What are the next steps?
advertisement

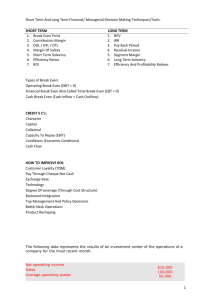
Commissioning for Value 1 key objective + 3 key phases + 5 key ingredients = COMMISSIONING FOR VALUE OBJECTIVE - Maximise Value (individual and population) Five Key Ingredients: 1. Clinical Leadership 2. Indicative Data 3. Clinical Engagement 4. Evidential Data 5. Effective processes 2 Granularity Populations CfV Pack Atlas Programme Budgets Where to Look 3 Systems Deep Dive Individuals SDM Care Planning Provider Pathway What to Change Manage care out of hospital How to Change The NHS Atlases of Variation Reducing unwarranted variation to increase value and improve quality Awareness is the first step towards value – If the existence of clinical and financial variation is unknown, the debate about whether it is unwarranted cannot take place ‹#› Clinical & Financial Variation • When faced with variation data, don’t ask: • How can I justify or explain away this variation? • Instead, ask: • Does this variation present an opportunity to improve? • Deep dive service reviews support this across whole programmes & systems and deliver Phase 2: • What to Change 6 NHS RIGHTCARE Partners and Stakeholders Case Outlines Mechanism Miscellaneous Decision (e.g. Commissioning Annual Plan) Process 7 Contracts Implementation Governing Body Reform Proposals Full Business Case Public Engagement Reform Ideas GP Member Practices Ideas Decision Group Clinical Policy Development and Research Decommissioning Clinical Executive Group HEALTHCARE REFORM PROCESS Service Reviews Procurement Primary Care Development Service Review Pathway – Diagnostic steps Step 1 – define: CURRENT SERVICE 8 Step 2 – define: Step 3 – Step 4 – categorise: recommend: FitFit forfor Purpose Purpose Maintain Efficiency andand market market options options Redesign, Contract, Procure Supply Supply andand capacity capacity options options Contract, Procure, Divest No/ low benefit Divest FUTURE OPTIMAL SERVICE Galvanising Clinicians – On the right things Number of Circulatory indicators in the bottom quintile of the practice cluster Each coloured bar represents a different set of indicators e.g. dark blue is prevalence. The specific indicators are then shown in the table on slides 21-27 for the 3 practices with the highest total number of indicators in the bottom quintile 1 Note, some of the data are based on small numbers. Statistical significance has not been tested and should not be inferred. The data are presented to identify potential areas of improvements rather than providing a definitive . comparison of performance 9 Easy answers in Secondary Care? • Diagnostic Atlas • %age stroke patients undergoing brain imaging within 1 hour of arrival at hospital, by hospital • • • • • 10 80th %ile Fairfield NMGH MRI Royal Oldham - 55% 43% 32% 7% 4% Secondary Care • Diagnostic Atlas • %age stroke patients undergoing brain imaging within 24 hours of arrival at hospital, by hospital • • • • • 11 80th %ile Fairfield NMGH MRI Royal Oldham - 98% 96% 91% 81% 94% Heart disease pathway = 95% confidence intervals Initial contact to end of treatment NHS Bradford City CCG Bradford’s focus on optimal system and value - CVD Population Prevention Individual Risk Factor Management and Prevention L-term RoI S- and mterm RoI Chest Pain Atrial Fibrillation Heart Failure S-term RoI M-term RoI M-term RoI Embed and use the tools of delivery – business process, service specifications and protocols, contract management, monitoring, support and managing pathways 13 AID - Adopt, Improve or Defend: Clinical protocols viability assessment and prioritisation 1. Research and collate clinical referrals protocols – start with Vale of York CCG’s - www.valeofyorkccg.nhs.uk/rss 2. Gather impact assessment group (IAG), comprising reform lead, clinical lead and finance lead. 3. IAG - follow initial impact assessment process (next slide) 4. Assess appropriate protocols against locally determined criteria – e.g. use reform decision tree 5. Adopt, or Improve and adopt, dependent on prioritisation – N.B. base the financial prioritisation on collated impact Initial Impact Assessment process Is the protocol deemed clinically appropriate for local use? Yes Are new pathway steps required to be implemented locally? No Will it reduce demand and/ or more complex/ costly treatment? No Yes Yes Can amendments be made to make it so/ optimise it for local use? Describe new pathways steps Collate impact and process through decision tree Yes Make amendments Pass to reform team to work up initial viability assessment Ideas & Cases Are there any health benefits? No Do not proceed Rate of Return <12 months High Priority RoI* >£250k Medium Priority RoI* >£100k Yes Low Priority RoI* <£100k Is it a must do? Yes* No Does it save money? No High Priority RoI* >£500k Rate of Return >12 months No Does it increase value*? Yes Prioritise Yes Yes Can it be delivered? No Yes Can it be made deliverable? Medium Priority RoI* >£250k Low Priority RoI* <£250k *See additional slides at end No Do not proceed Set Timetable for completion of case outline* Decision Tree for prioritising reform proposals 6 steps to an optimal urgent care front end system • 1. Operate robust Ambulatory Care protocols • 2. Care home education and training • Manage in home, reduce admissions • 3. Advanced Paramedic Practitioner • 1 WTE = >£1m impact on frequent callers per CCG • Supports Parity of Esteem • 4. Commissioner/ Primary Care-led A&E triage • Only way in to A&E is via triage, unless ‘major’ • Triage to MDTs and UCC/ H@H • Divert unnecessary urgent care • 5. Multi-Disciplinary Teams for key care areas (Respiratory, CVD, Diabetes, Dementia, etc) • Detect, divert and begin case management • 6. Urgent Care Centre/ Hospital @ Home • Provide less complex alternative for ‘minors’ 17 Bury priority: Mental Health 18 Bury priority: Mental Health 19 Phase 3 – How to Change • Behaviour, culture and leadership development • Attitude to implementation • Delivery levers, contract and market management Service specifications, CQuINS, PDAs and contract clauses; Referrals management (reactive Vs proactive, pathway aides) • Market management - 4 steps to buying optimal (in order of ease) Agreement, negotiation and persuasion (current provider improves willingly); Contract management (make them do it); Using current market options (encourage price and quality competition), and; Creating new market options (AQP, Tender, etc) ‹#› Leadership - Not for the fainthearted • BPE for improvement is designed to: • Make you look for problem areas (and face entrenched views) • Make you fix them (no matter how hard) • Highlight and deal with blocks in progress (including when important people/ stakeholders) • Doesn’t allow you to shy away 21 Change behaviours - Change is inevitable • Choice ≠ Whether to change • Choice = Whether to change yourselves or wait to be changed • People and Organisations who wait to be changed lose control, become resistant and block improvement 22 Patient Decision Aids – Implementation Process 1. Identify best 6 PDAs for local impact • Use DD, CfV, AoV, PLCV, local enthusiasm, etc 2. Localise with local GP lead and add referrals criteria and protocols • C. 50% of unwarranted activity dealt with by PDAs, 50% by protocols 3. Implement in key practices and prove impact 4. Spread across practices 5. Implement next 30 PDAs (in phases or collectively) 6. Implement International best practice Optional (innovative): 7. Design own, use and spread 23 Leadership behaviour - Not for the fainthearted • NHS RightCare is designed to: • Make you look for problem areas (and face entrenched views) • Make you fix them (no matter how hard) • Highlight and deal with blocks in progress (including when important people/ stakeholders) • Doesn’t allow you to shy away 24 Everyone gets to be Homer… Which Homer are you? Homer 1 (The Iliad) “Give me a place to stand and I will move the earth.” Homer 2 (The Simpsons) “Trying is the first step to failure” 25 World’s 1st change management guru – “To avoid criticism say nothing, do nothing, be nothing” Aristotle, c.350BC 26 Typical CCG embedding process • • • • • • • 27 Get buy-in and mandate from • Key leaders (AO, GP Chair, CFO) • Wider group (Gov Body, Clinical leads, SMT, GP forums) Demonstrate to wider stakeholders (Provider managers and clinicians, local PH, HWBs) Work with senior leads – BPE, Templates, Decision criteria, DT, governance structure and local guidance to support Whilst also progressing Where to Look (can include “quick win pre-What to Change phase” for the financially challenged) Support deep dive service review, evidence-building, case for change development, decision-making Whilst also developing delivery skills in preparation Build improvement capability – BI, programme office, project management, leadership resilience, contract management knowledgebase, delivery lever identification and use