Hereditary Breast/Ovarian Cancer
advertisement

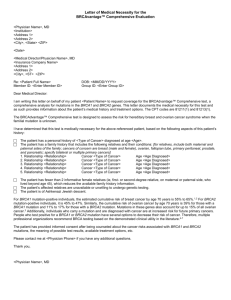
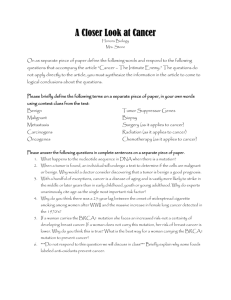
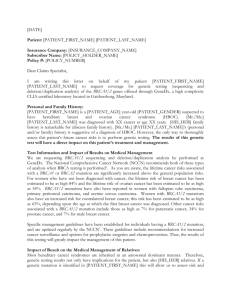
Hereditary Breast/Ovarian Cancer Prepared by: June C Carroll MD, CCFP, FCFP Sydney G. Frankfort Chair in Family Medicine Mount Sinai Hospital, University of Toronto Andrea Rideout MS, CGC, CCGC Certified Genetic Counsellor Project Manager – The Genetics Education Project Funded by: Ontario Women’s Health Council Version: March 2009 Acknowledgments Reviewed by: Members of The Genetics Education Project Funded by: The Ontario Women’s Health Council as part of its funding to The Genetics Education Project * Health care providers must use their own clinical judgment in addition to the information presented herein. The authors assume no responsibility or liability resulting from the use of information in this presentation. Outline Sporadic versus familial cancer Hereditary breast cancer syndromes Referral guidelines Benefits, risks and limitations of genetic testing Management Cases Cancer All cancer involves changes in genes…. Threshold effect: During mitosis & DNA replication mutations occur in the cell’s genetic code Mutations are normally corrected by DNA repair mechanisms If repair mechanism or cell cycle regulation damaged Cell → → accumulates too many mutations reaches ‘threshold’ tumor development Sporadic Cancer All cancer arises from changes in genes…. But NOT all cancer is inherited Most breast cancer is sporadic ~ 80% Due to mutations acquired over a person’s lifetime: Cause unknown – multifactorial Interaction of: age environment, lifestyle (obesity, alcohol), chance, unknown factors Sporadic cancer generally has a later onset Clustering of Cancer in Families 11% lifetime risk of developing breast cancer ~20% of women with breast cancer have a family history: 10 -15% of breast cancer is familial: Due to some factor in the family Environmental Undiscovered gene mutation Chance Generally not eligible for genetic testing 5-10% of breast cancer is hereditary: Caused by an inherited gene mutation which causes increased risk for cancer Variety of cancer syndromes About 2/3 of these - BRCA 1 or BRCA 2 mutations May be eligible for genetic testing Proportion of Hereditary Breast Cancer Familial 10-15% Hereditary 5-10% Sporadic 80% Knudson ‘two-hit’ Model Sporadic Cancer ONE HIT (hit=mutation) Birth: Two non-mutated copies of the gene SECOND HIT One mutation in one gene; Second gene non-mutated CANCER Two mutations - one in each gene Knudson ‘two-hit’ Model Hereditary Cancer ONE HIT (hit=mutation) Birth: Two non-mutated copies of the gene SECOND HIT One mutation in one gene; Second gene non-mutated CANCER Two mutations - one in each gene Compared to sporadic cancer, people with hereditary cancer have… A higher risk of developing cancer A younger age of onset of cancer Generally Multiple < 50 years of age primary cancers Hereditary cancer is less common in the general population than sporadic cancer Genes involved in hereditary breast/ovarian cancer > 2,600 mutations in: BRCA1- chromosome 17 BRCA2 - chromosome 13 Autosomal dominant transmission Carrier frequency of BRCA1& 2 mutations – 1/1,000 in general (Caucasian) population 1/40 - 1/50 in Ashkenazi Jewish people ~1/500 3 common mutations in Ashkenazi Jews Unique French Canadian mutations Autosomal Dominant Inheritance Legend Normal BRCA genes BRCA mutation Bb bb Bb Susceptible BRCA gene bb Population Risk Bb Susceptible BRCA gene B: BRCA gene with mutation b: normal BRCA gene bb Population Risk BRCA1 and BRCA2 What happens when their function is compromised ? Both genes are tumor suppressors: Regulation of cell growth Maintenance of cell cycle Mutation leads to: Inability to regulate cell death Uncontrolled growth, cancer Consequences of having a BRCA mutation: Estimated cancer risk by age 70 Breast Cancer ♀ BRCA Mutation Carriers In General Population 50-85% 11% 40-60% 1-2% 10-20% 1-2% ≤6% Rare BRCA1 & BRCA2 Ovarian Cancer BRCA1 Ovarian Cancer BRCA2 Breast Cancer ♂ BRCA2 Who should be offered referral for genetic counselling and/or genetic testing?.... Multiple cases of breast or ovarian cancer on same side of family, especially in closely related relatives in more than one generation when breast cancer is diagnosed before age 50 A family member with breast cancer diagnosed before age 35 A family member with both breast and ovarian cancers An Ashkenazi Jewish heritage, particularly with relatives with breast or ovarian cancer …Who should be offered referral for genetic counselling and/or genetic testing? A family member with primary cancer in both breasts (especially if before age 50) A family member with ovarian cancer A family member with male breast cancer A family member with an identified BRCA1 or BRCA2 mutation USPSTF 2005 recommends referral for genetic counselling and evaluation for BRCA testing to women with family history indicating increased risk of BRCA mutations Case: Rachel Rachel - healthy 40 year old Concerned about her risk for cancer Family history of both breast & ovarian cancer Case: Rachel’s family history LEGEND Breast cancer Ov Ca Died 48 Ovarian cancer Br Ca Dx 38 Br Ca Dx 30 Ov Ca Dx 40 RACHEL age 40 Rachel was referred to genetics… A genetics consultation involves: Detailed family history information Pedigree documentation Confirmation of cancer history: pathology reports/death certificates Medical & exposure history Empiric risk assessment Hereditary cancer / genetic risk assessment Psychosocial assessment Psychological Aspects to Consider Motivation for genetic testing: Reduce uncertainty Learn about risk for children Childbearing/marital decisions Explore further surveillance/treatment options Perceived risk Expectations of genetic testing Psychological well-being – current & past prior experiences with cancer prior loss/ disruptions associated with cancer approaching age of parent’s diagnosis or death from cancer A genetics consultation involves: Assessment of eligibility for genetic testing risk of a mutation must be ≥10% for most provincial programs Most appropriate family member to test first Estimated Discussion of risks, benefits & limitations of test Testing and disclosure of genetic test results Will be months before results are available Discussion of types of results and what they mean Screening/management recommendations Genetic Testing Available at regional genetic centres and familial cancer clinics Covered by provincial insurance plans (i.e. OHIP) if criteria are met: Ontario US Privative Lab Full gene testing $1,400CDN $3,120 USD Ashkenazi Panel $350 $535 Familial mutation $250 $440 February 2009 Testing is only offered if the risk of mutation is ≥10% Test highest risk affected individual first Only in exceptional circumstances will testing be offered to unaffected individuals Results from Genetic Testing Positive Deleterious mutation identified Negative Interpretation differs if a mutation has previously been identified in the family Mutation known – true negative Mutation unknown – uninformative Variant of unknown significance Significance will depend on how variant tracks through family - i.e. is variant present in people with disease? Can use software to predict functional significance Check with lab to see if reported previously Risks/Benefits/Limitations of genetic testing Positive test result Potential Benefits: Clinical intervention may improve outcome Family members at risk can be identified Positive health behaviour can be reinforced Reduction of uncertainty Potential Risks: Adverse psychological reaction Family issues/distress Uncertainty -incomplete penetrance Insurance/job discrimination Confidentiality issues Intervention carries risk Risks/Benefits/Limitations of genetic testing? Negative test result Potential Benefits: Avoidance of unnecessary clinical interventions Emotional - relief Children can be reassured Avoidance of higher insurance premiums Potential Risks: Adverse psychological reaction (i.e. survivor guilt) Dysfunctional family dynamics Complacent attitude to health Risks/Benefits/Limitations of genetic testing? Uninformative test result Potential Benefits: Future research may clarify test results Positive health behaviour can be reinforced Some relief Higher insurance premiums may be avoided Potential Risks: Continue clinical interventions which may carry risks Complacent attitude to health Uncertainty Continued anxiety Higher insurance premiums may not be reduced Legend Breast cancer Case: Rachel’s test results…. Ovarian cancer Rachel BRCA1 185delAG Normal Mutation What is the benefit of having genetic testing? Can anything be done to change risk/outcome? Recommendations for BRCA1 and BRCA2 mutation carriers: Lifestyle Reduce dietary fat Avoid obesity Reduce alcohol consumption Regular exercise Weak Evidence Recommendations for BRCA1 and BRCA2 mutation carriers Breast cancer surveillance - Recommendations from Canadian Hereditary Cancer Task Force, JOGC 2007 BSE – not recommended CBE – part of surveillance program including imaging Mammography & MRI (if available) q12 months age ≥30 MRI (possibly + U/S) if surveillance required before age 30 MRI may have higher sensitivity for surveillance of breast cancer among BRCA1/2 carriers 2008 Meta-analysis: combined mammography and MRI screening had a 94% sensitivity, 77% specificity (95% CI; p=0.01) Recommendations for BRCA1 and BRCA2 mutation carriers Ovarian cancer surveillance - Recommendations from Canadian Hereditary Cancer Task Force, JOGC 2007 Surveillance not routinely recommended Women should be counselled on the limitations of current screening for ovarian cancer If woman chooses surveillance, then consider the following q6 months starting at age 30-35: pelvic exam transvaginal ultrasound serum CA-125 Symptom recognition Management of Mutation Carriers – Surgical options: Risk reduction mastectomy Recommendations from Canadian Hereditary Cancer Task Force, JOGC 2007 Potential benefits should be raised with all women with a known mutation. Multidisciplinary team that includes at least: genetics professional, breast surgeon, plastic surgeon. Women should have access to: Written and oral information Support services Adequate time for reflection Breast reconstruction options should be discussed in advance Management of Mutation Carriers – Surgical options: Risk reduction mastectomy Hartmann et al. NEJM 1999 Retrospective study of 639 women with FH of breast cancer who had bilateral mastectomy (mutation status unknown) Expected 37 br ca in 425 women at mod risk (Gail model) Observed 4 (90% risk reduction) 3 br ca in 214 high risk women with mastectomy (1.4%) 156 br ca in 403 sisters without mastectomy – 38.7% (90% risk reduction) Meijers-Heijboer et al. NEJM 2001 139 BRCA1 and BRCA2 mutation carriers No br ca after 3 years in 76 ♀ with risk-reducing mastectomy compared with 8 cases of br ca in 63 who chose surveillance Management of Mutation Carriers – Surgical options: risk reduction salpingooophorectomy (SO) Recommendations from Canadian Hereditary Cancer Task Force, JOGC 2007 The potential benefits of risk reduction SO should be discussed with women. Management by multidisciplinary team that includes a genetics professional 2009 meta-analysis Rebbeck et al. 80% reduction in risk of BRCA 1/2 -associated ovarian/fallopian tube cancer 50% reduction in risk of breast cancer in BRCA 1/2 mutation carriers Hazard ratio 0.21 (95% CI = 0.12-0.39) Hazard ratio 0.49 (95% CI = 0.37-0.65) Optimal age of SO – more study needed Management of Mutation Carriers Chemoprevention Tamoxifen Prevention Trial 2005 Raloxifene Shows promise No data for mutation carriers Aromatase inhibitors – ExCel trial Invasive breast ca reduced from 42.5/1000 in placebo group to 24.8/1000 in Tamoxifen group in women at increased risk of breast cancer Preliminary data suggest benefit for BRCA2 but not BRCA1 carriers Exemestane vs. placebo (Ca Info Service – 1-888-939-3333) No data for mutation carriers 2007 Canadian Hereditary Cancer Task Force Recommendations: women choosing chemoprevention should be enrolled in a clinical trial Management of Mutation Carriers Consider… Psychosocial support to assist with: Adjusting to new information most adjust within 3-6 months subset remain psychologically distressed (16-25% anxiety and/or depression) Making decisions regarding management “to inflict surgery is a hard decision to make… when I don’t have the disease and feel healthy” Addressing family issues, self concept, body image Dealing with future concerns i.e. child bearing, surgical menopause after oophorectomy Referral to support groups Management of Mutation Carriers Consider… Additional psychosocial support may be needed for high risk individuals such as those with: History Poor of depression/anxiety coping skills Inadequate Multiple Loss social support / conflict in the family losses in the family of parent at a young age Recent Multiple loss surgical procedures Testing children for BRCA1 and BRCA2 mutations Benefits and non-harm Autonomy Consider the child’s autonomy and ability to provide informed consent Parents are not always the decision maker for a child Privacy/confidentiality No medical benefit from genetic testing for children < 18 Potential harm from this information – psychological, insurability, etc. Results are available to the parent who may or may not share these with the child Equity & justice Access to resources if the genetic status is known vs unknown Despite focus on hereditary cancers… Most women will not develop breast cancer Of those who do, most will not have a known family history Increasing age is the greatest risk factor Most women with family history of breast ca: do not fall into a high-risk category do not develop breast cancer are not eligible for genetic testing All women should be “breast aware” and contact their health care providers if any lumps or breast changes are noted. Cases Assessing the Risk of Hereditary Breast Cancer Using the Canadian Cancer Society triage card (below), what category of risk do the following family histories fit into? Legend Case 1 Colon Breast Colon Ca Dx 76 died 85Aneurysm Alz -75 A&W A&W Your Patient ↑Chol A&W Accident BrCa Dx 68 Asthma A&W MI 80 BrCa Dx 61 Case 1 Legend Colon Breast Case 1 Answer: Moderate risk for hereditary breast cancer Two 1st/2nd degree relatives on the same side of the family with breast cancer < age 70 Management: CBE and mammogram q1 years starting at 40 Discuss lifestyle changes Consider enrollment in chemoprevention clinical trial Legend Case 2 Alz -75 Br Ca Dx 41 A&W Breast Accident Stroke -83 A&W Your Patient ↑Chol A&W IDDM Asthma A&W MI 85 Migraines Case 2 Legend Breast Case 2 Answer: Moderate risk for hereditary breast cancer One 1st/2nd degree relative with breast cancer at 35-49 years Management: CBE and mammogram q1 years staring at 40 Discuss lifestyle changes Consider enrollment in chemoprevention clinical trial Legend Case 3 Prostate Breast Ovarian Alz -75 A&W Bilateral Breast Ca Dx 49 died 53 Aneurysm OvCa Dx 52 Prost Ca 65 Your Patient A&W Accident IDDM Asthma A&W BrCa Dx 75 ↑ Chol Case 3 Legend Prostate Breast Ovarian Case 3 Answer: High risk for hereditary breast/ovarian cancer One 1st/2nd degree relative with: bilateral breast cancer, first one before age 50 ovarian cancer (any age) Case 3 Answer: High risk Management: Offer genetics or familial cancer clinic referral Pt. agrees: Familial Cancer Clinic will suggest management Pt. declines: Discuss management with familial cancer clinic or manage as moderate risk Referral to psychologist and/or support group Discuss: lifestyle changes, enrollment in chemoprevention clinical trials Legend Case 4 Colon Breast Colon Ca Dx 76 died 85Aneurysm Alz -75 A&W A&W Your Patient ↑Chol A&W Accident MI 69 ↑Chol A&W Breast Ca 85 BrCa Dx 71 Case 4 Legend Colon Breast Case 4 Answer: Low risk for hereditary breast cancer Meets none of the high or moderate risk criteria Management: Clinical breast exam & mammogram q 1-2 years beginning at age 50 Discuss lifestyle changes Legend Case 5 Prostate Breast Ovarian Nt Causes -75 A&W Eastern Europe Ashkenazi Jewish Irish / German Christian Prost Ca Dx 80 Died 81 Died 81 stroke Schizophrenic Your Patient OvCa Dx 52 MI 65 A&W IDDM Asthma IDDM BrCa Dx 55 ↑ Chol BrCa Dx 45 Case 5 Legend Prostate Breast Ovarian Case 5 Answer: High risk for hereditary breast/ovarian cancer 3 relatives on the same side of the family with breast or ovarian cancer at any age Management: Offer genetics or familial cancer clinic referral Agrees: Familial Cancer Clinic will suggest management Declines: Discuss management with familial cancer clinic or manage as moderate risk Referral to psychologist and/or support group Discuss: lifestyle changes, enrollment in chemoprevention clinical trials Legend Case 6 Bladder Breast Head & Neck Neck CA Dx 70 Bladder CA Dx55 Bladder CA Dx 58 died 62 A&W Your Patient Head CA Dx 65 A&W Accident Diabetes Asthma A&W MI-84 BrCa Dx 61 Case 6 Legend Bladder Breast Head & Neck Case 6 Answer: Low risk for hereditary breast cancer Meets none of the high or moderate criteria Patient’s family worked in a tannery and shoe factory. Aromatic amines (dyes) increase the risk of bladder cancers Shoe manufacturers have an increase risk of nasal cavity cancers The high incidence of cancer is due to common environment exposures. Resources The National Cancer Institute: http://cancernet.nci.nih.gov/ Detailed information on cancer for patients and physicians including causes, treatments, clinical trials & more Canadian Cancer Society: www.cancer.ca FORCE: www.facingourrisk.org www.hereditarybreastcancer.cancer.ca Patient information aid Gene Clinics: www.Genetests.org See Gene Reviews for clinical summaries Where to find a genetics centre: www.cagc-accg.ca/centre1.html The Genetics Education Project Committee June Carroll MD CCFP Judith Allanson MD FRCP FRCP(C) FCCMG FABMG Sean Blaine MD CCFP Mary Jane Esplen PhD RN Sandra Farrell MD FRCPC FCCMG Judy Fiddes Gail Graham MD FRCPC FCCMG Jennifer MacKenzie MD FRCPC FAAP FCCMG Wendy Meschino MD FRCPC FCCMG Joanne Miyazaki Andrea Rideout MS CGC CCGC Cheryl Shuman MS CGC Anne Summers MD FCCMG FRCPC Sherry Taylor PhD FCCMG Brenda Wilson BSc MB ChB MSc MRCP(UK) FFPH References 1. Offit K 1998 Clinical Cancer Genetics: Risk Counseling and Management. Wiley-Liss, New York. 2. Daly MB, Bars Culver JO, Hull JL, Levy-Lahad E. Overview of Breast Cancer Genetics at www.genetests.org Last update September 11, 2003.Accessed on March 15, 2005. 3. Statistics from the Canadian Cancer Society: http://www.cancer.ca/ccs/internet/standard/0,3182,3172_ 14435_371399_langId-en,00.html. Accessed on March 15, 2005. 4. Lightning bolt photo credit: http://www.ghouli.com/articles/sp/mainstream_4b.htm References 5. Seo, JH, Cho D-Y, Ahn S-H, Yoon K-S, Kang C-S, Cho HM, Lee HS, Choe JJ, Choi CW, Kim BS, Shin SW, Kim YH, Son G-S, Lee J-B, Koo BH. BRCA1 and BRCA2 germline mutations in Korean patients with sporadic breast cancer. Hum Mutat 2004; Online Mutation in Brief #746. 6. Ford D, Easton DF, Peto J. Estimates of the gene frequency of BRCA1 and its contribution to breast and ovarian cancer. Am J Hum Genet 1995; 57:1457-1462. 7. Struewing JP, Hartge P, Wacholder S, Baker SM, Berlin M, McAdams M, Timmerman MM, Brody LC, Tucker MA. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med 1997; 336:1401-1408. References 8. Calderon-Margalt R, Paltiel O. Prevention of breast cancer in women who carry BRCA1 or BRCA2 mutations: a critical review of the literature. Int J Cancer 2004; 112:357-364. 9. Tonin PN, Perret C, Lambert JA, Paradia A-J, Kantemiroff T, Benoit M-H, Martin G, Foulkes W, Ghadirian P. Founder BRCA1 and BRCA2 mutations in early-onset French Canadian breast cancer cases unselected for family history. Int J Cancer (Pred Oncol) 2001; 95: 189-193. 10. Easton DF, Ford D, Bishop DT. And the Breast Cancer Linkage Consortium. Breast and ovarian cancer incidence in BRCA1 – mutation carriers. Am J Hum Genet 1995; 56: 265-271. References 11. Satagopan JM, Offit K, Foulkes W, Robson ME, Wacholder S, Eng CM, Karp SE, Begg CB. The lifetime risks of breast cancer in Ashkenazi Jewish carriers of BRCA1 and BRCA2 mutations. Cancer Epidemiol Biomarkers Prev 2001; 10:467-473. 12. Antoniou A, Pharoah PDP, Narod S, Risch HA, Eyfjord JE, Hopper JL, Loman N, Olsson H, Johannsson O, Borg A, Pasini B, Radice P, Manoukian S, Eccles DM, Tang N, Olah E, Anton-Culver H, Warner E, Lubinski J, Gronwald J, Gorski B, Tulinius H, Thorlacius S, Eerola H, Nevanlinna H, Syrjakoski K, Kallioniemi O-P, Thompson D, Evans C, Peto J, Lalloo F, Evans C, Easton DF. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 2003; 72:1117-1130. References 13. Ford D, Easton DF, Stratton M, Narod S, Goldgar D, Devilee P, Bishop DT, Weber B, Lenoir G, Chang-Claude J, Sobol H, Teare MD, Struewing J, Arason A, Scherneck S, Peto J, Rebbeck TR, Tonin P, Neuhausen S, Barkardottir R, Eyfjord J, Lynch H, Ponder BA, Gayther SA, Birch JM, Lindblom A, Stoppa-Lyonnet D, Bignon Y, Borg A, Hamann U, Haites N, Scott RJ, Maugard CM, Vassen H and the Breast Cancer Linage Consortium. Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. Am J Hum Genet 1998; 62:676689. 14. Risch HA, McLaughlin JR, Cole DEC, Rosen B, Bradley L, Kwan E, Jack E, Vesprini DJ, Kuperstein G, Abrahamson JLA, Fan I, Wong B, Narod SA. Prevalence and penetrance of germline BRCA1 and BRCA2 mutations in a population series of 649 women with ovarian cancer. Am J Hum Genet 2001; 68:700-710. References 15. Liede A, Karlan BY, Narod SA. Cancer risks for male carriers of germline mutations in BRCA1 or BRCA2: a review of the literature. J Clin Oncol 2004; 22:735-742. 16. Kirchhoff T, Kauff ND, Mitra N, Nafa K, Huang H, Palmer C, Gulati T, Wadsworth E, Donat S, Robson ME, Ellis NA, Offit K. BRCA mutations and risk of prostate cancer in Ashkenazi Jews. Clin Cancer Res 2004; 10:2918-2921. 17. Thompson D, Easton DF and the Breast Cancer Linkage Consortium. Cancer incidence in BRCA1 mutation carriers. J Natl Cancer Inst. 2002; 94:13581365. References 18. Petrucelli N, Daly MB, Burke W, Bars Culver JO, Hull JL, LevyLahad E, Feldman GL. BRCA1 and BRCA2 Hereditary Breast/Ovarian Cancer www.genetstests.org Last updated September 3, 2004. Accessed March 15, 2005. 19. Bermejo JL, Hemminki K. Risk of cancer at sites other than the breast in Swedish families eligible for BRCA1 or BRCA2 mutation testing. Ann Oncol 2004; 15:1834-1841. 20. The Breast Cancer Linkage Consortium. Cancer risks in BRCA2 mutation carriers. J Natl Cancer Inst 1999; 91:1310-1316. 21. Predictive Cancer Genetics Steering Committee. Ontario physicians’ guide to referral of patients with family history of cancer to a familial cancer genetics clinic or genetics clinic. Ontario Medical Review 2001; 68:24-29. References 22. Pal Y, Permuth-Wey J, Betts JA, Krischer JP, Fiorica J, Arango H, LaPolla J, Hoffman M, Martino M, Wakeley K, Wilbanks G, Nicosia S, Cantor A, Sutphen R. BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases. Cancer 2005; 104:2807-2816. 23. Berg AO, Allan JD, Frame PS, Gordis L, Gregory KD, Harris R, Johnson MS, Klein JD, Loveland-Cherry C, Moyer VA, Ockene JK, Petitti DB, Siu AL, Teutsch SM, Yawn BP. U.S. Preventive Services Task Force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: recommendation statement. Ann Intern Med. 2005; 143;355-361. 24. National Cancer Institute: Breast Cancer Prevention: http://www.nci.nih.gov/cancertopics/pdq/prevention/breast/healthp rofessional Accessed on April 4,2005. References 25. Horsman D, Wilson BJ, Avard D, Meschino WS, Sing CK, Plante M, Eisen A, Howley HE, Simard J on behalf of the National Hereditary Cancer Task Force. Clinical Management Recommendations for Surveillance and Risk-Reduction Strategies for Hereditary Breast and Ovarian Cancer Among Individuals Carrying a Deleterious BRCA1 or BRCA2 Mutation. J Obstet Gynaecol Can 2007;29:45–60. 26. Warner E. Systematic Review: Using Magnetic Resonance Imaging to Screen Women at High Risk for Breast Cancer Ann. Intern. Med 2008;148:671. 27. Hartmann LC, Schaid DJ, Woods JE, Crotty TP, Myers JL, Arnold PG, Petty PM, Sellers TA, Johnson JL, McDonnell SK, Frost MH, Jenkins RB. Efficacy of bilateral; prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med 1999; 340:77-82. References 28. Meijers-Heijboer H, van Geel B, van Putten WLJ, HenzenLogmans SC, Seynaeve C, Menke-Pluymers MBE, Bartels CCM, Verhoog LC, van den Ouweland AMW, Niermeijer MF, Brekelmans CTM, Klijn JGM. Breast cancer after prophylactic mestomy in women with BRCA1 or BRCA2 mutations. N Engl J Med 2001; 345:159-164. 29. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin: Hereditary breast and ovarian cancer syndrome. Gynecol. Oncol. 2009;113:6-11. 30. Rebbeck TR, Kauff ND, Domchek SM. Meta-analysis of Risk Reduction Estimates Associated With Risk-Reducing Salpingooophorectomy in BRCA1 or BRCA2 Mutation Carriers JNCI 2009;101:80. References 31. Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, Bevers TB, Kavanah MT, Atkins JN, Margolese RG, Runowicz CD James JM, Ford LG, Wolmark N. Tamoxifen for the prevention of breast cancer: current status of the national surgical adjuvant breast and bowel project P-1 study. J Natl Cancer Inst. 2005; 97:1652-1662. Kote-Jarai Z, Powles, Mitchell G, Tidy A, Ashley S, Easton D, Assersohn L, Sodha N, Salter J, Gusterson B, Dowsett M, Eeles R. BRCA1/BRCA2 mutation status and analysis of cancer family history in participants of the Royal Marsden Hospital tamoxifen chemoprevention trial. Cancer Lett. 2007;247:259-265. 32. Prichard RS, Hill AD, Dijkstra B, McDermott W, O’Higgins NJ. The prevention of breast cancer. Br J Surg 2003; 90: 772-783 33. King M-C, Wieand S, Hale K, et al. Tamoxifen and breast cancer incidence among women with inherited mutations in BRCA1 and BRCA2: National surgical adjuvant breast and bowel project (NASBP-1) breast cancer prevention trial. JAMA 2001;286:2372256. References 34. Kote-Jarai Z, Powles, Mitchell G, Tidy A, Ashley S, Easton D, Assersohn L, Sodha N, Salter J, Gusterson B, Dowsett M, Eeles R. BRCA1/BRCA2 mutation status and analysis of cancer family history in participants of the Royal Marsden Hospital tamoxifen chemoprevention trial. Cancer Lett. 2007;247:259-265. 35. Narod SA, Brunet J-S, Ghadirian P, Robson M, Heimdal K, Neuhausen SL, Stoppa-Lyonnet D, Lerman C, Pasini B, de los Rios P, Weber B, Lynch H for the Hereditary Breast Cancer Clinical Study Group. Tamoxifen and risk of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers: a case control study. Lancet 2000; 356:1876-1881.