Primer on Opportunistic Infections
advertisement

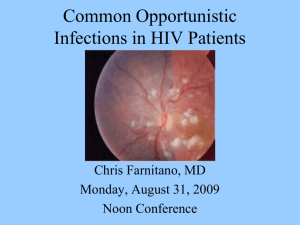
Common Opportunistic Infections in HIV Patients, Part 2 Chris Farnitano, MD Thursday, October 8, 2009 Noon Conference Objectives Discuss most common opportunistic infections (OIs): Dx and Rx Discuss immune reconstitution disease Review primary OI prophylaxis Forms Case Study SP 27 yo male seen in clinic in June 2009 Meds: unboosted atazanavir + Truvada since 1/09; ranitidine T cells 5; viral load 30,000 Why is his anti-HIV cocktail failing? Case Study SP Ritonavir added to boost atazanavir Patient instructed to take ranitidine in AM only and antivirals in PM Blood Cx for AFB, HIV genotype ordered Case Study SP Admitted to Kaiser August, 2009 with diffuse warm, tender lymphadenopathy Biopsy performed, read as suspicious for lymphoma Transferred to CCRMC after 7 days on clarithromycin, ethambutol, rifabutin T Cells 209, viral load 726 What is patient’s diagnosis? What are the most common OI’s? Cohort Studies in pre-triple therapy era: Candida Pneumocystis Carinii Cytomegalovirus Mycobacterium Avium Complex Pneumocystis - second episode Toxoplasmi gondii Herpes zoster Causes of death, PHC HIV clinic 2007-9 RH: Crypto meningitis TW: street drug overdose SA: sepsis, pneumonia and massive hemoptysis DW: metastatic prostate ca RP: CVA, laryngeal ca VA: PML (progressive multifocal leukencephalopathy) AM: bacterial pneumonia, ETOH cirrhosis, wasting OIs diagnosed, PHC HIV clinic 2005-9 PCP pneumonia Esophageal Candidiasis Herpes Simplex Herpes Zoster M. Kansasii immune reconstitution pneumonia Mycobacterium Avium Complex (MAC) Cryptococcal Fungemia, meningitis Histoplasmosis PML Effect of HAART on Opportunistic Infection Incidence Most OI’s have declined 80-90% OI’s seen now mostly in 3 groups undiagnosed HIV+ not in care or not adhering to therapy long time “battle-scarred warriors” failing after a long history of multiple regimens 50-200 T Cells: Pneumocystis Carinii Pnuemonia Toxoplasmosis Cryptococcus Toxoplasmosis <50 T Cells CMV Retinitis Mycobacterium Avium Complex Cryptosporidiosis Progressive Multifocal Leukencephalopathy PML Ockham's razor does not apply for advanced AIDS -often multiple diagnoses present simultaneously ie PCP, CMV, KS, Cocci 12% of bacterial pneumonias also have PCP 10% of PCP pneumonia complicated by bacterial infection search for second etiology if patient not improving Immune reconstitution diseases (HAART attacks) MAC adenitis CMV TB PCP Case Study SP Diagnosis: Immune Reconsitution MAC AFB blood culture from June grew out MAC on 8/12 (hospital day #13) Also: Perianal herpes Squamous cell carcinoma-in-situ, buttock Vancomycin-resistant enterococcus, groin Primary OI prophylaxis PCP -T cells <200 or thrush Toxo -T cells <100 and +Toxo titer MAC - Tcells <50 TB – INH x 9 months if PPD >5mm or quantiferon-TB positive Toxo prophylaxis Septra SS or DS qd or DS TIW Septra Desensitisation: 1cc qd x 3d, then 2cc qd x 3d, then 5ccqd x 3d, then one SS tab qd Dapsone 100mg qd +pyramethamine 50mg qweek + leukovorin 25mg qweek Atovaquone 1500mg qd MAC prophylaxis Zithromax 600mg x 2 tabs qweek reduces infection rate 59% Also seems to reduce risk of PCP Cytomegalovirus Retinitis Who Gets It? Rare above 50 T Cells Reactivation disease: most HIV patients CMV IgG+ (90% of gay HIV+ men) 90% of CMV disease is retinitis Cytomegalovirus Retinitis Symptoms painless, progressive visual loss unilateral blurry vision floaters Cytomegalovirus Retinitis Signs coalescing white perivascular exudates surrounded by hemorrhage brushfire pattern or tomato and cheese pizza Cytomegalovirus Retinitis Cytomegalovirus Retinitis Cytomegalovirus Retinitis Diagnosis if you suspect it, obtain ophthalmologist confirmation within 24-48 hrs. Cytomegalovirus Retinitis Treatment Valgancyclovir 900mg PO BID x 21 days, then qd Adverse effects: neutropenia ANC<500 in 15% thrombocytopenia anemia 50%: nausea, vomiting, abdominal pain or diarrhea Gangcyclivir intraocular implant Consider in addition to systemic therapy: Surgically implanted depo device Effective for 6 months Replace at 6 months if still not immune reconstituted Consider for sight threatening lesions near the central visual field Mycobacterium avium Complex - Who gets it? T Cells <50 screen with blood culture for AFB x 1 q 3 months to detect subclinical disease Mycobacterium avium Complex - Symptoms fever, night sweats weight loss diarrhea Mycobacterium avium Complex - Signs anemia Neutropenia Fever Diarrhea wasting Mycobacterium avium Complex - Diagnosis Blood culture usually positive if symptomatic but takes weeks to grow If need to know sooner then do bone marrow Bx Positive sputum culture usually colonization, not active disease Positive stool culture may be colonization, not active disease, mucosal bx more indicative of disease MAC-filled macrophages in spleen Mycobacterium avium Complex - Treatment Clarithromycin 500mg BID + Ethambutol 15mg/kg/d +/- Rifabutin 300mg qd Treatment failure rate is high without immune reconstitution drug toxicity development of resistance Case Study SP After 4 months of anti-MAC therapy + potent anti-HIV therapy: T Cells 71 viral load <48 Patient still hospitalized Large effusions persist Dubhoff tube required for feeding Diffuse chest/abdominal adenopathy persists MAC Cx’s show partial/complete resistance to all MAC drugs except clofazamine Prognosis? Forms Summary: Pyramid approach Prophylaxis simple: Septra and Zithromax Rule out TB in pneumonia with T Cells <200 Avoid treating PCP empirically An ounce of prevention pills is worth a pound of Treatment pills An ounce of prevention pills is worth a pound of Treatment pills