MICR 201 Microbiology for - Cal State LA
advertisement

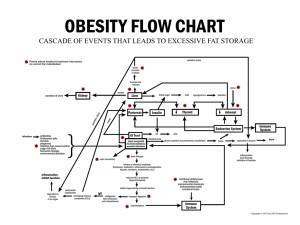
Microbiology- a clinical approach by Anthony Strelkauskas et al. 2010 Chapter 17: Failures of the immune response Chapters 14, 15, 16, 17 (up to HIV) Multiple Choice, T/F; 25 questions, 50 points Lecture, Chapter Questions Please bring Scantron, No. 2 pencil Host defense can be either inhibited or lost. ◦ When either happens, we don’t have the protection needed to survive the fight against microorganisms, be it primary pathogens or opportunists. ◦ Recurrent infections develop leading to premature death. The immune system can also turn on the host and cause damage. ◦ This happens in autoimmune diseases and hypersensitivities. (inherited) There are several reasons why host defense does not function properly or is absent: Immune defenses are normal but pathogen outsmarts the host Too little immune response ◦ Acquired immune deficiencies HIV ◦ Inherited (genetic, primary) immune deficiencies Too much immune response ◦ Against self: autoimmune diseases ◦ Against a harmless antigen (allergen): hypersensitivity reactions Subversion of host defenses by pathogens allows the spread of the pathogen and develop disease. Pathogens use a variety of strategies for avoiding destruction. ◦ Antigenic variation: Influenza virus, Trypanosoma ◦ Latency: Herpes virus, Varizella-zoster virus ◦ Resistance to host defenses: Mycobacterium tuberculosis ◦ Suppression of the immune response: Haemophilus influenzae and Neisseria gonorrhoeae secreting IgA proteases “Pneumocystis pneumonia is almost exclusively limited to immunosuppression patients …The occurrence of this disease in these five previously healthy individuals is unusual…. The fact that these patients are homosexuals suggests an association between some aspects of a homosexual lifestyle or disease acquired through sexual contact.” ~1981 By 1992, AIDS was the major cause of death in individuals 25-44 years of age in the US. The World Health Organization (WHO) estimates that 20 million people have died of AIDS. More than 40 million are currently infected. ◦ 0.6% of 15 – 49 year olds in the US ◦ 25.9% of 15 – 49 year olds in Swaziland (http://apps.who.int/ghodata/?vid=360) Changes in the incidence rate of HIV infection, 2001 to 2009, selected countries Increasing > 25% Decreasing > 25% Stable No data http://www.unaids.org/documents/20101123_globalreport_em.pdf; page 17 Infection by HIV is rising more rapidly in Eastern Europe and central Asia. One-third of persons infected with AIDS are between the ages of 15 and 24. HIV-1 is seen throughout the world. HIV-2 is mostly seen in Africa. In 1982-83, a retrovirus was isolated from the blood of individuals by groups in Paris, France, and Maryland, US, lead by Luc Montagnier and Robert Gallo, respectively. ◦ The virus, subsequently named human immunodeficiency virus - type I (HIV-1), was demonstrated to be the cause of AIDS. Retrovirus: RNA virus that reverse transcribes RNA (copies its genome into DNA) Enveloped virus with protein spikes ◦ gp 120 ◦ gp 41 2 copies of RNA Reverse transcriptase Integrase Protease HIV uses two glycoproteins for attachment – gp120 and gp41. They bind receptors on helper (CD 4) T cells, dendritic cells, and macrophages. For infection to be successful, co-receptors are required. ◦ Chemokine receptors Mutations in these two receptors, among others, block infection. Transmission is primarily through sexual contact and infected blood. The efficiency of transfer is based on the concentration of viral particles. The highest viral loads are found in peripheral blood monocytes, blood plasma, and cerebrospinal fluid. Semen and genital secretions are also sources of infection. In the US, transmission is highest among homosexuals. World wide, transmission is highest among heterosexuals. Sexual activity is still the leading method of transmission. Intravenous drug abuse is the 2nd most common form of transmission. The virus can be transmitted across the placental barrier and via breast milk. HIV can enter into the lamina propria: ◦ Through direct access via needle stick injury or blood transfusion. ◦ When the mucosal epithelial cell layer is broken. The extrusion of the virus from infected cells can be observed in tissue cultures. © Dominika Rudnicka; Nathalie Sol-Foulon; Olivier Schwartz/ Institut Pasteur Cells of the mucosal immune system are prime targets for initial infection. ◦ Dendritic cells (DC) bind to the HIV-1 envelope proteins with high affinity. ◦ DC migrate then to the lymph nodes and hold the virus until susceptible T cells come along and are infected. Reverse transcription of HIV results in the copying of viral RNA to DNA. ◦ Reverse transcriptase has no proofreading ability. Many mutations occur. This accounts for the virus’s ability to escape drug therapy and rapidly develop resistance. Retroviruses can use viral enzyme integrase to integrate viral DNA into the host cell’s chromosome. T cell activation induces transcription of provirus Viral RNA is transcribed, proteins synthesized and assembled at the cytoplasmic membrane. Virus exits via budding. HIV infection has three phases: ◦ Acute phase non specific, lymphadenopathy and flu like symptoms, high viremia ◦ Asymptomatic phase gradual decline in CD4+ TH cells Viremia is predictor of how fast the disease progresses Virus population becomes more heterogenous ◦ Symptomatic phase CD4 + TH cell counts drop below 200/mL blood AIDS develops, opportunistic infections, cancer Viral replication increases Cancer Kaposi sarcoma Precancerous: hariy leukplakia Approximately 10% of HIV infections progress to AIDS in the first three years. More than 80% show signs of clinical disease within 10 years. The remaining 20% are free of disease for long periods – more than 20 years in some cases. A small percentage never move past the asymptomatic phase. HIV replicates best in activated T cells. ◦ The greater number of opportunistic infections, the greater the number of T cells activated. ◦ The more T cells activated, the larger the quantity of virus particles produced. ◦ The more virus particles, the more infected cells and so on. Currently, viral load is determined by PCR (polymerase chain reaction, molecular genetic techniques). The rate of HIV replication is astonishingly high. 1010 virions can be released in a single cycle of infection per infected cell per day. The estimated genetic diversity of HIV produced in a single infected person is greater than all the diversity seen in a worldwide epidemic of influenza. Antibody response usually occurs during the first few months of infection. ◦ It can be as quick as a few days after infection. Antibodies are produced in response to the infection but are unable to clear it. IgG is the dominant form of antibody in any HIV infection and is involved in: ◦ Neutralizing the virus ◦ Blocking viral receptors ◦ Promoting complement-mediated reactions. Antibody response is important in HIV diagnostic. ◦ ELISA and Western immunoblotting All infected individuals have a cellular adaptive response to AIDS. ◦ Cytotoxic T cells are programmed to recognize all HIV-1 proteins. The response does not control and defeat the infection and the reason for this is not known. Antibody detection ◦ Serum samples (ELISA for screening, Western immunblot for confirmation) ◦ Most recent development: OraQuick test detects the presence of HIV in saliva collected using a mouth swab. The test is designed to return a result within 20 to 40 minutes Virus detection by PCR Culture of the virus Lymphoid organs ◦ Lymphadenopathy destruction of lymphoid tissue Nervous system ◦ Sub-acute encephalitis and dementia Gastrointestinal tract ◦ Diarrhea and food malabsorption Other tissues ◦ Heart, lungs, kidneys, and joints can be affected A. B. C. D. E. Reverse transcription of HIV by integrase results in the copying of viral RNA to DNA. Viral DNA is then incorporated into the host cell’s chromosomal DNA. Viral RNA is transcribed, proteins synthesized and assembled at the cytoplasmic membrane. Virus exits via budding. All steps are correct. A. B. C. D. E. 2000 cells/mL 20 cells/mL 20000 cells/mL 200 cells/mL None of the above. A. B. C. D. E. CD4 molecule Chemokine coreceptor MHC II molecule gp41 None of the above. Too little immune response In primary immunodeficiency disease, the immune system does not function properly. Parts of the immune response are defective because of mutations. Primary immunodeficiency diseases present as recurrent overwhelming infections in young children. The type of recurrent infection indicates the type of primary immunodeficiency. Recurrent infections by pyogenic bacteria indicate: ◦ Defects in antibody production ◦ Defects in the complement system ◦ Defects in phagocytosis Recurrent fungal or viral infections suggest that the defect is in reactions mediated by T cells. B cells make antibodies. B cell defects result in lack of antibodies and severe and repeated infection with encapsulated bacteria. ◦ Without capsule-binding, the antibody opsonization defense is lost Example: X-linked agammaglobulinemia ◦ X-chromosome linked mutation ◦ B cell development arrested ◦ Only males are affected: no circulating B cells, no antibodies ◦ Can be treated with immunoglobulin injections T cells, in particular TH cells, are the generals of our immune defense. ◦ Stimulate macrophages ◦ Act on B cells to make antibodies other than IgM in particular IgG, an opsonin ◦ Control virus infections and tumors Defects in T cell function can result in severe combined immunodeficiency syndrome (SCID). ◦ X linked forms ◦ Autosomal forms Defects in the complement system can lead to an increase in the occurrence of infectious diseases. ◦ Pyogenic infections with defects at C3 or factors above C3 ◦ Neisseria infections with defects of C5 – C9 Defects in phagocytic cells can cause severe immunodeficiency. ◦ Total absence of neutrophils is lethal. ◦ Defects in oxidative burst: chronic granulomatous disease ◦ Defects in ability to exit from blood stream: leukocyte adhesion deficiency Dysfunctional neutrophils Infection with S. aureus ◦ Cannot produce oxidative burst Monocytes and macrophages are recruited and activated by T cells ◦ Granuloma like structures are formed ◦ Recurrent an severe infections with opportunistic pathogens and also primary pathogens http://www.springerimages.com/Images/MedicineA ndPublicHealth/2-AID1101-08-032 Too much immune response against self Normally, tolerance prevents the development of autoimmune diseases. ◦ Developing lymphocytes are tested for self reactivity and those lymphocytes that are self reactive are removed by apoptosis or permanently inactivated. ◦ Lymphocytes are primarily activated by sudden increases in antigen concentrations. ◦ Lymphocytes require co-stimulatory signals to become fully activated, the right antigen is not enough Autoimmune diseases are the consequence of a failure of tolerance. The immune system reacts against self components. It is impossible to rid the host of the self antigen. Once self reaction has been initiated it is perpetuated. ◦ ◦ ◦ ◦ The autoimmune response destroys host tissues. Tissue destruction frees up more self antigens. This causes production of more autoantibody. Which destroys more tissue. Some people are genetically predisposed to autoimmune disease. ◦ Defect in the lymphocyte screening program Drugs and toxins can cause autoimmunity. Infection can result in an autoimmune reaction. ◦ They can react with self antigens to form derivatives perceived as foreign or nonself. ◦ Inflammation leads to tissue destruction and provides co-stimulatory signals. ◦ Previously protected sites (brain, eyes, testis, ovaries) become exposed to lymphocytes and selfreactive lymphocytes can become activated. ◦ Cross reactive antibodies can be generated Autoimmune diseases vary in: ◦ Severity ◦ Effector mechanisms Autoantibodies Self reactive cytotoxic T cells ◦ The tissue affected Autoimmune diseases are divided into two types: ◦ Organ-specific – reaction against self is confined to certain organs Type 1 insulin-dependent diabetes ◦ Systemic autoimmunity – affects multiple organs Systemic lupus erythematosus Insulin Dependent Diabetes Mellitus (IDDM) Early, sudden onset (adolescence) Initially mediated by autoantibodies against b-cell antigen Later phases include cytotoxic T-cell response Immunohistochemistry Insulin = brown Glucagon = black Normal IDDM Auto-antibodies against nuclear components (DNA, histones, etc) Immune complexes activate complement Complexes transported via on phagocytes or on erythrocytes to spleen/liver for sequestration Excess complexes are deposited in small blood vessels Local inflammation in skin, joints and kidneys, multi-organ damage May lead to activation of self reactive T lymphocytes Too much immune response against harmless antigen An allergic reaction is a form of immune response. ◦ “Too much against a harmless antigen” ◦ It is not usually life-threatening. ◦ It can produce serious tissue injury, even death. Allergic responses are the result of a person becoming hypersensitized. There are four main types of hypersensitivity reaction: ◦ Type I hypersensitivity (allergic rhinitis, conjunctivitis, asthma) ◦ Type II hypersensitivity (drug allergies, thrombocytopenic purpura) ◦ Type III hypersensitivity (serum sickness) ◦ Type IV hypersensitivity (tuberculin test -TH cell mediated; poison ivy contact dermatitis- CTL mediated) Antibody Cell Type I (“Allergy”) Type II (drug allergies, thrombocytopenic purpura) Soluble antigen: IgE: Mastcells Immediate-type Atopy: Exaggerated tendency to mount an IgE response Cell associated antigen: IgG: phagocytes, NK cells Type III (serum sickness) Type IV (tuberculin test, poison ivy contact dermatitis) Soluble antigen Antigen-Antibody complexes T-cell mediated Occurs when the immunoglobulin IgE responds to antigens called allergens. ◦ Most human allergies are caused by inhaling small, water-soluble proteins carried on pollen grains or dust-mite feces. Occurs when the immunoglobulin IgE responds to antigens called allergens. ◦ Most human allergies are caused by inhaling small, watersoluble proteins carried on pollen grains or dust-mite feces. Allergens trigger activation of IgE-binding cells. Upon allergen binding these cells degranulate and release huge amounts of bioactive molecules ◦ Mast cells ◦ Basophils ◦ ◦ ◦ ◦ ◦ Histamine Enzymes Leukotrienes IL4 Chemokines Clinical effects vary according to the site of mast cell Eosinophils have two functions in allergic reactions: ◦ Release highly toxic granules and free radicals. They normally kill microorganisms. They cause significant tissue damage in allergic reactions. ◦ Produce chemical mediators, prostaglandins, leukotrienes, and cytokines. This enhances and amplifies the allergic reaction. Immediate reaction ◦ Histamine mediated ◦ Smooth muscle contraction ◦ Vascular endothelial cell leakage Late phase reaction (8 – 12 h) ◦ Chemokine, cytokine, leukotriene, and enzyme mediated ◦ Sustained edema ◦ Cell influx ◦ Tissue remodeling Exaggerated tendency to mount an IgE response to environmental allergens Individuals affected are called atopic. ◦ They have higher levels of eosinophils. ◦ They are more susceptible to allergic diseases. ◦ Susceptibility may be genetic. Allergen can be deposited directly into the blood or rapidly absorbed causing systemic anaphylaxis. ◦ ◦ ◦ ◦ Widespread increase in vascular permeability Catastrophic loss of blood pressure Airway constriction Swelling of the epiglottis The reaction is known as anaphylactic shock and is potentially fatal. ◦ It requires immediate injection of epinephrine. Both environmental and inherited factors are important Environment: Susceptibility genes for asthma ◦ Exposure to infectious agents in early childhood drives a TH1 response ◦ Too hygienic environment with too little infectious agents drive a TH2 response ◦ Diet ◦ IL4, IL4 receptor ◦ High affinity IgE receptor ◦ MHC II Allergies!! Less allergies!! Drug associated Drug (e.g., penicillin) binds to platelets Big enough to be seen by immune system Antibodies made and bind to drug-platelet complex Macrophages take up complex or complement becomes activated and attacks membrane of platelets Platelet numbers decrease Spontaneous bleeding occurs Cell infiltrate!! Lipid soluble allergen is absorbed through skin and crosses cell membranes Allergen modifies self peptides Presentation of modified self peptide via MHC I to CTL Destruction of modified cell The immune system can break down and in some cases fail. It can also turn against the host. There are three ways the adaptive immune response can fail: viral infection (HIV) leading to AIDS, subversion of the immune response by pathogens, and genetic immunodeficiency. Autoimmune disease occurs when the adaptive immune response attacks the host. HIV is a latent virus that carries the enzyme reverse transcriptase. This enzyme allows the viral RNA to be converted to DNA, which can integrate into a host cell chromosome. There are three strategies that are used to subvert or defeat the host defense: antigenic variation, resistance to host defense, and suppression of the immune response. Resistance to host defense can involve several mechanisms, including the inhibition of phagocytosis. Primary immunodeficiency involves genetic abnormalities. Tolerance to self antigens prevents the development of autoimmune disease. Specialized regulatory T cells (T reg cells) control the development of an autoimmune response. Autoimmunity can be organ-specific or systemic. An allergic response is a type of immune response against antigens that are referred to as allergens. There are four types of hypersensitivity response.