Primer on Opportunistic Infections
advertisement

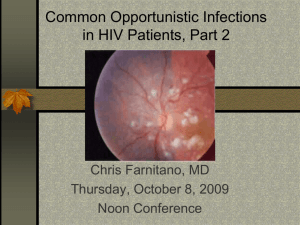
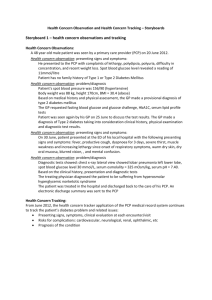
Common Opportunistic Infections in HIV Patients Chris Farnitano, MD Monday, August 31, 2009 Noon Conference Objectives • Discuss most common opportunistic infections (OIs): Dx and Rx • Discuss immune reconstitution disease • Review primary OI prophylaxis Forms What are the most common OI’s? • Cohort Studies in pre-triple therapy era: – – – – – – – Candida Pneumocystis Carinii Cytomegalovirus Mycobacterium Avium Complex Pneumocystis - second episode Toxoplasmi gondii Herpes zoster Causes of death, PHC HIV clinic • 2007-9 – – – – – – – RH: Crypto meningitis TW: street drug overdose SA: sepsis, pneumonia and massive hemoptysis DW: metastatic prostate ca RP: CVA, laryngeal ca VA: PML (progressive multifocal leukencephalopathy) AM: bacterial pneumonia, ETOH cirrhosis, wasting OIs diagnosed, PHC HIV clinic • 2005-9 – – – – – – – – – PCP pneumonia Esophageal Candidiasis Herpes Simplex Herpes Zoster M. Kansasii immune reconstitution pneumonia Mycobacterium Avium Complex (MAC) Cryptococcal Fungemia, meningitis Histoplasmosis PML Effect of HAART on Opportunistic Infection Incidence • Most OI’s have declined 80-90% • OI’s seen now mostly in 3 groups – undiagnosed HIV+ – not in care or not adhering to therapy – long time “battle-scarred warriors” failing after a long history of multiple regimens More people living with AIDS Pyramid or iceberg model Strata of Pyramid • • • • >350 T Cells 350-200 50-200 <50 >350 T Cells • Increased incidence of diseases that also affect normal hosts: – – – – Recurrent Vaginal Candidiasis Pulmonary Tuberculosis Pnuemococcal Pneumonia Cervical Dysplasia Pulmonary TB 200-350 T Cells: • Herpes Simplex • Herpes Zoster • Thrush Herpes Zoster (Shingles) 50-200 T Cells: • Pneumocystis Carinii Pnuemonia • Toxoplasmosis • Cryptococcus Toxoplasmosis <50 T Cells • • • • CMV Retinitis Mycobacterium Avium Complex Cryptosporidiosis Progressive Multifocal Leukencephalopathy PML Ockham's razor does not apply for advanced AIDS • -often multiple diagnoses present simultaneously – ie PCP, CMV, KS, Cocci – 12% of bacterial pneumonias also have PCP – 10% of PCP pneumonia complicated by bacterial infection – search for second etiology if patient not improving Immune reconstitution diseases (HAART attacks) • • • • MAC adenitis CMV TB PCP Primary OI prophylaxis • • • • PCP -T cells <200 or thrush Toxo -T cells <100 and +Toxo titer MAC - Tcells <50 TB – INH x 9 months if PPD >5mm or quantiferon-TB positive Quantiferon vs. TST in HIV patients • Quantiferon not approved for use in immunocomprimised • 147 HIV patients in New Orleans given both tests: – – – – 36% did not return for TST reading 15 positive by quantiferon 1 positive by TST Quantiferon is more sensitive but without a gold standard for latent TB infection cannot say whether it is more or less specific • Another study showed similar positive test result rates but a better correlation with risk factors for quantiferon vs. TST suggesting quantiferon is a more specific test Quantiferon vs. TST in HIV patients • “Given the high risk for progression to active disease in HIV-infected persons, any HIVinfected person with reactivity on any of the current LTBI diagnostic tests should be considered infected with M. tuberculosis” • ----CDC guidelines, 3/24/09 PCP Prophylaxis • Septra SS or DS qd or DS TIW – Single strength has similar efficacy with fewer adverse reactions (I.e. late onset rash, hepatotoxicity, fever) – 25-50% of AIDS pts. D/c Septra DS due to reactions • Septra Desensitization: – 1cc qd x 3d, then 2cc qd x 3d, then 5ccqd x 3d, then one SS tab qd • Dapsone 100mg qd +pyramethamine 50mg qweek + leukovorin 25mg qweek • Aerosolized pentamadine 300mg q month • Atavaquone 1500mg qd Aerosolized pentamidine booth Toxo prophylaxis • Septra SS or DS qd or DS TIW • Septra Desensitisation: – 1cc qd x 3d, then 2cc qd x 3d, then 5ccqd x 3d, then one SS tab qd • Dapsone 100mg qd +pyramethamine 50mg qweek + leukovorin 25mg qweek • Atovaquone 1500mg qd MAC prophylaxis • Zithromax 600mg x 2 tabs qweek reduces infection rate 59% • Also seems to reduce risk of PCP Specific Opportunistic Infections Case Study: HW • 51 yo male with poor adherence to meds • HIV + since at least 1996 • 1st episode thrush March,2005 – – – – C/o dry mouth Exam: white patches on buccal mucosa T Cells 54 Treated with fluconazole, sx resolve Case Study: HW • Recurrent thrush July, 2005 – Fluconazole again prescribed • September, 2005 – – – – C/o odynophagia Dx: probably esophageal candidiasis Fluconazole again prescribed Sx resolve in 3 days Case Study: HW • Recurrent odynophagia January, 2006 – Switched to itraconazole liquid – 3 weeks later: • odynophagia resolved • Thrush persists, resolved on re-exam March, 2006 • August, 2006-March, 2007 – Recurrent episodes of thrush and esophageal candidiasis due to non-adherence to intraconazole – Each episode improves when patient is adherent Case Study: HW • April, 2007 – Persistent thrush despite stated adherence – Switched to Voriconazole – Sx resolve November, 2007 T Cells 5 Weight 121# (baseline 198#) -recurrent odynophagia despite adherence to voriconazole Admitted for IV Capsofungin Sx markedly improve in 24 hours Fungal Cx: Candida Albicans Sensitivities: resistant to fluconazole, itraconazole and voriconazole Case Study: HW • December 2007-August 2008 – Persistent extensive thrush – Continued on Voriconazole – T cells 54 -> 12 August 2008: moves in with sisters after hospital stay, adherence improves markedly January 2009: T cells 77, thrush much improved April, 2009: T cells 239, thrush resolved Candida • • • • Thrush Angular Chelitis Vaginal Candidiasis Esophageal Candidiasis Thrush • • • • cottage cheese plaques soft palate, buccal mucosa, tonsils can be removed with a tongue blade also erythematous form without exudate Thrush Angular chelitis • • • • pain fissures erythema difficulty opening mouth Angular Chelitis Recurrent Vaginal Candidiasis • less frequent than you would expect, unless T Cells<100 • can use Fluconazole 200mg qweek for suppression Esophageal Candidiasis • odynophagia • usually also has thrush (positive predictive value is 90%, but 18% of esophageal candidiasis presents without thrush) • Treat empirically x 5-7 days • if not better, scope to r/o other causes: – CMV, HSV, idopathic esophageal ulcers, lymphoma • Secondary prophylaxis needed Esophageal Candidiasis Treatment: • Fluconazole 100-200mg qd until sx resolve • Alternatives for resistant Candida: – – – – – Higher dose fluconazole (400-800 mg/d Itraconazole Voriconazole IV Capsofungin IV Amphotericin PCP - Who gets it: • Septra prophylaxis highly efficatious • Risk if T Cells <200 or thrush PCP - Symptoms • insidious onset – 2-4 weeks of progressive symptoms • Fever, sweats, weight loss, fatigue, nonproductive cough • progressive dyspnea • retrosternal discomfort PCP - Signs • Lung exam usually normal • CXR: bilateral diffuse interstitial infiltrate in 80-90% • LDH>400 in 62% • PO2<75 in 66% PCP Pneumonia Severe PCP • PCP - Diagnosis • Induced sputum x 3 in early AM (all on same day): 50-70% sensitive • Bronchoscopy (+/-Bx): 80-90% sensitive • PCR based tests • To collect sputums or go directly to bronch? PCP - Treatment • Can begin before Dx confirmed without affecting diagnostic yield • Prednisone 40mg BID x 5d. Then taper over total 21d. • Septra 15mgTMP/kg/d IV div. Q8h x 21d. – Switch to po when improved • give first dose prednisone 15-30 minutes before Septra Approach to HIV patient with Pneumonia • What is the T Cell Count? T cell Count >200: • TB presents in typical fashion – cavitary in 50-60% – isolate only if CXR suspicious for TB • Opportunistic infections unlikely – can treat empirically for bacterial infection – S. pneumoniae, H. Flu most common (encapsulated) • Also consider: Non-Hodgkin’s Lymphoma T cell Count <200: • TB presents as lower lobe disease, adenopathy, miliary or interstitial pattern – cavitary in only 29% – isolate all abnormal CXR until TB ruled out • Opportunistic infections likely – obtain definitive diagnosis whenever possible – Coccidiomycosis, Cryptococcus, Aspergillis – CMV, KS, M.TB, M. Kansasii Don’t Treat PCP empirically • experienced physicians make wrong clinical diagnosis in 20% of suspected PCP • patients treated empirically have higher risk of death than patients who underwent bronch • High incidence of rash toward end of 21 d. Septra course • Adjunctive steroids may exacerbate other OIs • Many etiologies left uncovered Cytomegalovirus Retinitis - Who Gets It? • Rare above 50 T Cells • Reactivation disease: most HIV patients CMV IgG+ (90% of gay HIV+ men) • 90% of CMV disease is retinitis Cytomegalovirus Retinitis Symptoms • painless, progressive visual loss • unilateral blurry vision • floaters Cytomegalovirus Retinitis Signs • coalescing white perivascular exudates • surrounded by hemorrhage • brushfire pattern or tomato and cheese pizza Cytomegalovirus Retinitis Cytomegalovirus Retinitis Cytomegalovirus Retinitis Diagnosis • if you suspect it, obtain ophthalmologist confirmation within 24-48 hrs. Cytomegalovirus Retinitis Treatment • Valgancyclovir 900mg PO BID x 21 days, then qd • Adverse effects: – – – – neutropenia ANC<500 in 15% thrombocytopenia anemia 50%: nausea, vomiting, abdominal pain or diarrhea Gangcyclivir intraocular implant • Consider in addition to systemic therapy: – Surgically implanted depo device – Effective for 6 months – Replace at 6 months if still not immune reconstituted – Consider for sight threatening lesions near the central visual field Mycobacterium avium Complex Who gets it? • T Cells <50 • screen with blood culture for AFB x 1 q 3 months to detect subclinical disease Mycobacterium avium Complex Symptoms • fever, night sweats • weight loss • diarrhea Mycobacterium avium Complex Signs • anemia • neutropenia Mycobacterium avium Complex Diagnosis • Blood culture usually positive if symptomatic but takes weeks to grow • If need to know sooner then do bone marrow Bx • Positive sputum culture usually colonization, not active disease • Positive stool culture may be colonization, not active disease MAC-filled macrophages in spleen Mycobacterium avium Complex Treatment • • • • Clarithromycin 500mg BID + Ethambutol 15mg/kg/d +/Rifabutin 300mg qd Treatment failure rate is high without immune reconstitution – drug toxicity – development of resistance Forms Summary: • Pyramid approach • Prophylaxis simple: Septra and Zithromax • Rule out TB in pneumonia with T Cells <200 • Avoid treating PCP empirically • An ounce of prevention pills is worth a pound of Treatment pills An ounce of prevention pills is worth a pound of Treatment pills