Creating Policies To Support Trauma
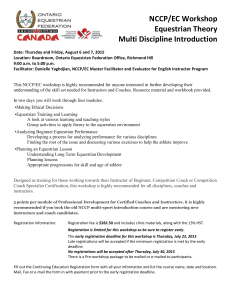
advertisement

Creating Policies to Support Trauma-informed Perspectives and Practices Janice L. Cooper, PhD Interim Director 3rd Annual Symposium, Bridging the Gap Fort Worth, Texas | November 3, 2009 Who We Are NCCP is the nation’s leading research and policy center dedicated to the economic security, health, and well-being of America’s low-income children and families. Part of Columbia University’s Mailman School of Public Health, NCCP promotes family-oriented solutions at the state and national levels. Our ultimate goal: Improved outcomes for the next generation. www.nccp.org Outline Background Trauma and Its Effects Special Populations Current Services and Policy Challenges Best Practices Specific Policy Interventions Policy Recommendations www.nccp.org Background 1982 Jane Knitzer’s seminal study, Unclaimed Children: The Failure of Public Responsibility to Children and Adolescents in Need of Mental Health Services 2005 work began for “Unclaimed Children Revisited: The Status of Children’s Mental Health in the United States 25 Years Later ” 2007 released Trauma Report 2008 released national report www.nccp.org Throughout her remarkable life and its many diverse experiences and achievements, Dr. Jane Knitzer embodied one consistent theme: that every child and every family is sacred, and that it is every person’s duty to reach out to the most marginalized and vulnerable among us. NCCP Director 2004-2009 Her life’s work reflects these values at every stage. Most recently on the IOM Committee on Depression, Parenting Practices, and the Healthy Development of Children www.nccp.org Unclaimed Children Revisited: Interests & Aims Identify effective state fiscal, infrastructure, training and related policies Research-informed Developmentally appropriate Family/youth driven Culturally competent Promote research informed dialogue to move policy Complement President’s New Freedom Commission’s initiatives by disseminating information on specific policy options www.nccp.org Understanding Trauma and its Effects Trauma is pervasive. Trauma refers to the severe distress, harm or suffering that results from overwhelming mental or emotional pain or physical injury. www.nccp.org Understanding Trauma and its Effects A core feature of the impact of the trauma is the long and short term loss experienced by those exposed to traumatic events. Critical elements of child development undermined by trauma (Cloitre, Cohen and Koenen, 2006): healthy attachment, social and emotional competency, self-assurance, confidence, independence www.nccp.org Lessons from ACES Study (Dube et al., 2001, Felitti et al., 1998) Strong relationship between adverse childhood experiences (5+) Suicide and Suicidal Attempts Chronic Illness (Obesity, Heart Disease, Liver Disease) Addictions Mental Health Problems Premature Death www.nccp.org What We Mean By Trauma-informed Trauma-informed strategies ultimately seek to (Harris & Fallot, 2001): do no further harm; create and sustain zones of safety for children, youth and families who may have experienced trauma; promote understanding, coping, resilience, strengths-based programming, growth, and healing www.nccp.org Children & Youth Disproportionately At-risk Children from Military Families Survivors of Abuse, Neglect & Sexual Violence Children & Youth with Disabilities Youth in Juvenile Justice Children who Experienced Natural and Man-Made Disasters Youth with Substance Use Disorders Homeless & Runaway Youth Children & Youth at Risk of Suicide Youth of Color www.nccp.org Children from Military Families Over 1.2 million children live in military families Approximately 700K have at least one parent deployed (Johnson et al., 2007) Deployment predictive of: 2X increase risk of child maltreatment (Gibbs et al., 2007) Increased risk of child trauma across developmental span from infancy through adolescence (Lincoln, Swift, Shorteno-Fraser, 2008) 32% child psychological morbidity; 42% high parental stress (5-12 yo) (Flake et al., 2009)* High parental stress put children at more than 7X increase risk for poor child psychological functioning* Among young children (U 5yo) those 3-5 higher levels of externalizing behaviors independent of parental distress (Chartrand,et al., 2008) www.nccp.org Children and Youth from Military Families Prevalence of Mental Health Problems among Military Personnel Post deployment 20% of active duty and 42% of reservists needed mental health treatment (not identify prior to deployment) (Lamberg, 2008)* Reservists, National Guard and younger active duty service members with combat related exposure increased risk for new onset of heavy drinking, binge drinking and alcohol-related problems (Jacobson et al., 2009) Lack of confidentiality may deter soldiers from accessing SUD related treatment (Milliken, Auchterlonie & Hoge 2007)* Referrals to SUD treatment dramatically lower compared to MH treatment* www.nccp.org Child/Youth Survivors of Abuse, Neglect & Sexual Violence Maine: 33% females and 67% males: a trauma related diagnosis or were involved in child welfare due to traumatic event (Yoe, Russell, Ryder, Perez and Boustead 2005) 50% female & 70 male rape survivors raped prior to age 18 (Tjaden, P and Thoennes 2006) 20% Females 50% Males Raped by age 12 www.nccp.org Children Who Experienced Abuse, Neglect or Sexual Violence www.nccp.org www.nccp.org www.nccp.org Disabled Children & Youth at Higher Risk More likely to be abused (Sullivan & Knutson, 1998) physically (1.5 times) sexually (2.2 times) Deaf children & youth higher risks (Sullivan & Knutson, 1998) www.nccp.org High Prevalence of Trauma Exposure in Juvenile Justice Over 90 % in juvenile detention in a large urban county have been exposed to at least one traumatic event & nearly 60% have experienced 6 or more traumatic events. (Abram et al, 2004) 11 % of youth in JJ were diagnosed with PTSD upon clinical assessment. (Abram et al, 2004) www.nccp.org What the Data Shows School-age Youth in Juvenile Detention Males Females Any MH disorder Any SUD disorder Anxiety disorder ADHD Any Disrupt. disorder Affect. disorder 65.5 73.8 50.7 46.8 21.3 30.8 16.6 21.4 41.4 45.6 18.7 27.7 Prevalence Behavioral Health Disorders of Youth in Detention by Gender (%) NB: Approx. 90% of youth in JJ are males. Source: Teplin, L., Abram, K., McClelland, G. M., Dulcan, M., & Washburn, J. J. (2006). Psychiatric Disorders of Youth in Detention. Juvenile Justice Bulletin (April 2006), 1-16. www.nccp.org What Data Shows: School-age Youth Who Experience Cumulative Trauma Overall cumulative exposure to childhood trauma = 82.5 Males were: 3.3 x more likely than females to experience intentional or “assaultive” violence (e.g. being raped, mugged, held up or threatened with weapon) 2.2 x more likely than females to experience other injury or trauma Source: Breslau, N., Wilcox, H. C., Storr, C. L., Lucia, V. C., & James, A. (2004). Trauma Exposure and PostTraumatic Stress Disorder: A Study of Youths in Urban America. Journal of Urban Health, 81(4), 531-544. www.nccp.org Children who experienced trauma from natural and man-made disasters Of Katrina survivors who were parents: (Abramson & Garfield, 2006) Nearly 50% reported their children had new emotional/behavioral problems Nearly 50% reported that they “never or only sometimes felt safe” Of all returning vets from Afghanistan & Iraq, those of transition-age (18-25), were the most likely to develop PTSD (Seal, Miner, Sen, & Marmar, 2007)* Overall PTSD rates among veterans of OEF/OIF 4X higher than community samples* www.nccp.org Youth with Substance Use Disorders at High Risk 3-4 times higher risk for PTSD (1) Multiple exposures to trauma predicted developing SUD (2) Youth with co-occurring PTSD & SUD lower levels of functioning (1) SUD associated with community violence, interpersonal violence, child maltreatment and self harm (3) SUD can serve as mechanism for self addressing trauma (3) SUD impedes effective trauma treatment (4) 1) Giaconia et al., 2000; 2) Giaconia et al., 1995; 3) Kilpatrick et al., 2003; 4) Jaycox, Ebener, Damesek, & Becker, 2004; Riggs, 2003. www.nccp.org Children of Homeless Families & Runaway Youth Two-fifths of the homeless population in the United States is made up of families (Bassuk et al, 2005). Their homelessness puts them at increased risk for other trauma, including physical and sexual violence, emotional abuse and intense anxiety and uncertainty. Almost two-thirds of homeless and runaway youth living on the street have witnessed violence and between 15-51 percent have been physically or sexually assaulted (Kipke et al, 1997). www.nccp.org www.nccp.org www.nccp.org Children at Risk of Suicide Three groups with a greater risk: American Indian/Alaska Native children and youth due to the historical trauma and current deprivation and trauma 64 % of all the completed suicide are committed by this group nationally, 17.6/100,000 versus 10.4/100,000 (Middlebrook et al, 2005) www.nccp.org Children at Risk of Suicide Adolescent Latinas A higher risk for suicide than Latino boys (15 % versus 7.8%) and non-Latino boys and girls (Keaton et al, 2006). Among girls, Latinas attempted suicide 50-60% more than African-American and white female adolescents (The NHSDA report, 2003). www.nccp.org Children at Risk of Suicide Gay, Lesbian, Bisexual, Transgendered and Questioning Youth (GLBTQ) Between 1.7 and 2 times more likely than their non-gay and lesbian peers to have suicidal thought (Russell & Joyner, 2001) More than 2.5 times more likely to attempt suicide than their non-gay peers (Russell & Joyner, 2001) www.nccp.org Secondary/Vicarious Trauma among Providers Impacts their ability as caregivers (Bober et al., 2005) Leads to higher rates of turnover (Van Hook, 2008) Provider with self care strategies included these in tx, led to lower levels secondary trauma & reduced turnover (Gordon, 2005) www.nccp.org Strategies to Reduce Vicarious Trauma (Osofsky, Putnam & Lederman, 2008) Smaller Caseloads Self-care Improve supervision of front-line workers Access to mh services Impart information on secondary trauma www.nccp.org Long-term Effects of Trauma Negative Impact on Brain Development Academic and Social Problems Chronic Illness, Morbidity and Mortality Intergenerational Impact www.nccp.org Current Service and Policy Challenges www.nccp.org Current Policy and Service Responses Characterized by: Failure to routinely screen and treat for trauma Lack of traction to use proven effective treatment strategies Use treatment practices and environments that retraumatize Seclusion & Restraint Boot Camp Peer or Staff Abuse Insufficient Attention to Vicarious/Secondary Trauma www.nccp.org Failure to Routinely Screen and Treat Information on child trauma rarely received according to some studies (Taylor et al., 2005; Hansen, Hasselbrock & Tworkowski, 2002) 84% of agencies reported in one study no/or extremely limited information on child/youth trauma history Much of emerging knowledge on trauma fails to make it into daily practice (Taylor et al., 2005) 33% of agencies report did not train staff to assess trauma Less than 50% reported training their staff on EBP for children and youth with exposure to trauma www.nccp.org State Policies and Practices that Re-traumatize www.nccp.org GAO (2007) report on Abuse in State-sponsored institutions: RTFs, boot-camps, wilderness camps 33 states with over 1600 staff involved in incidences of abuse of children and youth in 2005 10 investigated deaths within RTFs (one case in Texas) revealed common threads Untrained and inexperienced staff Lack of adequate nourishment in pursuit of “tough love” philosophy/strategies Reckless/negligent operating procedures www.nccp.org SAMHSA Policy on Seclusion and Restraint www.nccp.org Other Public Policies Can Serve to Expose Children/Youth to Trauma or Re-traumatize Immigration Reform Restrictive Housing Policies Disaster Response Plans Photo: P. Pereira, The Standard Times www.nccp.org Immigration Policies and Trauma 12 million undocumented workers in the US Estimates 5 million children have at least one parent undocumented 60% of these children are US-born citizens Over 1.6 million immigration related arrests Impact on children: Urban Institute/La Raza study 506 children; impact on attending school, accessing resources, getting different caring arrangements (Capps, et al. 2007) Children whose parents deported, arrested or detain in MN, CO, TX, NE,IA (NCCP analysis, 2006) www.nccp.org Source: http://www.ice.gov/pi/news/factsheets/worksite.htm www.nccp.org Unaddressed Challenges Funding Restrictions that Impeded Care and Sustainable Treatment Limited Support for Prevention & Early Intervention Workforce problems: Inadequacy in Supply and Quality www.nccp.org Identifying Best Practices: Key Elements Services Standardized Screening and Assessments Evidence-Based Interventions Culturally-Based Strategies Family and Youth Engagement and Support Infrastructure Training Policies to Eliminate/ Reduce Seclusion & Restraint Financial Strategies Culturally Competent Policies State Disaster-Related Plans for MH services www.nccp.org Best Practices: Selected Screening & Assessment Tools Acute Stress Checklist Child Dissociative Checklist Child Post-traumatic Stress Reaction Index Child PTSD Symptom Scale Child Stress Disorder Checklist Child’s Reaction to Trauma Event Scale Children’s Impact of Traumatic Event Scale Children’s PTSD Inventory Children’s PTSD Interview Children’s Sexual Behavior Inventory Clinician Administered PTSD Scale DISC (PTSD Module) Lifetime Incidence Traumatic Events Los Angeles Symptoms Checklist Trauma Symptom Checklist (Young Children/Children) When Bad Things Happen www.nccp.org Selected Evidence-based Interventions Parent Child Interaction Therapy aka Honoring Children, Making Relations (Bigfoot) Trauma-Focused CBT aka Honoring Children, Mending the Circle (Bigfoot) Cognitive Behavioral Interventions for Trauma in Schools Dialectical Behavior Therapy Trauma Recovery and Empowerment for Adolescents Seeking Safety for Adolescents www.nccp.org Case Studies (NY, ND, ME) www.nccp.org North County Children’s Clinic (NCCC): New York Watertown, NY 10th Mtn Division avg deployment OEF/OEF 5x Target Population- Families (Children) of Military Personnel 27,000 residents (16,000 active duty military – 60% deployed) 4 school-based health centers provide over 2000 mental health visits per year to children and families www.nccp.org North Country Children’s Clinic, New York Strengths Positive School Relations Clinically sound programming Collaboration with the Military HMO Challenges Military reimbursement for psy. health care inadequate Sustainable program funding Magnitude of needs exceed capacity Gaps in the continuum of care TriCare two-tier system; disallows some PCTs for e.g. family conflict and child maltx; no coverage intensive commty tx www.nccp.org Quote from Family Member We receive our medical care at the -- Ambulatory Health Clinic. We took our son there in June and expressed our concerns for his mental health. The Doctor wrote a referral for a child psychologist in our town. That doctor had a 3 month waiting list to get on the waiting list for an appointment. By now school had started and we were having nights where he stayed up all night crying, wanting his father to come home. If I did get him to sleep, he woke up crying. It became a struggle even to get him to go to school, he saw no use in going to school if that meant growing up without his father. He had also started losing interest in church, and cub scouts, two things that he usually loves. He did not want to leave the house at all…… With the help of the school-based clinic I was able to start helping my son cope with the deployment…… www.nccp.org Medicine Moon Initiative-North Dakota State-Tribal Initiative with 6 tribes Built upon System of Care Sacred Child Project Strong training component draws on cultural strengths and lessons learned from historical trauma “Ours is a way of teaching parents that children are sacred” Courtesy: Deb Painte, MMI www.nccp.org Medicine Moon Initiative-ND Strengths Culturally competent Wraparound Agreement with the state to bill directly for Medicaid Challenges Lack of sufficient psychiatric or behavioral resources to meet the most acute needs Lack of funding Focus on both current and historical trauma www.nccp.org Thrive: Trauma-informed System of Care, Maine Care delivery through trauma-lens Age 0-12 Service philosophy: “What has happened to this family” not, “What is wrong with this family” www.nccp.org Thrive: Trauma-informed System of Care, Maine Strengths System of care focused on strength, engaging whole family Universal screening Promotion of effective trauma specific treatments Staff Training Use of trauma sensitive assessments Quality assurance Challenges On-going provider buy-in, territorial issues pose obstacles to collaboration Medicaid managed care curve-out Struggles with substantive inclusion of all relevant agencies Sustainable financial and programmatic efficacy www.nccp.org Literature Review & Analysis of publicly available data: Main Data Sources Jennings, Ann. (2004). Blueprint for Action. Building Trauma-Informed Mental Health Service Systems: State Accomplishments, Activities and Resources. September 2004. http://www.annafoundation.org/articles.html State block grant applications. 2004-2007 SAMHSA Grant Awards - State Summaries FY 2005/2006 Personal Interviews with selected state officials www.nccp.org Services: Standardized Screening and Assessments Most states offer some form of screening and assessment. In nearly 60 percent of states and territories (data available on 46 states) universal or selective screenings and assessments are being conducted. In many cases the scope is limited. www.nccp.org Services: Evidence-Based Interventions In less than 20 percent of states which provide screenings and assessments, the screening and assessment tools are evidence-based. More than 50 percent of states provide evidencebased treatment/services; however, the scope is mostly limited. www.nccp.org Services: Culturally-Based Strategies About 30 % of states have culturally competent, trauma informed or focused treatment/services. www.nccp.org Infrastructure: Training Many states have developed training strategies of varying depth to increase the clinical and support capacity of those who deliver services to children, youth and their families who have been exposed to trauma. Nearly 40 percent of states (data available for 38 states) report training on trauma-informed/specific evidence-based practices. A small proportion of this training focuses on cultural groups, gender or families. www.nccp.org Infrastructure: Training (cont’d) While not widespread some best practices in training in states include: Strategies those aimed at developing trauma specialists as in Oklahoma System-wide or discipline-wide training like in Connecticut, Maine, Nevada, New York, Oklahoma, Illinois and Washington Trauma-related training that meet the conditions for state clinician certification as in Wyoming Embedding a trauma focus in statewide evidence-based training dissemination center in New York www.nccp.org Infrastructure: Policies to Eliminate/Reduce Seclusion & Restraint At least twenty states have implemented laws, regulations or policies designed to reduce and ultimately eliminate the use of seclusion and restraint. Five of these states have implemented strategies with far-reaching impact. www.nccp.org Infrastructure: Financial Strategies A number of state legislatures have also appropriated funding for specific trauma-related initiatives. Other state leaders have expanded the Medicaid benefit set to reimburse evidence-based trauma treatments, to facilitate trauma-specific treatments through billing and to fund specific clinicians. Generally absent are any state specific strategies to use the focus on information technology to create a more trauma-informed system. www.nccp.org Infrastructure: Culturally Competent Policies 8 states reported have culturally competent, trauma-focused policies. Alaska Connecticut Illinois New York Oklahoma South Carolina Vermont Washington www.nccp.org Highlights of State Responses: Illinois & Oklahoma Illinois Legislation requiring trauma informed services State plan for child welfare includes public health framework Workforce development Use of Effective Treatment Strategies Oklahoma Trauma strategies heavily workforce development centered Promotes cross systems collaboration Full-time state level trauma coordinator Evaluates and provides TA to contractors based on Jennings checklist of administrative practices and services www.nccp.org Key Elements of Success Leadership Support Funding State • Child Trauma Counseling Lessons Learned Standards for Trauma Informed Care Standards/Core Competencies for Trauma Informed Care Communication is essential Develop a common language for trauma. Transformation takes time. Federal • Co-occurring Initiative • Cross Training Initiative • Transformation Initiative • National Child Traumatic Stress Initiative Full time coordinator Collaboration Courtesy: Julie Young, OK www.nccp.org What did NCCP Survey Questions on Trauma Add? www.nccp.org Systematic Screening or Intervention for Trauma or Suicide Risk (Children and/or their Parents) 40 states report systematic screening or treatment for trauma or suicide risk 13 states did not respond or systematic screen/treat Common state efforts 12 reported screening for trauma/suicide risk (4 reported using Columbia Teen Screen) 10 states reported providing training on validated tools such as on TF-CBT; Applied Suicide Intervention Skills Training (ASIST); Question, Persuade & Refer (QPR); and, crisis/suicide prevention and intervention 7 states report using funds like Garrett Smith funds for prevention www.nccp.org Plan to Deliver Mental Health Services and Supports in Times of Disaster or Emergency 34 states reported that they had a specific plan 17 states reported that they did not have a plan 2 states did not respond Designated Individual in CMH charged with service coordination in the case of disaster/emergency 24 states reported they had a designated individual 8 states reported that they did not (in case of 3 for MH not specifically child mh) 17 missing/NA www.nccp.org Types of Responses from States on MH Services for Children in State Emergency Plan Each regional coordinator has a designated emergency satellite phone Regional (10) disaster management teams A system of trained and coordinated crisis counseling staff and networks A network ready to respond of volunteers and professionals “All hazards” leadership team A MOU with community behavioral health centers to coordinate, organize and mobilize during any crisis www.nccp.org Policy Recommendations www.nccp.org All federal, tribal, state and local policies should reflect a trauma-informed perspective Important factors: Developmentally appropriate Culturally & Linguistically Competent Encompass public health framework Engage children, youth and their families in healing. Fiscally-responsive Collaborative Accountable Support infrastructural development Competency-based training Address vicarious trauma www.nccp.org Policies should support/reinforce: Delivery systems that identify and implement strategies to prevent trauma, increase capacity for early intervention and intervention and provide comprehensive treatment Strategies designed to prevent and eliminate practices that cause trauma or re-traumatize Core components of best practices in traumainformed care: prevention, developmentally appropriate, empirically supported strategies, cultural and linguistic competence and family and youth engagement www.nccp.org Trauma-informed related policies must include/ensure: Funding that is supportive of care and that adequately reimburses for effective strategies Funding is contingent upon elimination harmful practices that re-traumatize Investment in strategies to ensure workforce competency in effective strategies Provision of incentives for care delivered in community-based settings like schools and child care settings in addition to health care settings www.nccp.org For More Information, Contact: Dr. Janice Cooper cooper@nccp.org Or Visit NCCP web site www.nccp.org SIGN UP FOR OUR UPDATES www.nccp.org