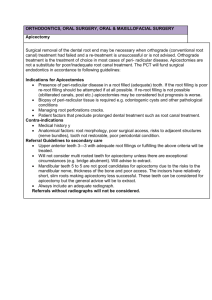
Restoration of Endodontically Treated Teeth
advertisement

Restoration of Endodontically Treated Teeth Post and Core System Characteristics of endodontically treated teeth 1. 2. 3. 4. 5. Tooth structure loss by: i. Caries, trauma, erosion, abrasion, attrition. ii. Previous restorations and recurrent caries under restorations. iii. Endodontic treatment; due to removal of coronal and intraradicular Dentine during access and root canal preparation. Micro cracks in remaining tooth structure produced by endodontic procedures. Weakened collagen intermolecular cross-links of Dentine lower shear strength. Dehydration; non-vital teeth have less moisture content than vital teeth. Esthetics; biochemically altered Dentine modifies light refraction through the tooth and modifies its appearance. The combined result of these changes are: increased fracture susceptibility and decreased translucency. Treatment planning for non-vital teeth 1. Pretreatment Evaluation: i. ii. iii. Quality of the endodontic treatment Periodontal condition Restorative evaluation i. ii. iii. iv. iv. Strategic importance Anatomic position of the tooth The amount of remaining coronal tooth structure The functional load on the tooth esthetic evaluation 2. Treatment plan: i. ii. iii. Post Core Definitive restoration Treatment planning for non-vital teeth 1. Pretreatment Evaluation: i. ii. Quality of the endodontic treatment: • The endodontic treatment should be properly done. • Retreatment should be considered if tooth exhibits any clinical signs of inflammation, a periapical pathology exists, or inappropriate endodontic filling material was used ( silver pointes). Periodontal condition: • This is important for long-term success of teeth. • Weak teeth should be extracted. • A mutilated tooth in which the restorative treatment would violate the junctional epithelium or the attachment level (e.g. extensive caries, perforations, external root resorption) should be considered for crown- lengthening surgery or orthodontic extrusion. iii. Restorative evaluation: a. Strategic importance: • does the final restoration depends on this tooth ? Are the adjacent teeth reliable? What about an implant ? b. Anatomic position of the tooth: • Anterior teeth: • They receive mainly angular forces reinforcement effect of posts is doubtful. • If the tooth is intact except for the endodontic access opening etched resin in the access is sufficient. • A post and core is only indicated when the tooth is weakened by the presence of large or multiple coronal restorations or they require form or/and color changes that cannot be affected by bleaching, resin bonding or laminate veneers. • Mandibular incisors and maxillary lateral incisors usually require a post. • Maxillary central incisors and canines crown preparation, the remaining tooth structure, is accomplished before deciding a post should be placed. • Posterior teeth: • They receive mainly vertical forces. • When there is sufficient tooth structure to retain a core and crown posts are not needed. • Teeth which don’t have occlusal interdigitation or have an bucco-occlusal form that preclude interdigitation ( e.g. Mandibular 1st premolars with small poorly developed lingual cusps) , with sufficient coronal tooth structure, restoration of the access should be acceptable. • Teeth which have interdigitation with opposing teeth full coverage crowns or onlays should be used as occlusal forces push the cusps apart. • Maxillary premolars are subjected to angular and vertical forces if the clinical crown length > its cervical width a post may be indicated. c. d. The amount of remaining coronal tooth structure: • More than half conservative treatment with coronal restorations without posts. • minimal post, core, and definitive restoration. The functional load on the tooth: • The post, core, and crown system is indicated, when more extensive protective and retentive features are required in the restoration: 1) Bruxism and heavy occlusion. 2) Abutment teeth for long-span fixed bridges. 3) Abutment teeth for free end removable partial denture. iv. esthetic evaluation: • Esthetic zone (Anterior teeth, premolars, and often 1st molar) requires: 1) Careful selection of restorative materials. 2) Careful handling of the tissues. 3) Timely endodontic intervention to prevent darkening of the root as it looses vitality. 2. Treatment plan: (post and core) • 1) 2) 3) 4) 5) The purpose of a post is to provide retention for a core; as both laboratory and clinical data fail to provide definitive support for the concept that posts strengthen endodontically treated teeth. • If the walls of the root are thin owing to removal of internal root caries or over-instrumentation during post preparation then a post may strengthen the tooth. • Reinforcement of a tooth by a post means: moving the point of fracture from the gingival margin of the crown some distance up the root towards the root apex. • The following characteristics should be determined prior to beginning the clinical procedures : Post length Post diameter Type of post and core that will be used (prefabricated post and restorative material core or anatomically customized cast post and core) Root selection in multi-rooted teeth Core material and definitive restoration. 1) Post Length: • It is of more importance for retention than diameter. • 4 - 5 mm of gutta-percha should be retained apically to ensure a good seal. • posts should be extended to that length, or equivalent to the crown length, in all teeth except molars. • With molars, posts should not be extended more than 7 mm from the orifice of root canal in the base of the pulp chamber. Extension beyond this length can lead to root perforation or only very thin areas of remaining tooth structure. • Posts should extend 4 mm apical to the bone crest to decrease stress in dentine and in the posts. 2) • • • • • • • • Post Diameter: It is important to resist distortion or permanent bending under functional forces. Ideally, after completion of endodontic treatment, the canal shouldn’t be further enlarged. Rather, the post should be modified to fit the canal. Do not exceed one-third the root diameter. Optimal post diameter measurements have been determined to be: 1) Mandibular incisors 0.6 – 0.7 mm 2) Maxillary central incisors, canines, and the palatal root of the maxillary 1st molar 1.0 – 1.2 mm & may even reach 1.7 mm. 3) The rest of teeth 0.8 mm. Mesial roots of mandibular molars and the buccal roots of maxillary molars shouldn’t be used for posts. Mandibular premolars with oval or ribbon shaped canals shouldn’t be prepared further for a post the gap is filled with luting cement which add elasticity to it. Roots with remaining dentine thickness less than 1mm are indicated For custom made posts. The amount of remaining intraradicular dentine after endodontic treatment: • Canines, maxillary incisors, and the palatal root of maxillary 1st molar = > 1mm. • All other teeth = < 1mm. N.B Craze Lines: Craze lines in dentin are areas of weakness where further crack propagation may result in root fracture and tooth loss. The patient should be informed of their presence. If possible, avoid post placement in favor of a restorative material core. If a post is required, it should passively fit the canal, and the definitive restoration should entirely encompass the cracked area, whenever possible, by forming a ferrule. 3) Type of post: A. Acc. to type of material: • Metallic. • Non-metallic: 1. Carbon fiber posts: composed of unidirectional carbon fibers in an epoxy matrix. Esthetic version contains quartz. It is smooth, rigid, highly radiopaque, and can be removed. 2. Ceramic posts: composed of zirconium dioxide. It is hard and can withstand high flexural stresses. 3. Fiber-reinforced posts: composed of woven polyethylene fiber ribbon that is coated with a dentine bonding agent and packed into the canal, when it is light cured. It is esthetic, smooth, less stiff, reduce incidence of root fracture, and less radiopaque. • Excessive retention of zirconia (ceramic) posts may preclude conventional endodontic retreatment if cannot be removed atraumatically. • Carbon fiber and Fiber-reinforced posts may not need to be as long as traditional posts. A 1:1 ratio between the post and the crown is sufficient. • In laboratory tests metallic posts are more fracture resistant than carbon fiber posts. • Most metal, carbon fiber, and ceramic posts chemically bond to resin cement. • Stainless steel posts are more retentive to composite cores than carbon fiber posts. • Carbon fiber and Fiber-reinforced posts have a lower modulus of elasticity than metal posts and are considered to have elasticity similar to dentine, this provide more force dissipation, reducing the risk of root fracture. • Stainless steel contains nickel which may cause allergy. Non-metallic posts are highly biocompatible. • Prefabricated Stainless steel posts may show corrosion. Custom-cast and non-metallic posts don’t show corrosion. B. C. Acc. to retention: • Active: include many designs (e.g. threaded, split threaded). they produce high stresses which increase the potential for vertical fracture. They should be unscrewed one fourth of a turn after installation. Split threaded posts even produces higher stresses. Active posts are indicated in short canals. • Passive: it is cemented to the root canal using zinc phosphate, glass ionomer, or a resin cement. Resin modified glass ionomer is not indicated as hygroscopic expansion may cause root fracture. Low expansion formulations of resin modified glass ionomer can be used. Acc. to fabrication: • Pre-fabricated post: • tapered smooth, se , or threaded. • parallel smooth, se , or threaded • Custom-cast post: • indicated in: i. Non-rounded root canals. ii. Extremely divergent sidewalls of root canals. • • • • • • Tapered smooth posts are the least retentive. And may cause wedging effect on the tooth. Tapered threaded posts are more retentive than parallel threaded. Parallel posts distribute stresses less evenly and cause apical stress concentration. Tapered posts cause post-core junction stress concentration and equal stress distribution between the cementoenamel junction and the apex. So , it should be considered for teeth that have thin apex. Tapered posts require no further canal preparation after endodontic treatment as it can be modified to fit into the canal. So, it can be used in thin fragile roots. Venting and surface roughness are important features which should be added to custom-cast posts. 4) Root selection in multi-rooted teeth posts are best placed in (the primary roots) in palatal roots of maxillary molars distal roots of mandibular molars, they are the. The buccal roots of maxillary molars and the mesial root of mandibular molars should be avoided if at all possible. If these roots must be used in addition to the primary roots, then the post length should be short (3 to 4 mm) and a small-diameter instrument should be used (no larger than a No. 2 Peeso instrument, which is 1.0 mm in diameter). Use cast interlocking post: It is two pieces, characterized by depressions parallel to the sidewalls of other canal. The distal post is put first then the other will interlock with it finally. Technical procedure for prefabricated posts Pattern construction of custom-cast post I. 1. 2. 1) 2) 3) 4) 5) 6) Direct method • Material: A. Wax. B. Self cure A.R. C. Plastic ready-made burn out post. • Steps: Lubrication of root canal (die lubricant). If direct wax pattern: Select a metallic sprue former: Fits loosely inside R.C. Length > than that of core. Serrated using diamond stone or disc (to ensure good retention bet. wax & sprue). Softening of blue casting wax and insertion into the R.C. Heating of sprue. Wait till hardening of wax. Add for any deficiencies until it’s removed with slight resistance “snugly fit”. Core can be made of wax, followed by investing and casting. 6) If direct A.R. pattern: Select a plastic dowel: Fits loosely inside R.C Long. Serrated (notched). Mixing of A.R. and insertion into the R.C. before the dough stage. Before complete curing, moisten the dowel with monomer and insert into R.C. Also before complete curing, move the plastic dowel inward and outwards to prevent interlocking in any undercuts or roughness. Add any modifications until it’s removed with slight resistance “snugly fit”. Investing and casting. 4. 1) 2) 3) 4) Plastic ready made burnout post: Plastic posts supplied with its special drills (same size & shape). Prepare root canal. Build up core with wax or acrylic resin. Investing and casting. 3. 1) 2) 3) 4) 5) II. 1. - - Indirect method: Steps: Impression: By light body elastomer applied by a syringe, starting from apex. Insert an st.steel wire to: 1- support imp. Material. 2- prevent imp. tearing during removal. Use a (Cu band) or (tray) to complete impression procedures. Remove the impression and evaluate it, then pour a stone cast. Thank you