhibitor • Severe hemophilia A : 14-25 % (occur average 9 days later) • Bethesda assay – 1 Bethesda unit: the amount of antibody that will inactive 50% of the normal factor VIII( or IX) in 2 hrs when the residual factor VIII( or IX) level is between 25-75 % – 1:10 dilution of test plasma has this effect -> 10 Bethesda unit • Low responder – Ab titer < 5 B.u – High-dose factor VIII concentrates and routine inhibitor assay • High responder – Ab titer > 5 B.u – anamnestic response – Tx: • • • • • Continuous factor VIII infusion Porcine factor VIII concentrate Recombinant factor VIIa Prothrombin complex concentrate Activated prothrombin complex concentrates ( Autoplex T, FEIBA) Hemophilia – Factor VIII (or IX) Inhibitor • Long-term management – High dose factor VIII: immune tolerance induction – Intravenous -globulin – Immunosuppressive therapy: cyclophosphamide, prednisolone – Remove of antibody by extracorporeal immunoadsorption of Staphylococcus protein A columns 1. Long term prophylaxis of bleeding in patients with severe hemophilia A is important. Which of the following is (are) correct? (1) Recombinant factor has definite lower incidence of inhibitor production (2) The dose of coagulation factor should be optimal, based on individual requirement. (3) Recombinant factor is more effective than plasma product (4) The prophylaxis period should be indefinitely, as long as patient needs Ans : 2, 4 2. A 4-year-old boy with and intramuscular hemorrhage that developed 3 days after accidentally being hit by his brother with a bat. He has never suffered from spontaneous bleeding. His maternal uncle dropped out of the army because he experienced more bleeding events than expected. Physical exam is unremarkable except for a swollen, painful right quadriceps muscle. The platelet count, PT, and APTT are normal. The most likely diagnosis is: (A) Mild hemophilia B (B) inherited platelet defect (C) Mild hemophilia A (D) Factor XIII deficiency (E) Dysfibrinogenemia Ans : A 3. About coagulopathy, which of the following statement is correct? (1) Henophilia A is a disorder of Factor VIII deficiency, it is inherited by X-linked recessive (2) One unit per kilogram factor VIII transfusion can raise the plasma factor VIII by 1 % (3) The half-life of Factor IX is about 24 hrs (4) The half-life of Factor VIII is about 24 hrs Ans : 1,3 4. Which of the following products may be considered as therapeutic agents for the patients of hemophilia A with inhibitor ? (1) High dose factor VIII concentrates (2) Activated prothrombin complex concentrates (3) Porcine factor VIII (4) Recombinant factor VIIa Ans : 1,2,3,4 5. For a case of severe hemophilia A complicated with iliopsoas muscle hematoma, which minimal plasma level of FVIII should be kept at the initial treatment stage? (A)15% (B)40% (C)60% (D)80% (E) 120% Ans : D 6. A 11 y/o girl had easy nasal bleeding before. She had lifethreatening bleeding at her menarche. Laboratory data revealed PT 45.2’’, aPTT 32.0’’ and platelet count 374,000/cumm. Which of the following treatments is relatively suitable for this patient? (A)cryoprecipitate (B)Promthrombin complex concentrate (C)Recombinant factor VIII (D)Recombinant factor IX (E)DDAVP Ans: B Von Willebrand Disease • Large , multimeric glycoprotein • Act in coagulation – Bridges together plt with vascular subendothelium (Gp IbIX) – FVIII carrier protein • Synthesis in megakaryocytes and endothelial cells • Stored in Weibel-Palade body (endothelial cell) and granule (platelet) Von Willebrand Disease • The most common bleeding disorder – Incidence: 1 % – Genetic : chromosome 12 (p13.3) ,usually AD, AR ( 2N, 3 and rare 2A ) – Blood group O vWF( 30% lower than other group) – vWF elevated in stress, pregnancy and trauma • Clinical presentation – Excessive bruising , menorrhagia, trauma induced mild to moderate bleeding , hemarthrosis ( type 3) Von Willebrand Disease-Screen Test • • BT, aPTT “vWF immunoassay(Ag)” • • “Ristocetin cofactor activity” • • • • If VWF ok and decrease FVIIIc2N Plt aggression test ( LD-RIAP) • • • single most sensitive and specific test binding of VWF to Gp Ib receptor on platelet discrepancy between “vWF function” and “vWF ag “provide : qualitative disorder “F VIIIc” • • quantitative immunoelectrophoretic assay Pt’s platelet(ristocetin induced) To DDx of 2B and plt-type from others Multimer studies 1994 Classifications of VWD 1994 Term 1994 Definition Genetics, Comment Type 1 Partial quantitative deficiency Dominant with variable expression; phenotype influenced by multiple genes Type 2 Qualitative defect Type 2A Decreased platelet-dependent function with absence of largest multimers Dominant Type 2B Increased VWF affinity for platelet GPIb Dominant. May be associated with thrombocytopenia, especially after DDAVP Type 2M Decreased platelet-dependent function with presence of largest multimers Dominant Type 2N Decreased VWF affinity for FVIII Recessive, often mistaken for mild-moderate hemophilia A Type 3 Virtually complete deficiency Recessive: homozygous or doubly heterozygous Platelet-type (pseudo-VWD) Not a defect of VWF, not to be considered a form of VWD Dominant. A platelet disorders: increased affinity of platelet GPIb for VWF. Thrombocytopeinia may be present. normal Type 1 Type 3 Type 2A Type 2B Type 2N Type 2 M PT-VWD BSS VWF:Ag N absent N or or N N VWF:Rco N absent N or N FVIII N or N 1-3% N or N or N N N RIAP N often normal absent often normal N N absent LD-RIAP absent absent absent absent absent absent absent Platelet count N N N N N N DDAVP VWF con VWF conc VWF conc VWF conc VWF conc VWF conc platelets platelets Response DDAVP good none poor decrease platelets poor poor decrease platelets none or poor Response to VWF conc good good good good good good decrease platelets none Frequency 1-2% very rare 1:250,000 rare rare rare rare rare rare N variable abnormal, presence of small multimers or absent multimers absence of large and intermedi ated- size multimers absence of large multimers N N reduced, caused by “consumpti on” by platelet normal Usual Tx Multimers N (DDAVP) (DDAVP) Management • Education • Cryoprocipitate (dose: desired rise level % × BW × 0.75) BT with vWF and F VIII at same time ( or need 8-12 hr to work) • DDAVP for type 1 – not for type 3, not for 2A, 2B • Amicar (antifibrinolytic agent) for mucosal bleeds • Humate-P (factor 8 and vWF) for surgery, trauma • Platelet for pseudo-vWD • Recombinant factor 7a, correct underlying disorder (hypothyroidism) for acquired vWD 1. A patient suspected with von Willebrand disease (vWD and) had a normal level of vWF antigen but reduced vWF activity. Which of the following subtype is matched the above pattern of test results? (a)Type 1 vWD (b) Type 2A vWD (c) Type 2N vWD (d ) Type 3 vWD (e) Platelet-type vWD Ans : b 2. Which of the following statements about von Willebrand disease (vWD) are correct? (1) Patients with blood group O have vWF levels that are on average 30% lower than patients with blood group A, B, or AB (2) Patients with pseudo-vWD have a genetic defect resulting in increased affinity of GpIIb-IIIa (3) Patients with type 1 vWD have concordant reduction of vWF:Ag and vWF:Rco (4) Patients with type IIb vWD have best response to DDAVP Ans: 1,3 3. Which of the following laboratory results would be useful for the diagnosis of vWD? (1) Prothrombin time (2) Assay for factor VIIIc and vWF (3) Clot retraction time (4) Ristocetin cofactor activity Ans : 2,4 4. Which of the following about von Willibrand’s disease (vWD) is correct ? (A) in type I vWD, the level if von Willebrand factor ( vWF) is decreased (B) the coagulation defect cannot be corrected by DDAVP infusion (C) the levels of vWF in a normal woman always remain constant and are not affected by menstrual cycle (D) in type III vWD, the level of von Willebrand factor is normal but the functional activity is reduced (E) the most common presentation of vWD is the unexplained thrombocytopenia Ans: A 5. The response to DDAVP is usually predicted to be effective in the following subtypes of vWD: (1) type 3 Ans : 4 (2) type 2B (3) type 2M (4) type 1 6. Which of the following factors can affect vWF level ? (1) sex (2) age Ans : 1,2,3,4 (3) ABO blood type (4) exercise 7. Which of the following subtypes of vWD is the most easily mistaken for hemophilia: (A) type 1 (B) type 2A (C) type 2B (D) type 2M (E) type 2N Ans : E 8. The statements are true, except (A) von Willebrand factor (vWF) is a large multimeric plasma protein composed of subunit polypeptides (B) vWF has no known enzyme activity (C) vWF functions as a carrier protein for factor VIII (D) vWF is not necessary for normal factor VIII survival in vivo (E) The normal function of vWF in platelet plug is apparently dependent on the assembly of this protein into large multimers Ans: D 9. A 22-year old woman is referred for the evaluation of menorrhagia. She has frequent problems with heavy mens and nosebleeds, and also has gun bleeding after minor dental surgery. She uses no medications regularly, but dose take aspirin for menstrual cramps. She states that her mother and two maternal aunts have similar problems, and one aunt had a hysterectomy at age 30 to control her menorrhagia. The laboratory tests show : Platelet count 345,000/uL Platelet aggregation normal to ADP, epinephrine and collagen, absent with ristocetin Bleeding time(Ivy) 21 minutes Partial thromboplastin time 39 seconds Prothrombin time 10 sec.( control= 10.5) Factor VIII coagulant activity 43 % Factor VIIIR Ag 20 % The most likely diagnosis is : (A) Glanzmann’s thrombasthenia (B) Bernard-Soulier syndrome (C) Type I von Willebrand’s disease (D) Platelet dysfunction caused by aspirin ingestion (E) vascular purpura Ans : C 10. Which statements about von Willebrand’s disease (vWD) are correct ? (1) vWD is inherited in an autosomal manner (2) The diagnosis is established by finding reduced plasma levels of vWF activity, vWF: Ag, or factor VIII, or a prolonged bleeding time (3) Partial thromboplastin time is often normal in vWD (4) Analysis of the multimeric composition of vWF is required for subtyping of vWF but is not helpful in choosing optimal therapeutic agents Ans: 1, 2, 3 11. The response to DDAVP is usually predicted to be effective in the following subtypes of vWD? (1) type 3 (2) type 2B (3) type 2M (4) type 1 Ans : 4 12. If a reproductive-age women with menorrhagia of unknown cause, the percentage of inherited bleeding disorder will be: (A) 5-10% (B) 10-25 % (C) 20-30 % (D) 30-40 % (E) 40-50 % Ans : B 13. von Willebrand factor is normally found in (1) plasma (2) endothelial cells (3) subendothelial space (4) megakaryocytes Ans: 1,2,3,4