Body Fluids
advertisement

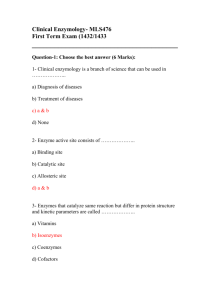
Body Fluids Deborah Goldstein Argy Resident September, 2005 Fluids • CSF • Pleural Fluid • Peritoneal Fluid Pt with fever, nuchal rigidity.... 1. Get blood cx 2. Give Abx • S. pneumo (30-50%), N. Meningitidis (10-35%), H. influenza (<5%), Listeria (5-10%), Staph • • • • Ceftriaxone 2mg IV q12h for GPC, GNR Vanc 1g IV BID for PCN-resistant Strep pneumo Ampicillin for Listeria (in elderly, young) Decadron 0.4mg/kg IV q12 if concern for Bact infxn • • Give with first dose of Abx! Improves mortality, reduces incidence of hearing loss 3. R/O increased ICP w/Head CT if needed 4. Do LP Who to LP? Indications • Fever, vomiting, HA, photophobia, altered level of consciousness, leukocytosis, meningeal signs...to r/o infection, malignancy Contraindications • INR>1.5 • Platelets <50,000 Risks of LP First Do No Harm... • Post-lumbar puncture HA – Have pt lie down 1-3hrs after to prevent CSF leak • Bleeding; spinal hematoma • Infection (poor sterile technique) • Herniation Lumbar Puncture Procedure • Pt lies in L lateral decub position, knees to chest • Posterior iliac crest as marker for L3-L4 space • Prep/drape lower back in sterile fashion...lidocaine • Insert LP needle pointing towards umbilicus until “pop” • Obtain opening pressure (only if pt lying down) • Fill tubes #1-4 with CSF CSF Evaluation • Tube 1-cell count and differential • Tube 2-glucose, protein • Tube 3-cultures, gram stain, cytology, (HSV PCR, West Nile, India ink, Crypto Antigen, VDRL, Lyme Ab, AFB...) • Tube 4-cell count and differential Normal CSF Composition • • • • • Clear color <5 RBC’s <5 WBC’s Protein 23-38mg/dl (can use 14-45) Glucose—60% of serum level (75-100) Opening pressure • • • • Normal = 80-180 mmHg Obese pts: up to 250mmHg can be normal Pathologically elevated: >250mmHg If elevated, likely due to cerebral edema from intracranial pathology • Infection (cryptococcal meningitis), tumor, benign ICH (pseudotumor) RBCs Always send tube #1 and #4 for cell count and compare RBCs Traumatic tap: Elev RBC in tube 1, nl in tube 4 – 1000 RBC : 1 WBC to adjust WBC count in bloody tap SAH or HSV: Elev RBC in tube 1 AND tube 4 • “Crenated RBCs” and xanthochromia (yellow supernatant after centrifuge) – Seen in hyperbilirubinemia (ESLD), old SAH, old blood from prior traumatic LP or bleed WBC’s • Infection! • PMN predominance: likely bacterial meningitis • Lymphocytic predominance: viral vs. fungal vs. TB vs. malignancy Protein • Normal: protein is excluded from CSF by blood-CSF barrier • Increased: nonspecific • Elevated in all infectious meningitis – May remain elevated for months postmeningitis (viral or bacterial) • Increased in malignancy and inflammatory conditions (ie Guillain-Barre) Glucose Normal • Viral infection Low glucose • Bacterial meningitis, TB, fungal Really low • <18 is strongly suggestive of bacterial meningitis Typical Viral Meningitis • CSF WBC elevated, but <250 (first PMNs, then lymphocytes) • CSF protein elevated, but <150 • Glucose > 50% of serum concentration Typical Bacterial Meningitis • CSF WBC >1000, PMN predominance • CSF protein >500mg/dl • CSF glucose <45 mg/dl Example • A previously healthy 33-year-old lawyer presents to the ER with acute onset headache and confusion. He develops grand mal seizures in the ER. He is treated and sent for a head CT, which shows bilateral hemorrhage in the temporal lobes (and no hydrocephalus). • CSF: mild pleocytosis (mostly lymphocytes), gluc= 60, protein = 30 a)Arbovirus encephalitis b)Brain toxoplasmosis c)Echovirus encephalitis d)Herpetic encephalitis e)Metastatic melanoma HSV Encephalitis • Aseptic meningitis: CSF w/mild lymphs, nl gluc, nl prot • Most common etiologic agent of sporadic viral encephalitis • Previously healthy pt with rapid onset of confusion and seizures • CT: hemorrhagic necrosis of the temporal lobes • Arbovirus encephalitis: most important cause of epidemic viral encephalitis; clinical course is milder and prognosis is better than herpetic encephalitis • CNS Toxo: in immunocompromised pts; round, ring-enhancing intracerebral masses • Echovirus encephalitis: common cause of asceptic meningitis; mild symptoms (headache, malaise) with normal CSF • Metastatic melanoma: CNS lesions may hemorrhage; but mets appear as space-occupying masses Example • Pt with AIDS on Combivir (AZT/3TC) and Indinivir c/o leg weakness, incontinence. On exam, reduced strength in lower extremities with mild spasticity. Also diminished sensation in b/l feet, legs. Brain MRI: nonfocal • CSF: Opening pressure=100 mm H20, Cell count=5 lymphs, Glucose=48, Protein=33 Normal serum B12, negative serum RPR, hct nl. • What’s he got? A. AIDS dementia complex B. CMV polyradiculopathy C. Cryptococcal meningoencephalitis D. Vacuolar (HIV) myelopathy E. AZT neurotoxicity HIV Myelopathy • Common neurologic complications of AIDS • Degeneration of spinal tracts in posterior, lateral columns (causing them to look vacuolated) • Physical findings are similar to B12 deficiency • Diagnosis of exclusion! • AIDS dementia complex: progressive memory loss, alterations in fine motor control, urinary incontinence, altered mental status • CMV polyradiculopathy: CSF has neutrophilic pleocytosis • Crypto meningoencephalitis: presents with signs/symptoms of meningitis, and CSF shows fungus • Zidovudine-related toxicity: can cause asthenia, myopathy Thoracentesis Indications • Diagnostic - All NEW effusions (except if clearly due to heart failure) • Therapeutic – Respiratory distress • Suspected parapneumonic effusions must be tapped ASAP (“Don’t let the sun set on a pleural effusion”) Don’t do Thoracentesis if... • Coagulopathy (INR>2, platelets <25,000) • Severe lung disease on contralateral side (risk of PTX) • Mechanical ventilation (not due to risk of PTX from PEEP, but due to decreased resealing) Loculated? • Must be >1 cm and free flowing in lateral decubitus view • If CT shows free-flowing fluid, you don’t also need lateral X-ray Thoracentesis Procedure • Confirm fluid is free-flowing, not loculated • Obtain consent • Consider US mark if medium-size effusion or loculated • Have pt sitting up and leaning forward over table • Percuss fluid level and go 1-2 spaces below, in midclavicular line • Enter just ABOVE the rib to avoid neurovascular bundle • ALWAYS obtain a CXR post-tap Pt gets dyspneic after you’ve withdrawn 150cc from L chest.... You took 2.3L clear fluid off this pt’s Right chest. F/u CXR shows.... Other Thoracentesis Complications • PTX • Re-expansion pulmonary edema – Don’t take off more than 1L • • • • Hemothorax Infection Hypotension Hepatic or Splenic puncture What to order? Serum LDH, total protein (Add on to am labs) Pleural fluid: • Total Protein, LDH • Glucose, cell count and diff, pH (on ice) • Gram stain, culture, fungal stain and culture, AFB • Cytology • Other: triglyceride level to r/o chylothorax; amylase to r/o pancreatitis, esoph perf; Adenosine deaminase to eval TB Light’s Criteria for Exudates Fluid is exudate if it meets 1 of 3 criteria: 1. Pleural fluid LDH/serum LDH > 0.6 2. Pleural fluid protein/serum protein > 0.5 3. Pleural fluid LDH > upper limit of normal serum LDH • If all 3 negative, fluid is Transudate Transudate • Result from imbalances in oncotic and hydrostatic pressure • Usually low oncotic +/- high hydrostatic pressure • Pulm Edema/CHF • Cirrhosis with ascites • Hypoalbuminemia/Nephrotic syndrome, ESLD • Fluid overload s/p aggressive IVF • Peritoneal dialysis Exudate Caused by local, not systemic, factors • Infection • Neoplasm • Pancreatitis • Esoph perf • RA • SLE • Sarcoid, Wegeners, PE, Meig’s, Chylothorax Lymphocytosis • Malignancy (50-70% lymphs) • Also TB, sarcoid, RA, chylothorax (>90% lymphs) Pleural eosinophilia • • • • Pneumothorax Hemothorax Pulm infarct Parasitic disease • • • • Fungal infection Drugs Malignancy Asbestos Why is glucose low? (<60) • • • • • • RA TB Empyema SLE Malignancy Esophageal rupture Who needs a chest tube? • Frank pus OR • Positive gram stain OR • pH < 7.0 Non-TB Parapneumonic Effusions Class 1 = “Nonsignificant” • <10 mm thick on decub. Don’t tap, just observe Class 2 = “Typical parapneumonic” • >10 mm thick on decub, pH>7.2 , Glucose>40 mg/dL • GS neg, cx neg • Diagnostic tap, then Abx alone Class 3 = “Borderline complicated” • pH>7.0, <7.2 and/or LDH>1,000 and glucose>40 mg/dL • GS neg, cx neg • Abx and serial thoracenteses Grading Effusions Class 4 = “Simple complicated” • pH<7.0 and/or glucose<40 mg/dL and/or Gram stain/culture positive • Not loculated or frank pus • Chest tube and Abx Class 5 = “Complex complicated” • pH<7.0 and/or glucose<40 mg/dL and/or Gram stain/culture positive • Multiloculated • Chest tube and fibrinolytics (rarely require thoracoscopy or decortication) Grading Effusions Class 6 = “Simple empyema” • Frank pus • Single locule or free flowing • Chest tube +/- decortication Class 7 = “Complex empyema” • Frank pus present • Multiple locules • Chest tube and fibrinolytics • Often requires thoracoscopy or decortication Example • A 59-year old man with HIV and Hepatitis C develops progressive SOB and presents to the ER satting 90% RA. On CXR, he has a large Right-sided pleural effusion. • Serum LDH=200, serum protein = 5.6. • Pleural fluid: LDH 100, protein 2700, WBC 400, pH 7.35, glucose=85 • Exudate or Transudate? Retap? Abx? • Pleural fluid LDH/serum LDH=100/200= 0.5 – needs to be >0.6 to be exudate • Pleural fluid protein/serum protein=2700/5600= 0.4 – needs to be >0.5 to be exudate • • • • • • Pleural fluid LDH is < ULN serum LDH Transudate Cause is cirrhosis/ascites Presents w/Right sided pl effusion No Abx or need to retap Tx the underling problem (ascites) w/diuretics, aldactone; optimize treatment for Hep C, HIV Example • A 34 y.o. woman with cystic fibrosis presents to the ER with fever, cough and night sweats for 10 days. CXR shows LLL consolidation and surrounding free-flowing effusion. • The lab loses tubes for serum LDH, protein • Pleural fluid: cloudy, LDH=1360, pH=6.9, gluc=36, gram stain neg • Does she need a chest tube? Fibrinolytics? Exudate • because LDH>upper limits of normal serum LDH Class 4 = “Simple complicated” • pH<7.0 and/or glucose<40 mg/dL and/or Gram stain/culture positive • Not loculated or frank pus • Chest tube and Abx, no fibrinolytics Paracentesis Indications for paracentesis • A febrile pt with ascites is assumed to have SBP until proven otherwise • New onset ascites—etiology? • Increasing abdominal pain/discomfort • Respiratory compromise • Unexplained leukocytosis, acidemia, renal failure • AMS Risks of Paracentesis • • • • Bowel perforation Hemoperitoneum (0.01%) Hematoma (1%) Infection (0.01%) Contraindications • Coagulopathy is NOT a contraindication – But don’t do paracentesis if pt is in DIC • Must be careful if minimal fluid visualized on U/S • If peritoneal carcinomatosis, do not do this procedure yourself – Gut gets tethered to the anterior abdominal wall and can’t move away from your needle; you can perforate it. Paracentesis • Percuss pt’s abdomen for dullness/shifting dullness • Avoid obviously visible abdominal wall collaterals • Avoid inferior hypogastric artery (midway between ASIS and lateral border of pubis) • If therapeutic, can drain up to 4L safely for symptomatic relief (BP check pre and post safe) • Large-volume tap: give 1 bottle (12.5g) 25% SPA for each 2L ascitic fluid removed Inferior hypogastric artery After paracetesis, SBP drops to 90 and hct drops by 4 points... What to send fluid for • • • • Cell count with diff Albumin LDH Total protein • glucose • Gram stain/cx • cytology Appearance of fluid • Clear—usually indicates uncomplicated ascites, ie liver failure/cirrhosis • Turbid/cloudy—infected • Pink/bloody—traumatic, punctured collateral vessel, malignancy – Correct for bloody tap: 1 WBC: 750 RBC 1 PMN: 250 RBC Serum-to-ascites albumin gradient (SAAG) =Serum albumin – ascitic fluid albumin If the gradient is >1.1: • Portal HTN (drives fluids into peritoneum) • SBP, cirrhosis, Alcoholic hepatitis, CHF If the gradient is < 1.1: (protein leaks into peritoneum and fluid follows) • Peritoneal carcinomatosis, peritoneal TB, pancreatitis, nephrotic syndrome SBP • SAAG > 1.1 • Suspect if >250 PMNs (>100 PMNs in pt on peritoneal dialysis) • 70% GNR (E.coli, Klebsiella) 30% GPC (S. pneumo, Enterococcus) • Treat with ceftriaxone, cefotaxime • “Culture negative SBP” if >250 PMNs but cx neg; treat the same Bowel Perforation • • • • GPC in chains, GPR, GNR, fecal flora... Increased PMN’s, Total protein >1g/dl, Glucose <50mg/dl, LDH elevated Pt is SICK