chapter 10 - WordPress.com
advertisement

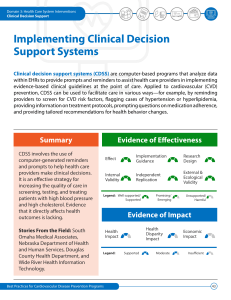
INCORPORATING EVIDENCE USE OF COMPUTER –BASED CLINICAL DECISION SUPPORT SYSTEMS FOR HEALTH PROFESSIONALS Ida Androwich Margaret Kraft 1. Define computerized clinical decision support systems (CDSS). 2. Identify types of CDSS, their characteristics, and the levels of responsibility implicit in the use of each type. 3. Describe effects of CDSS on clinician performance and patient outcomes in healthcare. 4. Understand the features, benefits, and limits of CDSS. 5. Develop a future vision for CDSS within nursing. Clinical decision support Decision support systems Information systems Knowledge and Cognition • Decision support systems (DSS) are automated tools designed to support decision-making activities and improve the decisionmaking process and decision outcomes. • A CDSS is designed to support healthcare providers in making decisions about the delivery and management of patient care. • A CDSS program’s goals may include patients safety and improved outcomes for specific patient populations as well as compliance with clinical guidelines, standards of practice , and regulatory requirements. • The primary goal of CDSS is the optimization of both the efficiency and effectiveness with which clinical decisions are made and care is delivered. • Nursing decision support systems (NDSS) are tools that help nurses improve their effectiveness, identify appropriate interventions, determine areas in need of policy or protocol development, and support patient safety initiatives and quality improvement activities. • CDSS includes a set of knowledge-based tools that can be fully integrated with the clinical data embedded in the computerized patient record (Electronic Health Record) to assist providers by presenting information relevant to the healthcare problems being faced. • CDSS may focus on treatment, diagnosis or specific patient information. • CDSS may be defined as any computer program that helps health professionals make clinical decisions. CDSS software has a knowledge base designed for the clinician involved in patient care to aid in clinical decisionsmaking. • Johnston et al. (1994) defined CDSS as “computer software employing a knowledge base designed for use by a clinician involved in patient care, as a direct aid to clinical decision-making.” • Sims et al. (2001) broadened the definition to “CDSS are software designed to be a direct aid to clinical decision –making, in which the characteristics of an individual patient are matched to a computerized clinical knowledge base and patient-specific assessments or recommendations are then to the clinician or the patients decision.” • Coiera (1994) discussed the role of CDSS as augmenting human performance and providing assistance for healthcare providers especially for tasks subject to human error. • Whatever definition chosen, it seems clear that healthcare is being transformed through information and knowledge management and technology is being used to “tame data and transform information”(Berner,1999). Randall Tobias – former VP of ATT - Computer has virtually unlimited capacity for processing and storage of data - Human has limited storage9memory and processing power, but does have judgement, experience and intuition. Three main purposes of a DSS: 1. Assist in problem solving with semi structured problems 2. Support, not replace, the judgment of a manager or clinician 3. Improve the effectiveness of the decision-making process Early Systems Focus on Diagnosis Early known CDSS developed by de Dombal in 1972 at Leeds University Used Bayesian theory to predict the probability that a given patient, based on symptoms, had one of seven possible conditions 1974 – INTERNIST – Developed at the University of Pittsburgh to support the diagnostic process in general internal medicine by linking diseases with symptoms - Later became the basis of successor systems including quick medical reference (QMR) 1976 – MYCIN – rule-based expert system to diagnose and recommend treatment for certain blood infections In nursing, TWO early and well known systems a) COMMES ( Creighton online multiple modular expert systems) b) CANDI (Computer aided nursing diagnosis and intervention - Were developed to assist nurses with care planning and nursing diagnosis ADMINISTRATIVE and ORGANIZATIONAL SYSTEMS INTEGRATED SYSTEMS • Shortliffe – uses function, mode of advice, consultation style, underlying decision-science methodology, and user-computer interactions to categorize systems • Teich and Wrinn – examine DSS from the aspects of functional and logical classes and structural elements • • • • • Feedback provided Organizational of the data The extent of proactive information provided Intelligent actions of the system Communication method • • • • • • • • • • • • Substitute therapy alerts Drug family checking Structure entry Consequent actions Parameter checking Redundant utilization checking Relevant information display Time-based checks Templates and order sets Profile display and analysis Rule-based event detection Aggregate data trending • • • • • • • • Triggering Dispatching Rule logic Process control Notification / acknowledgements Action choices Action execution Rule editor Perreault – organized key CDSS functions as: 1) Administrative – support for clinical coding and documentation 2) Management of clinical complexity and details – keeping patients on research and chemotherapy protocols, tracking orders, referrals, follow-up, and preventive care 3) Cost control – monitoring medication orders and avoiding duplicate or unnecessary tests 4) Decision support – supporting clinical diagnostic and treatment plan processes promotion of best practices, use of condition-specific guidelines, and population-based management a. Data-based (population-based) b. Model-based (case-based) c. Knowledge-based (rule-based) d. Graphics-based systems A. Data-based systems – capitalized on the fundamental input into any intelligent system, data - Provide decision support OLAP – on line analytic processing B. Model-based DSSs – driven by access to and manipulation of a statistical, optimization, and/or stimulation model Model – generalization that can be used to describe the relationships among a number of observations to represent a perception of how things fit together Genetic algorithms (Gas) and neural networks (NNs) – newer computation techniques that are involving problems solving solutions Knowledge-based systems – rely on expert knowledge that is either embedded in the system or accessible from another source and uses some type of knowledge acquisition process to understand and capture the cognitive processes of healthcare providers EBP – evidence based practice D. Graphics-based systems – take advantage of the user interface to support the decisions by providing decision “cues” to the user in the form of color, graphical presentation options, and data visualization C. DTL – useful for specific straightforward tasks RBL – allows for complex decision capacities - More flexible with answers. Provides consistent outcomes and is adaptable to change - Also tends to have rigid solutions and allows little or no clinician autonomy Taxonomy for CDSS: 1. Context 2. Knowledge and data sources 3. Workflow 4. Decision support 5. Information delivery Institute of Medicine (IOM) – human error as a major source of patient care morbidity and mortality • Bates – practice lags behind knowledge by several years - This lag could be shortened if not eliminated by the availability of current knowledge to support decision-making process • Henry – identified essential elements needed for informatics infrastructure: Sittig – cites the following FIVE Elements: 1. 2. 3. 4. 5. Integrated real-time patient database Data-drive mechanism Knowledge engineer Time-driven mechanism Long-term clinical data repository Knowledge engineering – field concerned with knowledge acquisition and the organization and structure of that knowledge within a computer system Interviews – MOST COMMON used method of eliciting knowledge Cognitive Task Analysis (CTA) – set of methods that attempt to capture the skills, knowledge, and processing ability of experts in dealing with complex tasks • GOAL of CTA: Tap into these “higher order” cognitive functions • Tan and Sheps – six-step approach to CTA • Increasing Inclusion of Patients – CDSS allow patient access to the knowledge base of the system • Dual Purpose of Documentation – balance the use of poorly designed or inadequately tested systems with individual clinicians being forced to make patient care decision-making without existing evidence at the point of care • Dual Purpose: 1. Improving care for the individual patient 2. Improving care for the future populations of patients via aggregated information used for clinical decision-making • CDSS can: o Improve patient care quality o Reduce medication errors o Minimize variances in care o Improve guideline compliance o Promote cost savings