Glycolysis
advertisement

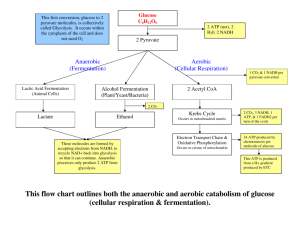
Glycolysis and Gluconeogenesis Alice Skoumalová 1. Glycolysis Glucose: the universal fuel for human cells Sources: diet (the major sugar in our diet) internal glycogen stores blood (glucose homeostasis) Glucose oxidation: after a meal: almost all tissues during fasting: brain, erythrocytes Glycolysis: oxidation and cleavage of glucose ATP generation (with and without oxygen) all cells in the cytosol (the reducing equivalents are transferred to the electron-transport chain by the shuttle) ATP is generated: 1. via substrate-level phosphorylation 2. from NADH 3. from oxidation of pyruvate Regulation of glycolysis: 1. Hexokinase 2. Phosphofructokinase 3. Pyruvate Kinase Generation of precursors for biosynthesis: fatty acids amino acids ribosis-5-P Anaerobic glycolysis a limited supply of O2 no mitochondria increased demands for ATP Lactic acidemia in hypoxia Phosphorylation of glucose: irreversible Glucose 6-P: cannot be transported back across the plasma membrane a precursor for many pathways that uses glucose Hexokinases Glucokinase (liver, β-cell of the pancreas) high Km Michaelis-Menten kinetics 1. Conversion of glucose 6-P to the triose phosphates 2. Oxidation and substrate-level phosphorylation 1. Conversion of glucose 6-P to the triose phosphates essential for the subsequent cleavage • irreversible • regulation 2. Oxidation and substrate-level phosphorylation Substrate-level phophorylation Substrate-level phophorylation Summary of the glycolytic pathway: Glucosis + 2 NAD+ + 2 Pi + 2 ADP 2 pyruvate + 2 NADH + 4 H+ + 2 ATP + 2 H2O ∆G0´ = - 22 kcal (it cannot be reversed without the expenditure of energy!) Clinical correlations: Hypoxemia (lack of oxygen in tissues) Acute hemorrhage (hypotension, lost of erythrocytes) - anaerobic glycolysis - lactate formation, metabolic acidosis Chronic obstructive pulmonary disease (an insuficient ventilation) - anaerobic glycolysis, lactate formation, metabolic acidosis - accumulation of CO2, respiratory acidosis Myocardial infarction (lack of oxygen in myocardium) - anaerobic glycolysis, lactate formation - lack of ATP Aerobic glycolysis: involving shuttles that transfer reducing equivalents across the mitochondrial membrane Glycerol 3-phosphate shuttle: Malate-aspartate shuttle: Anaerobic glycolysis: dissociation and formation of H+ Energy yield 2 mol of ATP Major tissues of lactate production: (in a resting state) Daily lactate production 115 (g/d) Erythrocytes 29 Skin 20 Brain 17 Sceletal muscle 16 Renal medulla 15 Intestinal mucosa 8 Other tissues 10 Cori cycle: Lactate can be further metabolized by: heart, sceletal muscle Lactate dehydrogenase: a tetramer (subunits M and H) Lactate dehydrogenase Pyruvate + NADH + H+ LD lactate + NAD+ 5 isoenzymes: Heart (lactate) Muscle (pyruvate) Biosynthetic functions of glycolysis: Clinical correlations: Long-intensity exercise (for example a sprint) - the need for ATP exceeds the capacity of the mitochondria for oxidative phosphorylation, anaerobic glycolysis → lactate formation, muscle fatigue and pain - a training → the amounts of mitochondria and myoglobin increase Regulation • tissue-specific isoenzymes (low Km, a high afinity) • glucokinase (high Km) • the rate-limiting, allosteric enzyme • tissue-specific isoenzymes Fructose 2,6-bis-phosphate: is not an intermediate of glycolysis! Phosphofructokinase-2: inhibited through phosphorylation - cAMP-dependent protein kinase (inhibition of glycolysis during fasting-glucagon) the liver isoenzyme - inhibition by cAMP-dependent protein kinase (inhibition of glycolysis during fasting) Lactic acidemia: increased NADH/NAD+ ratio inhibition of pyruvate dehydrogenase 2. Gluconeogenesis Gluconeogenesis: synthesis of glucose from noncarbohydrate precursors → to maintain blood glucose levels during fasting liver, kidney fasting, prolonged exercise, a highprotein diet, stress Specific pathways: 1. Pyruvate → Phosphoenolpyruvate 2. Fructose-1,6-P → Fructose-6-P 3. Glucose-6-P → Glucose Precursors for gluconeogenesis 1. lactate (anaerobic glycolysis) 2. amino acids (muscle proteins) 3. glycerol (adipose tissue) Conversion of pyruvate to phosphoenolpyruvate 1. Pyruvate → Oxaloacetate Pyruvate carboxylase 2. Oxaloacetate → PEP Phosphoenolpyruvatecarboxykinase Conversion of phosphoenolpyruvate to glucose 3. Fructose-1,6-P → Fructose-6-P Fructose 1,6-bisphosphatase (cytosol) 4. Glucose-6-P → Glucose Glucose 6-phosphatase (ER) Clinical correlations: Alcoholism - excessive ethanol consumption → increase NADH/NAD+ ratio that drive the lactate dehydrogenase reaction toward lactate - lack of precursors for gluconeogenesis → its inhibition - insuficient diet - reduced glucose in the blood, consumption of glycogen in the liver → hypoglycemia Regulation of gluconeogenesis: concomitant inactivation of the glycolytic enzymes and activation of the enzymes of gluconeogenesis 1. Pyruvate → PEP Phosphoenolpyruvate carboxykinase induced by glucagon, epinephrine, and cortisol 2. Fructose 1,6-P → Fructose 6-P Fructose 1,6-bisphosphatase - inhibited by fructose 2,6-P 3. Glucose 6-P → Glucose Glucose 6-phosphatase - induced during fasting Summary Glycolysis • Generation of ATP (with or without oxygen) • The role of glycolysis in different tissues • Lactate production • Regulation Gluconeogenesis • Activation during fasting, prolonged exercise, after a highprotein diet • Precursors: lactate, glycerol, amino acids • 3 key reactions: Pyruvate → PEP Fructose-1,6-P→ Fructose-6-P Glucose-6-P → Glucose • Regulation Pictures used in the presentation: Marks´ Basic Medical Biochemistry, A Clinical Approach, third edition, 2009 (M. Lieberman, A.D. Marks)