IBs - Personal Health Budgets Evaluation

Evaluation of the Individual
Budget Pilot Projects
Karen Jones, Ann Netten, José-Luis Fernández,
Martin Knapp, David Challis, Caroline Glendinning,
Sally Jacobs, Jill Manthorpe, Nicola Moran, Martin
Stevens and Mark Wilberforce
Individual Budgets (IBs)
At heart of ‘personalisation’ agenda
Promoting choice
2005 Cabinet Office Strategy Unit report
2005 Social Care Green Paper
Built on experiences of:
Direct payments
In Control
Principles underlying IBs
Greater role for users in assessing needs
Users should know resources available before planning how needs met. Resource Allocation
System (RAS) recommended
Encourage users to identify desired outcomes and how to achieve these
Support individuals in using IBs
Test opportunities to integrate funding streams and simplify/integrate/align multiple assessment processes and eligibility criteria
Experiment with different ways of deploying IBs
Funding streams in IBs
Adult social care (gateway to IB)
Supporting People (DCLG)
Independent Living Fund (DWP)
Disabled Facilities Grant (DCLG)
Access to Work (DWP)
Integrated Community Equipment Services (DH)
Potential deployment options
Considerable local and individual flexibility:
Cash direct payment
Care managerheld ‘virtual budget’
Providerheld ‘individual service account’
Indirect payment to third party
… or combinations of these
The IB pilots 2006-7
13 local authorities
representative mix but higher than average take-up of direct payments
Mix of user groups (OP, LD, MH, P/SI)
Mix of funding streams
Evaluation
Do IBs offer better way of supporting disabled adults and older people than conventional methods of resource allocation and service delivery?
Which models work best and for whom?
Evaluation covered:
User experiences, implementation experiences, funding stream integration, impact on care managers, impact on providers, risk and protection, outcomes, costs, cost-effectiveness
IBSEN evaluation
Do individual budgets offer a better way to support disabled adults and older people than conventional methods of resource allocation and service delivery?
If so, which models work best and for whom?
Evaluation dimensions
User experience
Carer impact
Workforce
Care management
Provider impact
Risk & protection
Commissioning
Outcomes
Costs
Cost-effectiveness
Evaluation design
Randomised trial – 500 each IB and comparison groups across sites and user groups
Baseline data on circumstances and current support arrangements
Outcome interviews after 6 months
IB group – content and costs of support plans
In-depth user interviews 2 – 6 months – support planning process
Interviews with IB leads (x 2), providers, commissioning managers, other managers
Interviews and diaries, front-line staff and first-tier managers
Data collection
Randomised controlled trial – within each site, users allocated to IB or comparison group
Baseline data from LA records
Follow-up outcome interviews after 6 months
Analysis IB support plans
In-depth user interviews – support planning process
Interviews with IB leads, funding stream leads, providers, commissioning and other managers, support planning organisations
Interviews and diary study, front line staff and first tier managers
People included in the evaluation
1594 of the 2521 individuals randomised (63%) consented
Final sample of 959 people:
34% physically disabled
28% older people
25% with learning disabilities
14% using mental health services
Wide variations in age, functional need and FACS level
IB and comparison groups not different at baseline
Note : IB not in place at 6 months for everyone
Costs
Average weekly value of an IB:
£359 learning disabilities £228 older people
£310 mental health users £149 disabled people
Average weekly cost across all user groups =
£279 for IB group … £296 for comparison group
Care manager support for IB group (£19) was higher than for those with conventional support (£11)
Cost variations : higher costs for those who declined an IB ; and for those without a support plan at 6 months
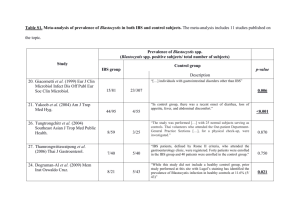
Funding streams
Funding stream integration
99% support plans contained social service funding
11% of support plans contained SP funding
8% of support plans contained ILF monies
1 support plan contained Access to Work funding
No support plans contained funding from DFG
Deployment options
67% IB managed as a DP
MH (89%) more likely
OP (56%) less likely
20% managed by local authority
13% managed by an agent
1 IB administered through a Trust
4 had services organised through a provider
Patterns of Expenditure
Personal assistant
Home care
Leisure activities
Planned short breaks**
Other
Direct payments
% Mean annual expenditure
64 £8,940
20
43
£7,140
£2,020
24
23
£1,750
£930
Managed budgets
% Mean annual expenditure
47 £7,420
40
24
£7,480
£1,750
15
21
£5,460
£270
Examples of Innovation
Accommodation
(N=24)
Cleaning service
Decorating service
Gardening service
Employment and occupation
(N=16)
Going out: trips/cinema etc
Health-related (N=3)
Private health care
Classes/arts and crafts
Gym membership/swimming
Computer maintenance
Admission fees for service user and PA
Massage for carer
Alternative therapy
IB Process
45% IB services in place at interview
10% for less than one month
51% for more than 3 months
11% not all in place
Do IBs impact on outcomes?
Do IBs improve outcomes?
Interviews at 6 months; only 45% had IB support in place
Measures:
Quality of life (7-point scale)
Psychological well-being (GHQ12)
Social care outcomes (ASCOT)
Satisfaction (7-point scale)
Differences between IB and comparison groups
Multi-variate analyses
Outcomes
Quality of life
Overall sample – no significant difference
MH – IB group better QoL
Psychological well-being (GHQ12)
Overall sample – no significant difference
OP – IB group lower well-being
Both measures – bigger IBs = better outcomes
Social care outcomes (ASCOT)
Overall sample – no significant difference
IB group higher scores in ‘control over daily living’ domain
LD – higher levels of control
Satisfaction
IB group more satisfied overall
P/SD IB group more satisfied
Overall outcomes
Positive effects of IBs
QoL, social care outcomes and satisfaction
Older people
Concerns about managing budgets?
Anxiety about change?
Lower budgets, more personal care, less flexibility?
Level of IB affects outcome
Are IBs cost-effective?
Are improvements in outcomes justifiable in terms of costs?
Combined data on costs and outcomes
Some evidence of cost-effectiveness in overall sample in respect of social care outcomes
Weaker evidence of cost-effectiveness with respect to psychological well-being
But significant variations by user group:
IBs more cost-effective for PD and MH groups
No evidence of cost-effectiveness for OP