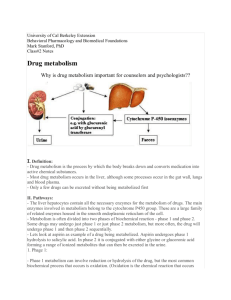
First pass effect

Chapter 2. Metabolism and Elimination
A. Liver is the primary site of drug metabolism.
First pass effect (or first pass metabolism) : metabolism of a drug or other xenobiotic during the absorption process.
Typically in the liver or gastrointestinal tract after oral administration.
The liver is a metabolic machine and often inactivates drugs on their way from the GI tract to the body.
Some drugs (e.g. nitroglycerin) are not given orally but by alternative route.
B. Metabolism can change a drug in several ways
1. The polarity is usually increased , enhancing the water solubility and renal excretion of the drug metabolite.
2. The activity of the drug is reduced . Exceptions are the prodrugs , which are drugs that are inactive in the form administered but are metabolized to their active forms.
Other examples of bioactivation: prontosil/sulfanilamide ; methanol/formaldehyde , salicin/salicylic acid--aspirin
Bonus-Credit for work out the detail reaction mechanism
3. Drug metabolites usually have smaller V d
( apparent volume of distribution) dose (mg)
V d
= plasma concentration at equilibrium (mg/ml)
All biotransformation reactions can be assigned to one of two major categories called phase I and II reactions
C. Phase 1 reactions are nonsynthetic .
1. Oxidation by mixed function oxidases (MFO) [also known as cytochrome P-450s, microsomal enzymes, mono-oxygenases] occurs in the smooth endoplasmic reticulum (ER). Important exception (see below).
a. NADPH, cytochrome P-450 reductase, and O
Drug +NADPH +H + +O
2
2 are required.
Drug-O+NADP + + H
2
O b. Many reactions can be produced, including:
(1) hydroxylation
(2) dealkylation
(3) deamination
(4) sulfoxidation
(5) oxidation
2. Reductions
3. Hydrolysis
Ethanol and caffeine metabolized by enzyme present in soluble fraction
Examples of oxidative reaction
Examples of reduction reactions
Examples of hydrolysis reactions
D. Phase 2 reactions are conjugative (synthetic).
1. Glucuronidation occurs in the ER. Glucose is used to form uridine diphosphate glucuronic acid (UDPGA) which then transfers a glucuronide to the drug in the presence of glucuronyl transferase.
2. Other substances can also be conjugated (by transferases) to drugs, thereby reducing the drug activity, including : a. sulfate b. acetyl c. methyl d. glutathione e. amino acids, especially glycine
E. Factors affecting drug metabolism.
1. Enzyme induction . Some drugs (e.g. barbiturates, phenytoin, rifampin, warfarin, alcohol) and pollutants (e.g. cigarette smoke) increase the activity of drug-metabolizing enzymes. Enzyme induced include: MFOs, glucuronyl transferase, the steroid metabolizing system. This induction hastens the metabolism of the inducing drug and many other drugs.
self-induction, cross-induction. case 1: coumadin (anticlotting drug) / phenobarbital
(sedative/hypnotic drug) case 2: diphenylhydantoin (antiepilepsy drug)/ steroids (birth control)
2. Enzyme inhibition . It can occur by decreased synthesis of enzymes, increased degradation of the enzyme, or competition of two or more drugs for the same binding site. For example, cimetidine inhibits the metabolism of several potentially toxic drugs including phenytoin, warfarin and theophylline.
( Enzyme inhibition cont .)
-Liver cirrhosis, hepatotoxicants e.g. CCl
4
, toluene
-Virus infections, influenza A or adenovirus, may affect the metabolism of theophylline (bronchodilator) case in 1980 in Seattle
3. Genetic polymorphisms . The response to drugs varies between individuals. Usually the variation shows the Gaussian distribution, however, some drug responses show discontinuous variation. For example, hepatic N-acetylase displays genetic polymorphism. About 50% of the population acetylate isoniazid (an anti- T.B. drug) rapidly, while the other
50% acetylate it slowly.
4. Age . Babies and the elderly show reduced hepatic metabolism of drugs and the reduced renal mechanisms as well.
II. Excretion of drugs and drug metabolites
A.The kidney is the primary organ that excretes drugs and drug metabolites.
1. Even when the drug is excreted in the unmetabolized form, the kidney also decreases the pharmacological activity.
2. Polar drugs and polar drug metabolites are readily eliminated by the kidney.
Nephron , the functional unit of kidney, approx. 1.2 million units in each man
Proximal tubule
Glomeruls
, to retain plasma proteins
Glomerular filtration
Cardiac output to kidney 20% approx. 1200 ml/min, I.e. expose to 650 ml of plasma per min; normal rate of plasma filtration 125 ml/min (the glomerular filtration rate) , the filration rate is plasma drug concentration independent less than 50 kd molecules pass through
Serum creatinine is an indicator
B. Filtration of the unbound molecule accounts for the excretion of most drugs
1. Drug bound by plasma proteins will not be filtered by the glomerulus .
2. Hydrophilic or lipophobic substances are most efficiently eliminated by kidney, because they are not readily reaborbed across the nephron tubule after they are filtered.
3. If a drug is a weak base, administration of ammonium chloride will acidify the urine and increase the amount of the base that is in the ionized form.
a.The excretion of the weak base will be increased.
b.This will be most effective if the pK a physiological pH.
of the drug is near the
C. Active transport of a few drugs occurs in the proximal tubule.
1. It usually involves secretion of strong acids or strong bases.
2. Characteristics of active transport are: a. competition between substrates for the carrier b. saturation of the carrier c. being unaffected by plasma protein binding
3. Active reabsorption can also occur.
4. A few substances are both actively secreted and actively reabsorbed (e.g. uric acid, aspirin).
Blood vessel
Tubular secretion
– Active transport, energy dependent secretory process.
– is plasma drug concentration dependent
– is subjected to competition for transporter, e.g. penicillin secretion can be interfered by the co-administration of probenecid
(analgesic, anti-gout)
Re-absorption
– is a passive process dependent on the lipid solubility, pKa, pH, urine flow rate.
–
The effect of urinary pH: In case of phenobarbital ( a weak acid) overdose the urine can be alkalinized by sodium bicarbonate; Conversely, ammonium chloride is used to acidify urine to increase the excretion of basic drugs
D. Biliary excretion occurs in the liver
1. Large polar compounds, often conjugated metabolites, are actively excreted into the bile . important for elimination of compounds with a molecular weight >500
2. Enterohepatic cycling occurs with a few drugs that are eliminated in the bile, reabsorbed from the intestine, returned to the liver and again eliminated in the bile.
liver small intestine
a. glucuronidase in the intestine can cleave off the glucuronide, so the free drug can be reabsorbed.
b. Digitoxin, a cardiac glycoside, undergoes enterohepatic cycling.
c. This may increase the half-life of the drug.
Lung
1. the primary site of elimination for gaseous anesthetics and volatile compounds.
2. ethanol : 90% metabolized in liver, 2% via lungs equilibrium partition for ethanol between blood and alveloar air is approx. 2100:1;
Thus, [ethanol] in blood = 2100 x [ethanol] in end-expiratory air